Case 1
A 48-year-old female, having previously had an augmentation ileocystoplasty 10 years ago, has been referred with right loin pain by the emergency department. A venous blood gas is performed shortly after triage with the following values:
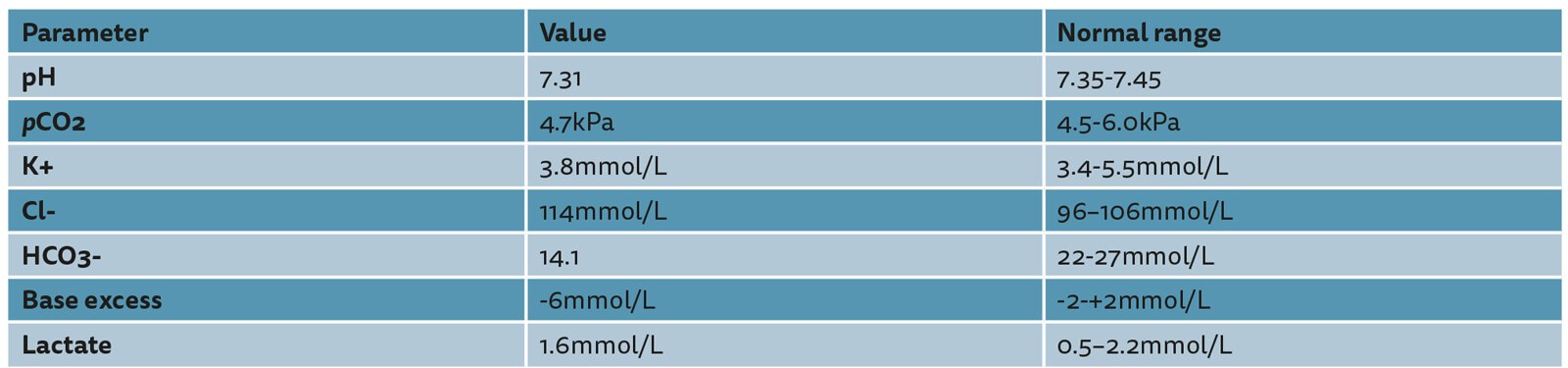
- What is the biochemical abnormality demonstrated?
- What is the mechanism of this?
- What is the other significant metabolic consequence as part of this abnormality?
- What other potential operations may this patient have had?
- What are the indications for augmentation cystoplasty?
- What potential issues secondary to this reconstructed urinary tract anatomy could this patient have to explain their symptoms?
- What segment of bowel is most commonly harvested and why?
- What other long-term complications may occur following this procedure?
Case 2
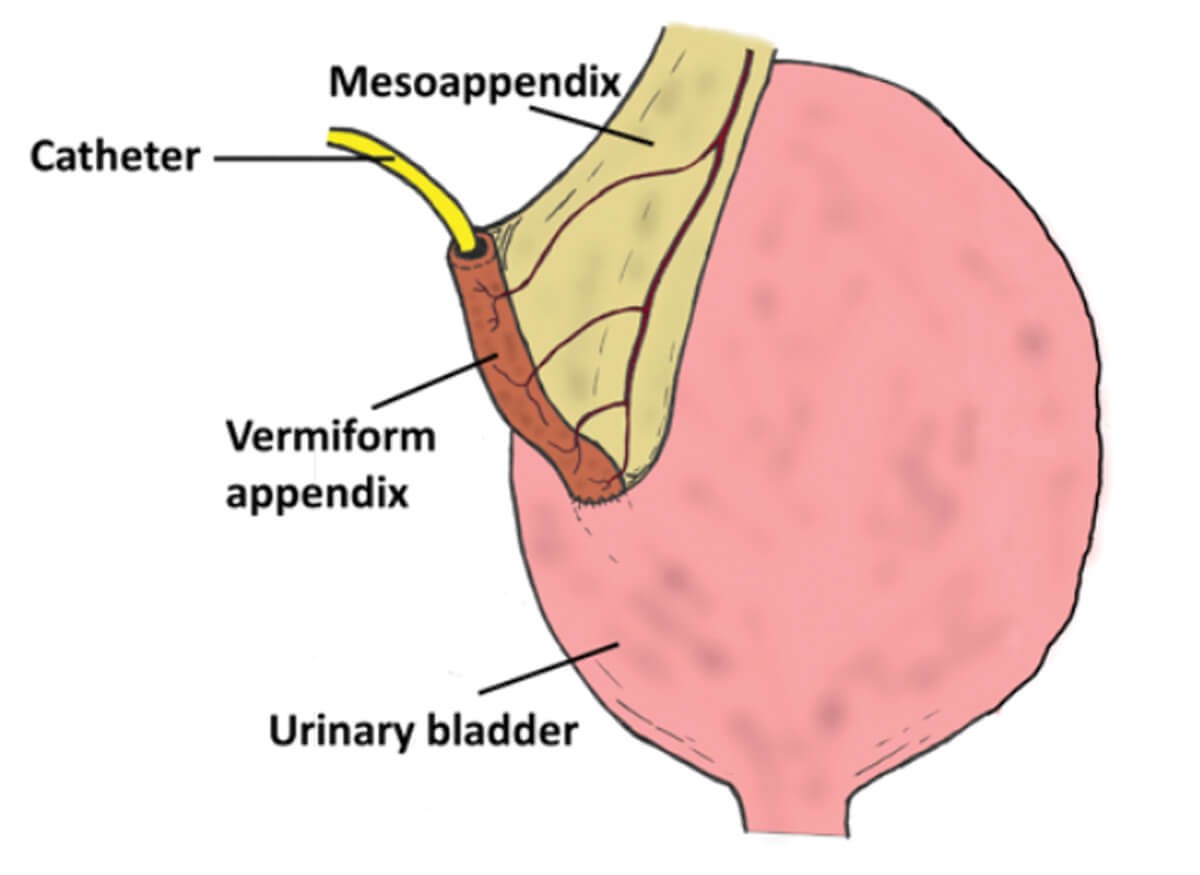
- What procedure is demonstrated in the figure and what is achieved by this operation?
- What alternative can be used instead of the vermiform appendix and what is this procedure commonly referred to as?
- What is the mechanism of continence from these procedures?
- If a patient has both an augmentation cystoplasty and the procedure demonstrated here, what additional procedure can be considered to achieve complete urinary continence?
- What are the indications for this operation?
Cystoplasty – answers
Case 1
- Hyperchloraemic metabolic acidosis.
- Ammonium and chloride ions are resorbed by the bowel segment, bicarbonate ions are secreted by the bowel segment and excreted in the urine.
- Bone mineral density decreases due to calcium carbonate being mobilised out of bone stores to buffer the acidosis.
- Cystectomy and ileal conduit, cystectomy with ileal bladder substitution.
- Idiopathic overactive bladder, neurogenic lower urinary tract dysfunction, fibrosing bladder pathologies (such as tuberculosis, schistosomiasis, and ketamine bladder syndrome).
