Paediatric urology training
A review of paediatric emergency services in the UK involving general surgery, urology and paediatric surgery was initiated due to the problems encountered by the lack of suitable experience outside large paediatric surgical units to deliver emergency surgery in childhood. In July 2016 a change was recommended in the provision of emergency surgical services for children over the age of five including procedures such as inguinal hernia, torsion of the testes, appendicitis, etc.
Exploration of the acute scrotum features at level four at all stages of the curriculum now, both in urology and more recently general surgery. Management of these conditions cannot be limited to those individuals in paediatric practice as delays can occur due to transfer. Certificate of Completion of Training (CCT) guidelines have now been amended for urology so that trainees will have to complete no less than 40 days or the equivalent of 80 sessions in training in paediatric urology environments such as clinics, wards, accident and emergency, and theatre lists, between the years of ST3 and ST7. This may be taken in block or in smaller units of time. For trainees that are within the training programme already, this should be completed on a pro rata basis depending on how many years they have already completed in the programme.
Specialty Advisory Committees (SAC) liaison members will be mindful that each programme will have its own way of organising this and that trainees will take between four and five years to obtain the necessary experience stated in the guidelines. New guidance to help training programme directors (TPDs) will be available shortly.
Trainees wishing to develop their skills further will be able to complete a special interest module in paediatric urology. This can be done at ST7, or as out of programme training (OOPT), or in exceptional circumstances as an out of programme experience (OOPE). For those wishing to practise paediatric urology as part of their consultant job plan it is envisaged that they will need to take up either a further six months paediatric urology post completion of CCT training to develop their practical skills, or work in a supervised capacity by visiting a paediatric surgical unit until independent competency is reached. Thereafter they will need to work in collaboration with a regional unit in a hub-and-spoke model with a paediatric urology / surgery unit. They will have to record their work and document this for continuing professional development in paediatric urology.
If we can follow through on this paradigm, then once again we will have urologists in the UK who can provide excellent local care for the paediatric urology population. The British Association of Urological Surgeons and the SAC in Urology support this and wish to ensure that there are adequate learning opportunities within the urology curriculum and the various training programmes.
National Selection
The next round of National Selection will be held on 6-7 April 2017 at Elland Road Stadium in Leeds. The only planned change is an updated portfolio station which will be based on models currently in use by most other surgical specialties. It will rely more on a rigid and detailed scoring system of the applicants’ portfolio, and less on a traditional interview format. Applicants will be given clear instructions on what evidence they will be required to show and how they should lay out their portfolios to make scoring as straightforward as possible.
Simulation
The second Urology Simulation Boot Camp for new ST3 trainees took place from the 15-19 September 2016 in Leeds and 34 trainees attended. The cohort of trainees included a few CT2 trainees aspiring for urological National Selection. There were four to six participants in each group and pre coursework was done via the Virtual Learning Centre at Leeds. This included multiple choice questions (MCQ), and experience in radiation protection and laser training.
“The curriculum in urology to CCT has now been benchmarked to ensure it has assessment tools by which each aspect of the curriculum can be assessed.”
The course consisted of eight modules and the stations included scrotal surgery with priapism and penile fracture, flexible cystoscopy and suprapubic catheterisation, ileal conduit formation and ureteric reimplantation. Basic laparoscopic skills were taught. Other techniques covered were transurethral resection of the prostate (TURP) and bladder tumours (TURBT) with bladder washout, injection of botulinum toxin, principles of insertion of tension-free vaginal tape (TVT) and transobturator tape (TOT) with pelvic anatomy, flexible ureteroscopy, cystoscopy and stent insertion. In addition, scenarios in general management, communication and ward-based scenarios using both SimMan® 3G advanced patient simulators and actors were taught and practised.
Assessment and evaluation was undertaken with pre and post course formative assessment of knowledge and judgement. This year’s cohorts of trainees will include comparison against trainees who did not attend the course using existing workplace-based assessments (WBA) with direct observation of procedural skills (DOPs) and procedure-based assessment; this will be then evaluated. The Joint Committee on Surgical Training (JCST) is approaching the General Medical Council (GMC) to see if additional funds can be made available for simulation. If this becomes available then it is hoped that simulation will become a mandatory feature within the curriculum.
It is planned to introduce a cadaveric / simulation ST5 boot camp in approximately 12 months’ time. This will follow the curriculum and, for those who have attended the original ST3 boot camp last year, provide ongoing assessment of progress. It is planned to introduce a pre-CCT ‘soft skills’ boot camp to cover leadership, management, training the trainers, ethics and conflict.
Benchmarking
The curriculum in urology to CCT has now been benchmarked to ensure it has assessment tools by which each aspect of the curriculum can be assessed. This will include the present variety of workplace-based assessments.
