Introduction
Spinal cord injury (SCI) is a devastating, life-changing condition, which is currently irreversible. Depending on the level of the spinal cord affected (and whether the lesion is complete or incomplete), patients may subsequently develop reduced voluntary motor function, sensory loss and impaired autonomic, bowel, bladder and sexual function. The causes may be classified as traumatic (e.g. following road traffic accidents or falls) or non-traumatic (e.g. secondary to malignancy, infection or vascular lesions). Traumatic SCI is more common in males and those less than 45 years [1].
Following SCI in the United Kingdom, patients are usually transferred to one of 11 specialised centres (Table 1) before returning to life in the community. Based on statistics from these centres, it is estimated that approximately 1200 individuals sustain a SCI in the UK each year, with around 40,000 people living with paralysis [2].
Table 1: United Kingdom Spinal Cord Injury Units.
Belfast Musgrave Park Hospital Spinal Cord Injuries Unit +44 (0)28 9066 9501
Glasgow Queen Elizabeth National Spinal Injuries Unit +44 (0)141 201 2555
Middlesbrough The North of England Spinal Injuries Centre +44 (0)1642 850850
Oswestry The Midland’s Centre for Spinal Injuries +44 (0)1691 404655
Rookwood Welsh Spinal Injuries and Neurological Rehabilitation Unit +44 (0)29 2041 5415
Salisbury The Duke of Cornwall Spinal Treatment Centre +44 (0)1722 336262
Sheffield The Princess Royal Spinal Injuries Unit +44 (0)114 271 5644
Southport The Regional Spinal Injuries Centre +44 (0)1704 547471
Stanmore The London Spinal Injuries Unit, Royal National Orthopaedic Hospital +44 (0)20 8954 2300
Stoke Mandeville National Spinal Injuries Centre +44 (0)1296 315000
Wakefield Pinderfields, Yorkshire Regional Spinal Injuries Unit +44 (0)1924 201688
Regardless of their residual level of function, patients will require life-long involvement with medical services. It is estimated that the NHS spends around £500 million pounds per year on the management of SCI patients although the extent to which this expenditure occurs outside of the specialist centres is difficult to quantify [2]. A study of health care utilisation amongst patients with SCI found that 38% of British patients received care from doctors other than their general practitioner or spinal injuries specialist [3]. Health care providers in the specialist centres have access to the training and experience required to develop expertise in the management of these patients.
“The emergency or elective admission of a spinal cord injured patient may be viewed as a challenging and potentially anxious experience, for health care providers and patients alike.”
Of particular importance is the need to recognise and treat potentially fatal complications such as autonomic dysreflexia (AD) (Figures 1 and 2). Unfortunately this experience is not universally available as suggested by the findings from a recent survey of UK SCI patients in which some respondents expressed concerns regarding the treatment they received from non-specialist centres [4]. In these settings, the emergency or elective admission of a spinal cord injured patient may be viewed as a challenging and potentially anxious experience, for health care providers and patients alike. The aim of this article is to highlight some of the general aspects of care, which should be considered when a SCI patient is referred or admitted for urological treatment at a non-specialist centre.
Figure 1: Autonomic dysreflexia
This potentially life-threatening condition usually affects patients with lesions at or above T6 level. It is due to an excessive sympathetic nervous system response to a noxious stimulus, most commonly a distended bladder. This results in massive vasoconstriction of the splanchnic and other vessels below the level of the lesion resulting in hypertension (systolic pressures up to 300mmHg). The rise in blood pressure is detected by aortic and carotid baroreceptors, which trigger compensatory parasympathetic mediated bradycardia and vasodilatation above the level of the lesion. Reported symptoms include headache, flushing, sweating, blurred vision and skin changes. Untreated AD can result in cardiac arrhythmias, seizures, intracranial haemorrhage and death.
A high index of suspicion is vital if the diagnosis is to be made in a timely fashion. Management comprises recognition, identification and removal of the noxious stimulus, followed by a period of monitoring until the symptoms and blood pressure normalise (Figure 2).
Figure 2: the management of autonomic dysreflexia (adapted from Gall et al [10]).
