Background
Improving outpatient (OP) efficiency and service structure is of paramount importance as the NHS seeks to manage ever increasing demand in the wake of the COVID-19 pandemic. As we re-establish services and attempt to clear the backlog, new ways of managing current workload, in addition to future referrals, need to be considered.
Recent Getting it Right First Time (GIRFT) reports including Urology: The Path to Recovery (https://gettingitrightfirsttime.co.uk/wp-content/uploads/2022/05/Urology_2022-05-10_Framework_GIRFT-Urology-Strategic-Framework-Manual.pdf) have highlighted the importance of streamlining referral pathways, increasing one-stop OP service usage, and improving the interface with primary care towards our recovery. Accordingly, ‘intelligent triage’ offers considerable benefit.
Within the Mid-Yorkshire Hospitals (MYHT) and Barnsley (BHNHSFT) Urology Area Network (UAN), intelligent triage encompasses a series of activities undertaken by five triaging consultants managing all non-2WW referrals coming into the department:
- Responding to advice and guidance requests (AAG) from primary care.
- Triaging electronic referrals (e-RS) into the appropriate outpatient clinic (OPC) slot.
- Ensuring appropriate pre-clinic investigations are requested.
- Reviewing all internal requests for an OP appointment.
- Responding to written expedite requests for referrals already present within the system.
To effectively undertake this work, the triage team interrogate available patient clinical records allowing appropriate management of e-RS and internal secondary care referrals with AAG alone, with the aid of an AAG library for consistency. Four departmental Programmed Activities (PAs) are timetabled weekly for intelligent triage.
Our UAN with Barnsley was formed in October 2020, however electronic referral systems in Barnsley were not available to us until July 2021, seven months after our own service had been established. In addition, there are differences between the two trusts in the primary care commissioning for radiological investigation requests. These two factors affect the pre-OP management of certain patient referral groups for the Barnsley population.
Methods
An AAG document based on national clinical guidelines and best practice was generated by the triaging team to ensure a consistent approach between the team members.