Future developments with respect to benchmarking of the curriculum will include guidelines for which aspects of the curriculum should be evidenced in each year of training. It is likely that all aspects of the curriculum will need to be assessed at some stage and new Standards for Curricula are now being consulted on. They will require curricula to be written with high level outcomes-based focus. The emphasis on the detailed, granular syllabus is being reduced. Assessments will need to show that the requirements for the high level outcomes have been reached. The likely process for this will be for specialties to design entrustable professional activities (EPAs) and to base the curriculum on these. It is hoped that the general surgery submission will provide a model which will help inform other specialties as they undertake their own revisions that will be required over the next three years or so.
CCT guidance
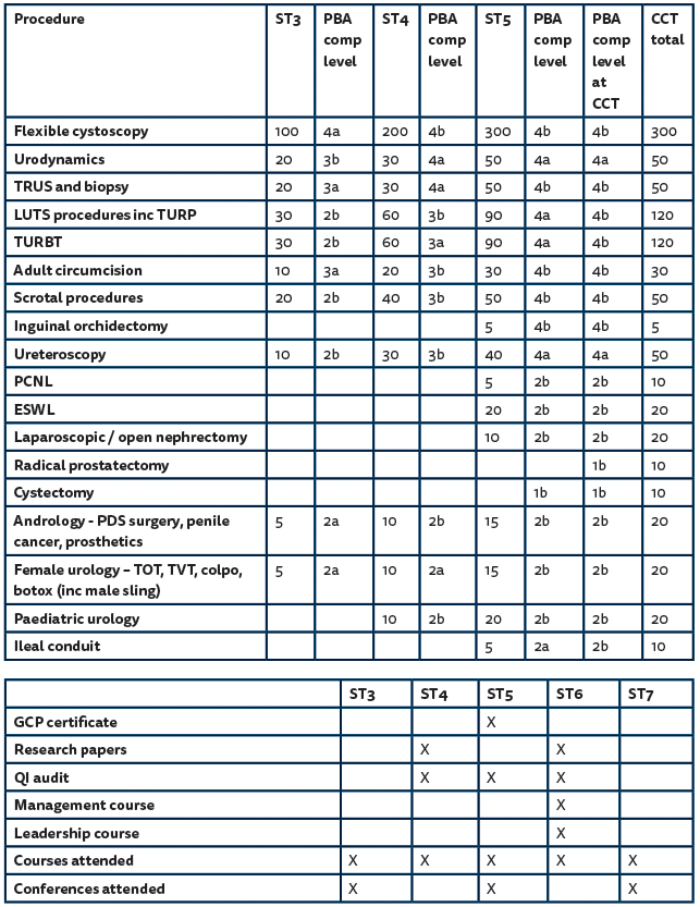
The CCT guidelines have been updated. These include a reduction in indicative numbers for radical prostatectomy and cystectomy and the introduction of ileal conduit. The latter is a transferable skill, obtainable at the time of performing a cystectomy in many cases, and has been introduced to address the needs of emergency surgery skills.
Requirement for a Good Clinical Practice certificate has also been introduced, together with two first author publications, to meet GMC requirements for research and reduce differences between surgical specialties. This whole area is under review and is likely to change significantly over the next year.
From July 2016 both outcome six and CCT sign-off will occur by the TPD and SAC liaison member at the final Annual Review of Competence Progression (ARCP). It is very important that both ensure that all the guidelines and competencies have been met by the trainee and checked by the TPD and SAC liaison member well in advance of the final ARCP. Trainees should be informed that if evidence is not available then outcome six and award of CCT may be delayed. To aid this, outcome six and CCT guidance has been produced and is available on the Joint Committee on Surgical Training (JCST) website under urology CCT guidelines (www.jcst.org/quality-assurance/certification-guidelines). A pre-CCT checklist includes guidance for aspects of the curriculum that should be achieved at certain stages of training (Figure 1).
Figure 1: ST 3-7 checklist guide.
Core surgical training
The Core Surgical Training Committee (CSTC) is keen to see a combination of themed and generic programmes to ensure that trainees are able to develop their experience to fulfil ST3 criteria in a career speciality of their choice. Otolaryngology, trauma & orthopaedic surgery, and vascular surgery SACs are considering run through pilot programmes.
Improving surgical training (IST)
The General Surgery SAC are implementing an IST run through pilot from 2018. The aim of the project is to produce a trainee that is the same product surgically at CCT as at present, but trained in a different way which will have addressed the problems at the core surgical level of training.
The current plan is for a prospectus to be sent out from the Royal College of Surgeons (RCS) in partnership with Health Education England (HEE) to all heads of schools in the next month looking for expressions of interest. Interested local education and training boards (LETBs) are being asked to commit to delivering pilot IST aspects of the general surgery curriculum (which has now been submitted to the GMC and is awaiting approval) and to commit to an enhanced method of assessment including EPAs with mechanism for acceleration, deceleration and termination of trainees as appropriate.