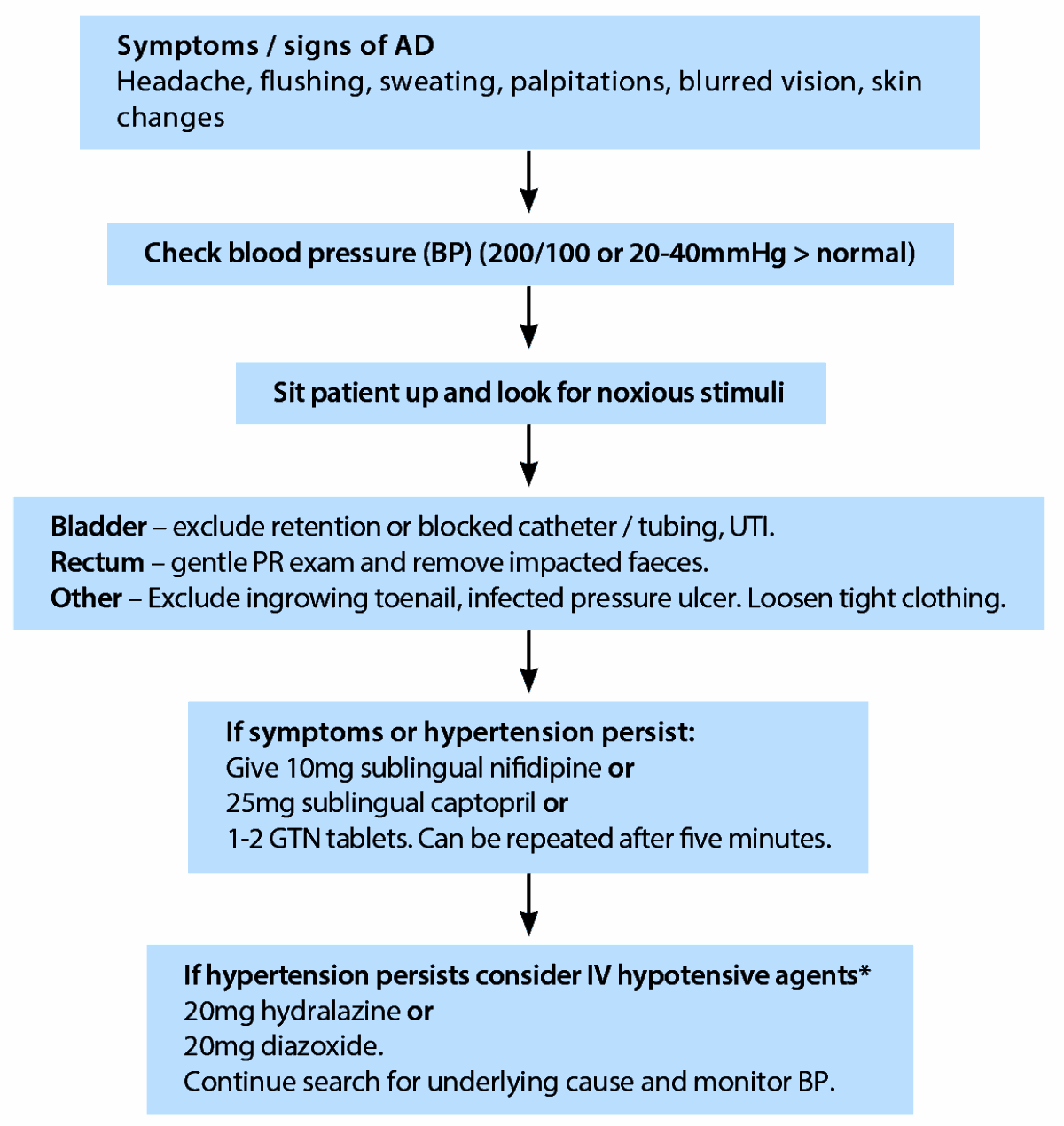
* Treatment should be administered in a monitored setting with advice from the regional SCI unit.
Referrals to the outpatient department
Recurrent urinary tract infections (UTI)
- Symptoms and signs include fatigue, new onset of incontinence, cloudy or malodorous urine.
- Antibiotic treatment should be based on the results of urine culture and antibiotic sensitivity tests, in line with local resistance patterns.