Throughout the study period our clinical systems were under continuous development. By working closely together, the team were able to incorporate changes into the AAG protocols. This included changes allowing AAG requests from primary care to be directly amended to OP referrals, whereas they previously required a separate e-RS referral.
We prospectively reviewed 24 months of e-RS data from MYHT between December 2020 and December 2022, as well as 18 months of e-RS data from BHNHSFT. Referral number and rates for OP consultations at both sites were captured. BHNHSFT AAG request data was collected for the same period. AAG request data for MYH NHST was also obtained for a reduced period of 20 months. Both e-RS and AAG request data were analysed for total volume and conversion to OP consultations.
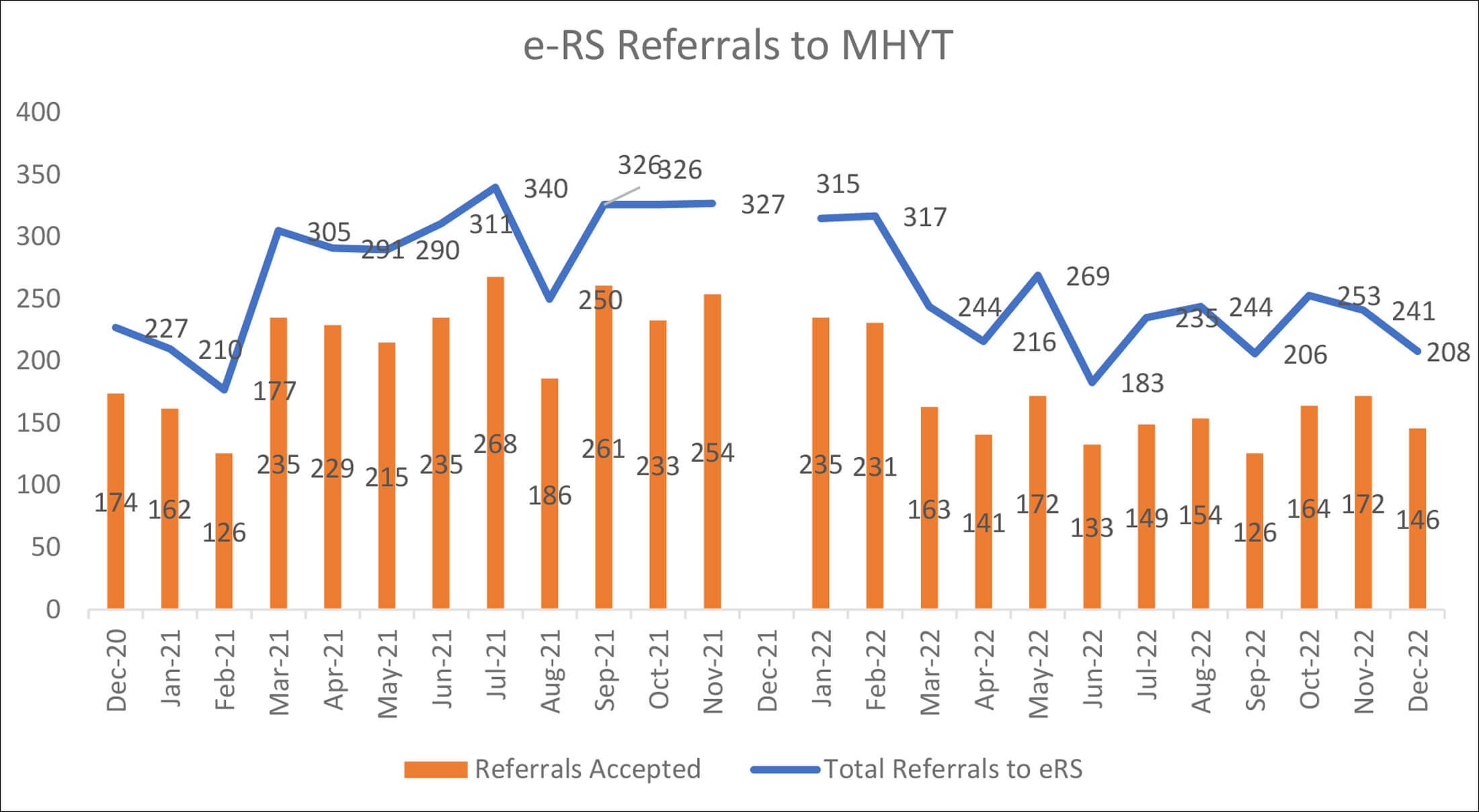
Figure 1: MYHT e-RS referrals total volume, with volume accepted for OPC appointment.
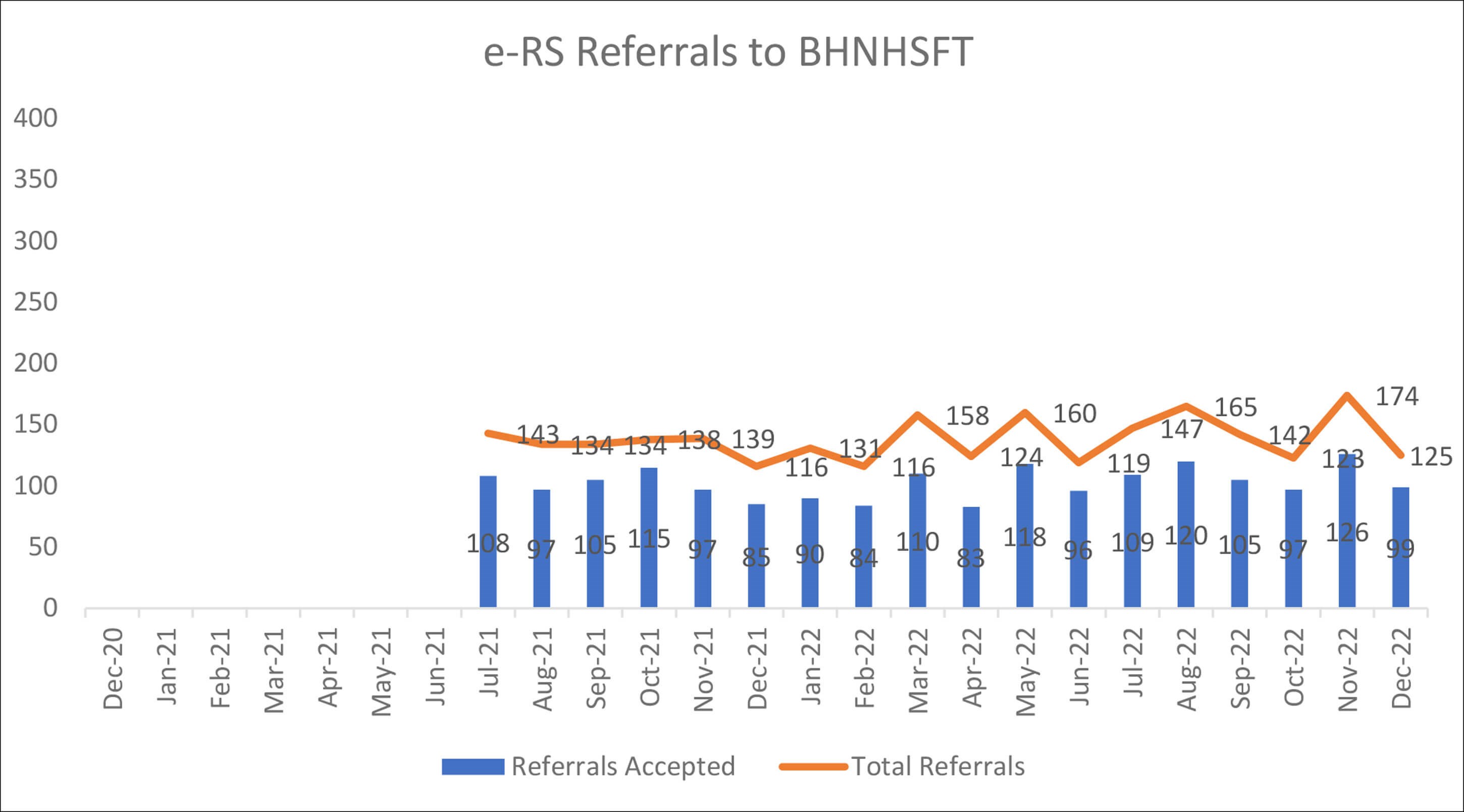
Figure 2: BHNHSFT e-RS referrals total volume, with volume accepted for OPC appointment.
Results
