Following success in national selection, it soon dawns on the successful candidate that entry into higher surgical training (HST) requires more than a little clinical knowledge. The role requires administrative and organisational skills not hitherto called upon. This additional skill set may come as the biggest challenge to the newly appointed ST3 trainee. Here Andrea Tay and Rob Gray outline a guide to surviving the first year of higher training. Their advice I am sure will resonate with many. From spacing work-based assessment to indicative numbers, they provide a personal guide to this, the first and most challenging of years as a registrar. Their step-by-step guide provides a tried and tested route to navigate the all-important Annual Review of Competence Progression (ARCP). The idea of becoming ‘wingman’ to your consultant is a concept that has fallen out of vogue in recent years, yet is one that most of us with greying temples will recognise and applaud. Andrea Tay has recently been appointed as the Section Editor for the trainees’ forum and will be looking after this section of Urology News from now on. Please write to Andrea at andreatay18@gmail.com if you would like to suggest an article.
Tim Lane, Editor (2012-2015), Urology News.
Introduction
First of all, congratulations all those in receipt of a National Training Number (NTN). It demonstrates that you have mastered the skill of churning out scientific papers in a short space of time and squeezed into enough scrotal explorations. Before you start your higher specialty training (HST), take a small morale-boosting break because the next five years will be pretty intense. HST is a marathon and you should pace yourself. This guide is aimed at new ST3s who have graduated from core surgical training (CST). We provide here a summary of what to expect in the first year of HST. We hope it will shorten your ‘settling in’ time so that you can get on with the business of urology!
Before you start
Visiting the department in advance is often beneficial, the aim here being to meet with the rota co-ordinator, your predecessor and the consultant body. Objectives include:
- Learn and tweak your weekly timetable in advance.
- Read up on common presentations to that neuro-urology clinic you are supposed to do on your second day.
- Plead with the rota co-ordinator (usually a senior registrar) not to be ambushed with an on-call on the first weekend.
- Run through the timetable with your predecessor to glean any useful tips and tricks for the year ahead.
The first month
Meet your training programme director (TPD) early in your rotation and identify who your educational supervisor is. It is a good idea to have a few clinical supervisors. Before your meeting with the TPD, it is best to take a few minutes to reflect on what you think your weaknesses are (this may be everything!) and what skills you would like to gain from your placement – be it gaining new core urology skills, sub-specialty knowledge or consolidation of previously learnt skills. The first day is usually packed with trust and local induction. Do try and gain access to wards and theatres early on, as this is the only clinical free day you will have for a long time, and looking around for people to open doors for you is the last thing you want in a busy job. The first day is the best time to pop into theatres and ask the theatre co-ordinator for a locker. Most importantly of all meet the secretaries! Make sure you know for whom they work, as you will be in much closer contact with them as a specialist registrar (and they will probably type your dictated reference one day!). A good trick to maximise training is to try and synchronise your unused annual leave with your consultants, so that you are not at work undertaking unsupervised service commitments and missing crucial training lists.
Administration
Stepping up to a registrar’s post can be slightly overwhelming on the administration front. In general (and especially in clinic) it is best to dictate as soon after seeing patients as possible (or even with the patient still in the room) although that may not always be possible (but nevertheless should always be done by the end of clinic lest important clinical details be forgotten). The work does not stop here however! Letters will need to be corrected and authorised within a few days. Importantly, you should keep a list of patient names for which you have requested outpatient investigations and note down the dates, so that you can chase them up when you are free – between cases or after clinic. It is scary how easy it can be for some very important or worrying results to go unaccessed for long periods of time if no one is checking. It also serves as a good learning exercise to see the outcomes of investigations ordered.
Knowing how to get hold of operating lists and reviewing clinical notes and results in advance is crucial, so that any positive MSU or MRSA results (for prosthesis insertion) can be appropriately managed beforehand to avoid cancellations (and loss of training opportunities). The surgical booking officers are good people to befriend! Try and see if you can take charge of booking small cases (with your consultant’s agreement), which you are interested in operating on or that provide good training opportunities.
Work-based assessments
The bare minimum is 40 work-based assessments (WBAs) per year (though this does vary between deaneries) and should include a range of case based discussions (CBDs), clinical evaluation exercises (CEXs), procedure based assessments (PBAs) and direct observation procedures (DOPs) in the early years. You are also expected to complete one mini peer assessment tool (mini-PAT) per year. Needless to say, it really does pay to start doing these assessments early in your training as many programme directors take a dim view of ‘clustered’ assessments undertaken in the last month before the ARCP. In training you should complete two to three closed loop audits and it is never too early to start on these!