- In severe or recurrent infections, exclude underlying causes such as urolithiasis. First line investigations are ultrasound (USS) and flexible cystoscopy, however computed tomography of kidney, ureter and bladder (CT KUB) can be used in selected cases.
- Routine antibiotic prophylaxis is not usually recommended due to the risk of developing antibiotic resistance although self-start regimes can be useful.
Urolithiasis
- May present with UTI, sepsis or autonomic dysreflexia.
- CT KUB is the gold standard for acute investigation of renal colic. Abdominal radiographs are not generally useful due to the presence of bowel gas and faecal loading.
- Consider annual surveillance USS to look for asymptomatic calculi.
- Extracorporeal shock wave lithotripsy (ESWL) may be used with stone free rates of 50-70%. There is a risk of shock wave induced muscle spasms and autonomic dysreflexia if analgesia is not used [5].
- If bladder calculi are suspected, flexible cystoscopy can be carried out under local anaesthetic but for patients with lesions above T6, a general anaesthetic procedure should be considered in view of the risk of autonomic dysreflexia occurring during the procedure.
Catheter issues
- Patients who use an indwelling catheter should ideally have a suprapubic catheter (SPC) to remove the risk of chronic urethral injury.
- Catheter bypassing can be due to blockages, detrusor overactivity or sphincter weakness. If blockages are the cause, the problem will resolve for days or weeks after each catheter change.
- Recurrent blockages can be managed by increasing the suprapubic catheter diameter (to 18 or 20Ch) and the frequency of changes. Weekly bladder washouts in the community with saline or solutions such as Suby G are sometimes used. If these measures are unsuccessful, perform rigid cystoscopy to wash out the bladder and exclude calculi.
- Detrusor overactivity can be treated by oral anti-muscarinic agents or botulinum toxin injection into the bladder wall.
- Stress incontinence may need surgical treatment e.g. autologous sling insertion or urethral closure.
Haematuria
- Patients with SCI probably have a higher risk of bladder cancer compared to the general population although there is significant variation in the estimates of the risk [6].
- Visible haematuria should always be investigated urgently to prevent any delay in treatment.
- Cystoscopy should not be performed with local anaesthesia only, in patients with lesions above T6 due to the risk of autonomic dysreflexia.
Erectile dysfunction
- The majority of men with SCI will experience psychogenic, reflexogenic, nocturnal or mixed erections.
- Phosphodiesterase inhibitors, intra-cavernosal injections, vacuum constriction devices and anterior sacral root stimulation, may all be employed as treatment options, according to patient choice [7].
- Patients with lower motor neuron injuries tend not to respond as well to phosphodiesterase inhibitors compared to injection therapy.
- Intra-urethral agents have not proved to be particularly useful in patients with SCI [8].
Male infertility
- Men with SCI may develop defects in Leydig and Sertoli cell function in addition to the loss of antegrade ejaculation.
- The mainstay of management is recovery of semen (using penile vibratory stimulation, electro-ejaculation or surgical retrieval) for use with assisted conception techniques.
- Investigation and treatment for male factor infertility should ideally be referred to a specialist centre.
Inpatient care of the SCI patient
Skin care
- Skin and pressure areas should be examined daily. Particular attention should be given to areas such as the ischii, sacrum, coccyx, trochanters and heels.
- Attempts should also be made to minimise moisture and incontinence. Consider using The Spinal Cord Injury Pressure Ulcer Scale (SCIPUS) which has been validated for use with SCI patients, as an alternative risk assessment tool on admission [9].
- Patients should be managed on an appropriate pressure-relieving mattress with position changes / turns, at least every two hours.
- Wheelchair-using patients should ideally have their own chairs brought in for use during their recovery as they will often have individually prescribed equipment such as pressure redistributing cushions.
- Patients who are admitted with pressure ulcers or develop an ulcer during the course of their stay, should be managed in consultation with a tissue viability nurse. Severe ulceration may require surgical intervention and involvement of the plastic surgery team.
Bladder management
- Patients who normally perform clean intermittent self-catheterisation (CISC) may be unable to continue this practice during an acute illness. In this instance, placing a urethral catheter for a short time may be more appropriate, especially in those with catheterisable bladder reconstructions.