Monthly e-RS referrals were consistently higher at MYHT compared to BDGH in keeping with differing catchment population sizes. Twenty-four months of data collection were available from MYHT, with 18 months from BHNHSFT comprising 6311 and 2488 referrals respectively (Figure 1 & 2). Percentages of e-RS primary care referrals managed with AAG alone were similar across the UAN with 72.3% (4564) of MYHT, and 74.1% (1844) of BHNHSFT e-RS referrals resulting in OPC requirement (Figure 3).
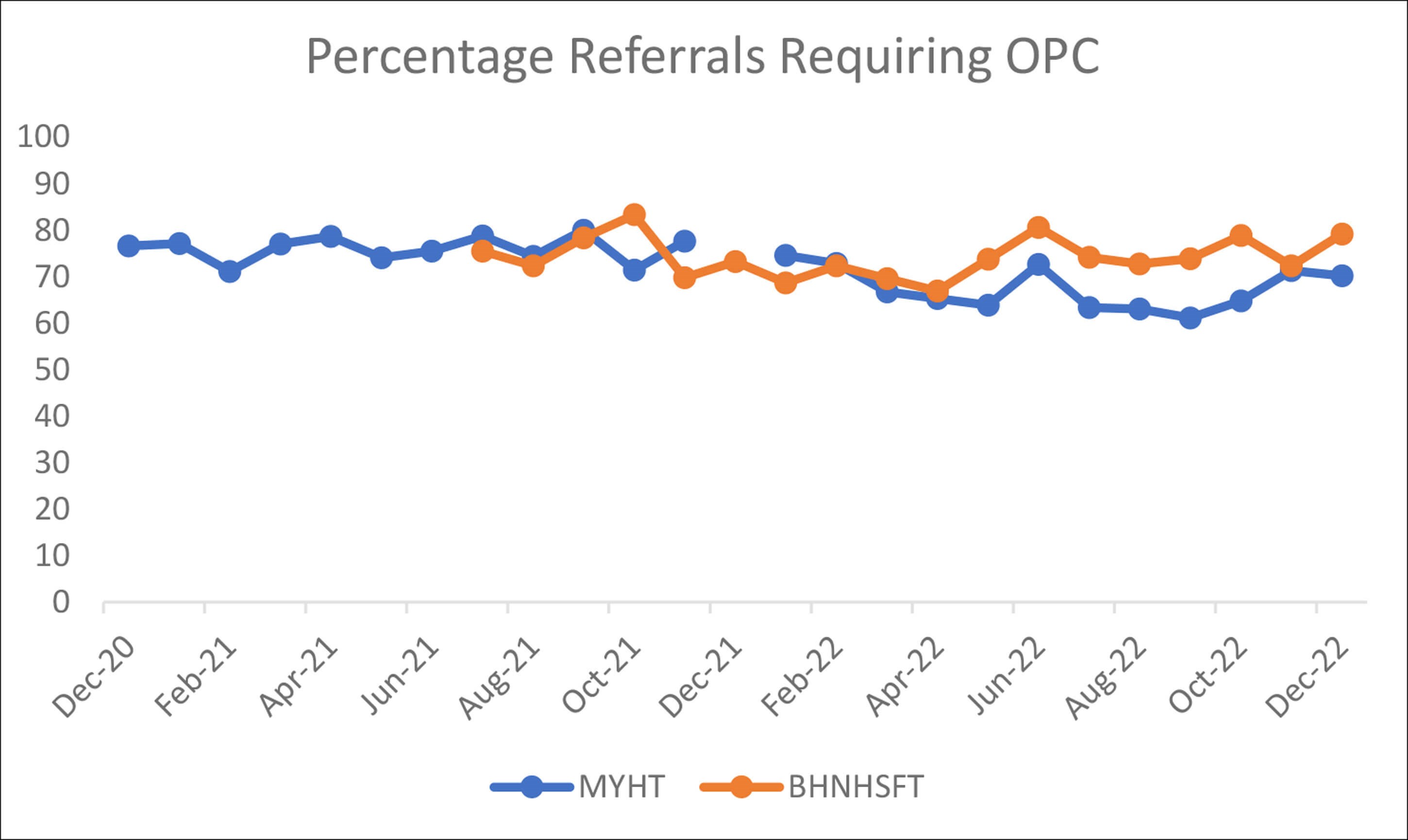
Figure 3: Comparison of MYHT and BHNHSFT referrals requiring OPC appointments.
Of 20 months data available within MYHT for AAG request acceptance rates 4781 were received; 1607 (33.6%) were converted to an OP attendance. In the initial 18 months after introduction at BDGH, 580 AAG requests were received, of which 136 (23.4%) required conversion for OP review.
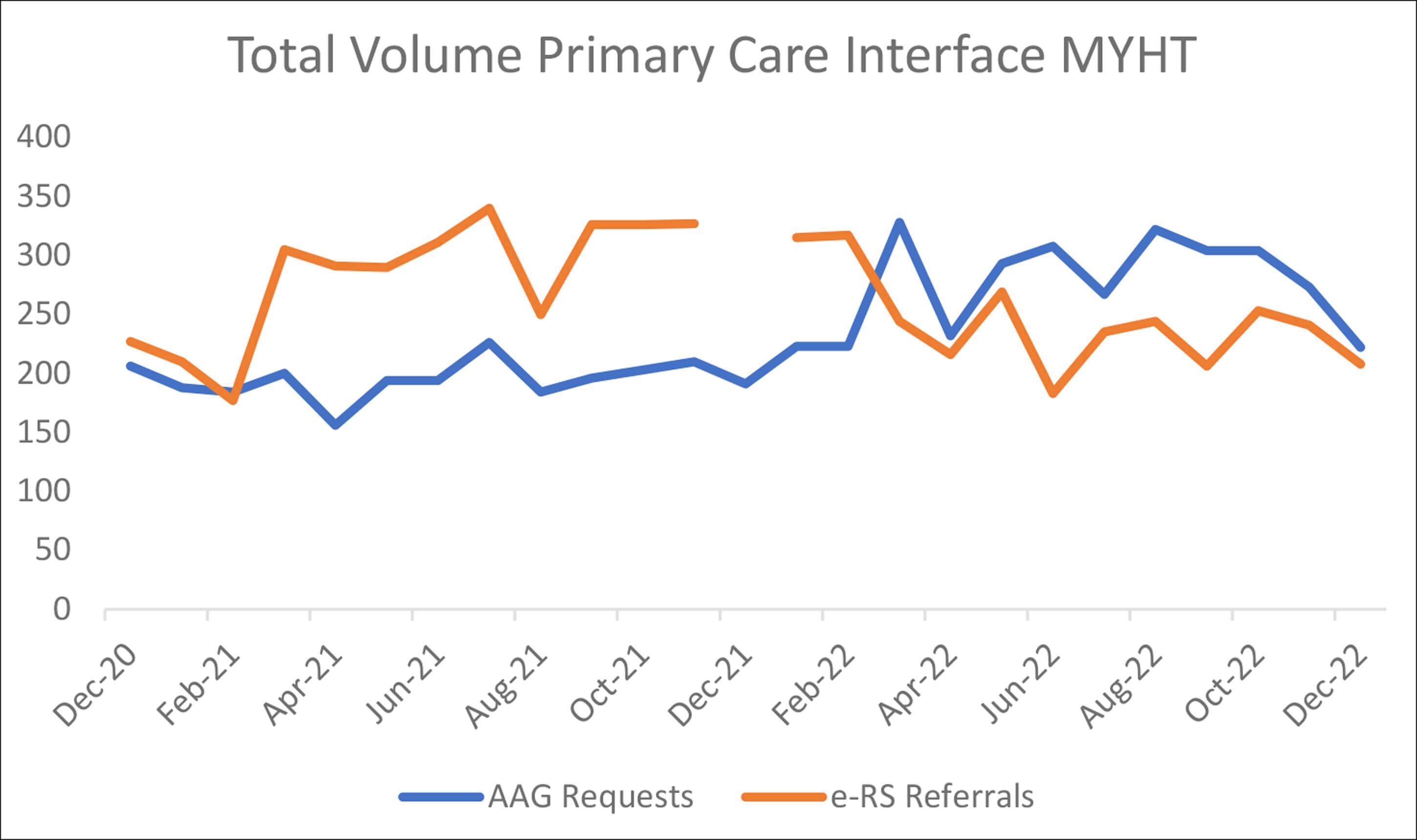
Figure 4: MYHT total monthly primary care interactions.
There is significantly more uptake from primary care of AAG requests within MYHT, with nearly half (47.2%) of all primary care interaction via AAG Requests (Figure 4). This contrasts with BHNHSFT services, where out of 3068 combined AAG requests and e-RS referrals, only 580 (18.9%) were AAG requests (Figure 5).