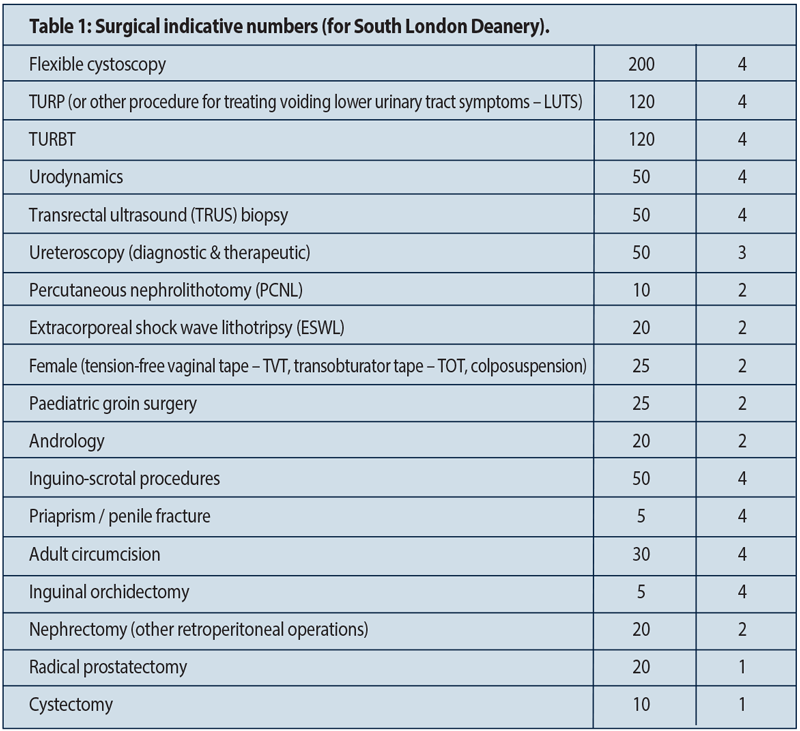
You are required to keep an accurate and contemporaneous logbook. In order to achieve your Certificate of Completion of Training (CCT), you will also need to achieve certain ‘indicative’ numbers in key operations. For the smartphone user, an easy way to keep your logbook ‘live’ is to have the e-logbook app and be vigilant about updating after each theatre session. You will not be able to achieve the required competency for certain operations until ST6/7, but you should focus your exposure on the core cases in the first two years, allowing you more exposure to the complex cases later on in training. Transurethral resection of bladder tumour (TURBTs) and transurethral resection of the prostate (TURPs) are the typical hurdles, so make sure you aim to do at least 20 per year. In order to keep track of your indicative numbers each year, you can set filters in the Intercollegiate Surgical Curriculum Programme (ISCP) logbook to only count certain operations over a certain time period. Sadly no surgical exposure – no matter how extensive – before your HST, counts for this purpose.
Courses and meetings
It is recommended that you complete the urodynamics, neuro-urology and ureteroscopy courses within the first two years. Having attended a dry and wet lab laparoscopy course will also help you with stepping up to perform laparoscopic operations when asked to. The Royal Society of Medicine (RSM) regularly holds meetings throughout the year where you can present and win substantial prizes. Regional deanery meetings are also another good place to submit abstracts.
You are expected to attend two meetings per year and present at least twice (national and international) throughout the five-year training period.
Associations
As a trainee in the UK, joining the British Association of Urological Surgeons (BAUS) is useful. The website contains a calendar where all important meetings and courses are published. The training section also allows you to familiarise yourself with the hospitals and trainers in the region. Most hospitals are moving towards the uniformed BAUS consent forms which are available on the website, and providing patients with BAUS procedure information leaflets in clinics is invaluable and can save time too. The European Association of Urology (EAU) and American Association of Urology (AUA) are venerable societies, and being a trainee member brings significant benefits. Not least because the EAU trainee subscription fee is cheap (£50), and allows free attendance at the annual congress. The pocket guidelines are a fantastic aide memoir in clinic. The Specialist Urological Registrars Group (SURG) is another good society and website to be aware of.
ARCP
If one thing is certain in your year as an ST3 it is that it will culminate in the dreaded ARCP. This typically occurs in early summer (not actually at the end of your year in training), and an in depth scrutiny of your year in training takes place. A panel of consultants and lay persons will look through your logbook, indicative numbers, WBAs, audits, courses and meetings attended, teaching experience and publications. It is a good idea to meet with your TPD during BAUS (in May) to discuss any important key issues that were not raised previously. This is also the time to voice any concerns you may have with training and may help with future rotation placement, to a certain degree.
And finally
Be a wingman to your consultant. It is crucial to know their key patients like the back of your hand, including results and admission dates. You should see them postoperatively even if you are not scheduled to do a ward round. Most consultants will expect you to know previous investigation results and indications for surgery (and some may not even let you scrub in if you are not prepared). All in all, make friends and enjoy your ST3 year. It is fun and relatively stress free before exam preparation starts!
Useful website
Curriculum Syllabus
https://www.iscp.ac.uk/documents/syllabus_U_2010.pdf