- Possibilities include an ascending urinary tract infection or obstructing stone. Although unlikely, delayed spontaneous bladder perforation is an important differential to consider but is unusual so long after the initial surgery; it is more likely to present with generalised abdominal pain secondary to peritonitis as opposed to presenting with loin pain, and the venous lactate, although not diagnostic, is not suggestive of perforation. It is also important to consider a non-urological cause such as a biliary, bowel or gynaecological pathology.
- Ileum 25-40cm distal to the ileocaecal valve. Used because it is relatively easy to handle, has fewer complications than the alternatives, and malabsorption is minimised at this point.
- Malignant changes – most commonly adenocarcinoma. The most common site is at the entero-vesical anastomosis (50%). Ninety percent develop after 10 years postoperatively with a median latency period to presentation of 19 years for any type of enteral segment. The estimated incidence is between 0-272 per 100,000 patients / year. In addition, there is the risk of renal impairment, upper tract dilatation, mucus production, late recurrence of symptoms, B12 / folate deficiency and altered bowel habit.
Case 2
- Mitrofanoff appendicovesicostomy, a catheterisable continent urinary conduit.
- Ileum, Yang-Monti tunnelled flap valve procedure.
- As the urinary bladder fills with urine, the pressure in the bladder increases. Consequently, the pressure on the tunnelled submucosal conduit increases and then closes as a valve.
- Bladder neck closure, tight pubovaginal sling, artificial urinary sphincter.
- Refractory neurogenic lower urinary tract dysfunction including non-relaxing sphincter dysfunction, refractory idiopathic bladder dysfunction, and as a combined procedure for augmentation cystoplasty and cystectomy with enteral bladder substitution (orthotopic bladder) to help facilitate bladder emptying.