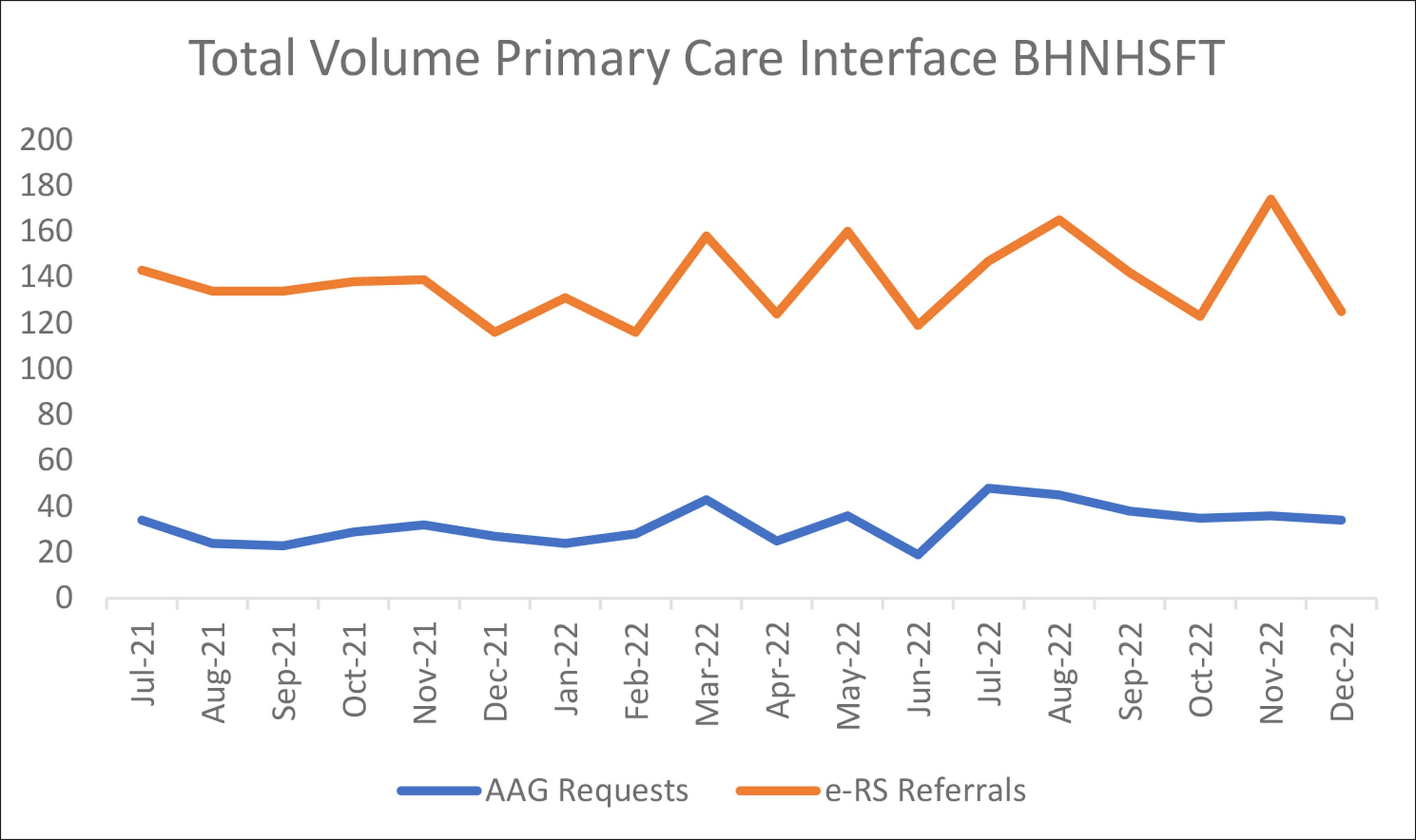
Figure 5: BHNHSFT total monthly primary care interactions.
Discussion
Using senior clinicians in intelligent triage ensures appropriate use of OP consultations, with over a quarter of e-RS referrals managed with AAG alone across the UAN. We note similar rates between trusts in managing primary care e-RS referrals with AAG alone, although differing use of our AAG services as a percentage of primary care interactions; this is likely related to variation in electronic pathway development between the trusts and differences in existing pathways across primary and secondary care across the UAN.
The reduction in e-RS referrals at MYHT from Spring 2022 coincides with increasing AAG request uptake. This is likely to be attributable to an improved AAG request system which allowed primary care to refer for OP attendance in addition to seeking advice within the same electronic system.
Whilst argument may be made for administrative staff fulfilling the triage role to free up consultants for direct clinical patient interaction, we feel algorithmic triaging is suboptimal for patient safety. Through use of dedicated resources and senior decision makers, we can provide timely, standardised AAG and accurately direct patients requiring secondary care review to the most appropriate clinic setting. Equally, this system enables over a quarter of patients to avoid a secondary care attendance altogether.
Patient safety is enhanced through red flag identification and appropriate timescales for OP review. Furthermore, it improves efficiency by allowing requisite pre-clinic investigations, and managements, to be in place by the time of OP review. Through use of this method, we are able to significantly free up our OP capacity to review appropriate referrals.
Our data highlights reproducibility in efficiency improvements between and established intelligent triage practice and newly established systems in other trusts or UANs. By continuing to develop standards and guidelines within the units, we are facilitating the development of further advancements with a move towards a full one stop service for new patients. A strong relationship with primary care colleagues is key.