Assuming that the pilot goes ahead in general surgery, two to three LETBS will appoint 20-40 trainees at the end of Foundation Year Two (FY2) into the run through programme. Selection is likely to include situational judgement and MCQs. Trainees at selection will have the choice of: a) Run-through pilot programme, b) Standard core training, c) No preference.
This is to ensure there is no selection bias to the project and allow early reporting by the middle of 2020.
Urology have been asked whether they wish to take part, and the implications for urology being involved in the pilot are as follows:
- A limited number of LETBs will be involved (two to three).
- For the majority of LETBs nothing changes.
- For trainees involved with the LETBs they have the option of choosing run through pilot, standard core, or no preference on their application at ST3.
- Whether urology is involved or not, urology trainers will be involved in the new methods of assessment of trainees in the pilot LETBs.
- Whether urology is involved or not, urology trainees will be involved in the new methods of assessment of trainees in the pilot LETBs, although still using the present ones as well.
- The on call rota at the core level will involve the use of physician assistants and nursing practitioners (number and competency level to be decided).
- The final CCT product with respect to competency is not expected to change, with no reduction in training time.
The urology community (SAC, BAUS Trustees and Council, and SURG) will need to take a view on what option available at present best meets the need of the specialty and our patients.
Intercollegiate Surgical Curriculum Version 10 (ISCP V10)
The recent update was released at the start of August 2016 and was intended to be more user-friendly for both trainer and trainee. Despite exhaustive in-house testing, and as is to be expected with a completely new website and database, there have been problems related to functionality in some areas. Many of these have been corrected and a programme of sequential continued correction based on priority is in place. Feedback has been mixed with the helpdesk receiving a large number of queries, although these are now reducing in number. Other feedback has been positive.
There is a facility, developed by the University of Warwick in collaboration with the ISCP, which will allow improved visualisation of a series of WBA outcomes. A working prototype searching real, anonymised data was demonstrated to the ISCP Management Committee and received unanimous approval. Work will now commence to examine how this may be integrated into the ISCP. Although the Warwick group work with large scale NHS patient data, governance issues will need to be addressed, as will intellectual property and the resources required.
“Requirement for a Good Clinical Practice certificate has also been introduced, together with two first author publications, to meet GMC requirements for research and reduce differences between surgical specialties.”
Academic trainees
The response from the National Institute for Health Research (NHIR) with respect to academic surgical training and the need for robust clinical training quality assurance, was that this should come through benchmarking at recruitment and then optimisation of the ARCP rather than through introduction of another process. NIHR is at present undertaking a review of training.
Return to work guidance
There is now new guidance for those trainees taking extended leave. For planned leave, such as out of programme for research (OOPR), out of programme for career break (OOPC), parental leave, planned sick leave and carers leave, an initial meeting should occur with the trainee arranging to meet with their TPD at least three months before any period of extended leave commences and complete a ‘Planning an absence from practice’ checklist (see ‘Sources’ section on the JCST website), which will produce an individualised profile of current and anticipated learning needs on return to clinical training. With unplanned leave the trainee has a responsibility to inform their TPD of any unplanned absence as soon as it is clear that this will be for an extended period. The trainee should meet with their TPD and again complete a checklist (www.jcst.org/key-documents/docs/return-to-work-guidance/view?searchterm=return+to+work) and formulate a plan for their period of absence. It is recommended that before the initial meeting the trainee completes a self-assessment of their progress against the JCST certification guidelines and training checklists for their specialty.
At this initial meeting, a programme of interim meetings should be agreed for the purpose of monitoring the situation of the trainee and subsequently for planning their return to clinical training. A meeting prior to return to training should then be organised, the purpose of which is to make definitive plans for the return to training. This should therefore take place between six weeks and three months prior to a return to clinical training, which allows for the implementation of any plans.
The TPD should then meet with the trainee for a progress meeting, ideally six to eight weeks after clinical training has recommenced, to monitor progress towards goals agreed at the meeting prior to return. Depending upon the progress made, it may be necessary to set further goals and arrange follow-up.
Workforce planning
Based on age and future retirement planning we can probably assume that we will need to replace a minimum of 530 posts through retirement over the next 12 years just to stand still. We will need an average of 44 CCT trainees to take up UK consultant posts per annum to maintain numbers with no expansion. That means over a five-year training cycle the best we can expect is 64 CCT awards per annum.
The number of consultants increased by 48 in the last 12 months (in a year which was pretty average in terms of expansion) and it looks as if we are going to be seriously short if the current trends continue. The number of unfilled posts has increased from 13 in 2012 to 121 posts in 2016.
If all posts were filled the expansion over the last 12 months would actually have been 9.7%, rather than 4.6%. We therefore need to plan to increase training numbers, and I will be discussing this with HEE, but in the current climate we are unlikely to get a real increase in training numbers and competition for consultant posts will be non-existent.