- Staff need to ensure that there is no traction on the catheter (to prevent urethral and sphincteric trauma), as the patient may lack sensation.
- If a long-term catheter has not been changed for a prolonged period, consideration should be given to performing a bladder ultrasound scan to identify encrustation or stone formation on the intravesical portion of the catheter.
- A stenosed suprapubic catheter track can often be salvaged by the introduction of a hydrophilic guidewire (e.g. Sensor™, Boston Scientific). The track may then be dilated under USS guidance to allow the SPC to be replaced.
- Care must be taken during endoscopic guided catheterisation procedures to reduce the risk of autonomic dysreflexia.
Bowel management
- The patient’s individual regime should be strictly adhered to where possible to reduce the risk of constipation or faecal impaction as these stimuli can also induce AD.
- Bowel management techniques include: oral prokinetic agents (e.g. metaclopamide), suppositories, enemas, abdominal massage, manual evacuation and transanal irrigation.
- Ensure patients receive adequate fluid and fibre intake during their admission, to maintain stool consistency.
- If there are no bowel movements despite an appropriate regime, bowel obstruction should be excluded radiologically [10].
Management of muscle spasm
- Excessive spasticity in the muscles of the lower limbs can result in pain, muscle spasms and contractures.
- Conservative management techniques include passive muscle stretching, orthoses, and oral anti-spasmodic agents e.g. baclofen, benzodiazepine, clonidine, tizanidine and dantrolene. Refractory cases may be managed by intra-thecal baclofen pump insertion [11].
- Failure of an intra-thecal pump to deliver the correct dose of baclofen can result in side-effects including drowsiness, nausea, headache, muscle weakness and light-headedness. These should be managed by re-introducing oral baclofen and specialist review of the pump settings.
- A small proportion of patients may develop life-threatening symptoms such as hyperthermia, seizures, disseminated intravascular coagulation, multisystem organ failure and cardiac arrest, in response to the acute withdrawal of baclofen. These patients should be managed in the intensive care department with advice from or transfer to a specialist SCI centre [12].
Chest management
- SCI (particularly cervical and upper thoracic lesions), may cause respiratory muscle dysfunction. This can result in an ineffective cough, difficulty clearing secretions, and an increased risk of chest infection.
- Patients should therefore have regular assessment of their respiratory system e.g. clinical examination, respiratory rate and pulse oximetry.
- Regular chest / neuro-physiotherapy input should be sought e.g. for assisted cough and inspiratory muscle training [13].
- Suction catheterisation or referral for bronchoscopy may be required for secretions, which prove difficult to clear.
Perioperative care of the SCI patient
Venous thrombo-embolism prophylaxis
- Patients with established SCI are at increased risk of developing a deep vein thrombosis and should be commenced on standard prophylactic therapy (according to local policy), assuming there are no contraindications.
- Care should be taken when using anti-embolism stockings in those with sensory loss, due to the risk of skin damage.
- The routine use of post-discharge prophylaxis is not recommended [14].
Positioning
- Careful positioning of the patient’s hips during transfers is important to reduce the risk of hip afferent induced lower limb spasms.
- Positioning on some operating tables may be challenging due to spinal curvature or limb contractures.
- Care should be taken to ensure pressure areas and previous ulcer sites are well protected whilst the patient is on the operating table.
- Tetraplegic patients are also poikilothermic and require a warm ambient temperature on the ward and in theatre, where they may be partially exposed for prolonged periods.
Anaesthesia
- The development of intraoperative autonomic dysreflexia may be prevented by the use of general, spinal or epidural anaesthesia [15].
- Inhalation agents such as sevoflurane in combination with nitrous oxide are effective at blocking AD but can result in hypotension.
- The use of suxamethonium should be avoided due to the risk of fatal hyperkalaemia [16].
- Local anaesthesia may be used for minimally invasive procedures but should be avoided for cystoscopy in patients with lesions above T6 due to the risk of AD [17].
Endoscopy
- Endoscopic access is usually achievable even if abduction is very limited, providing the patient’s hips can be flexed.
- If the patient has had an artificial urinary sphincter implanted, this may need to be deactivated by an appropriately trained person.
- Determine whether the patient has undergone any form of bladder augmentation or reconstruction as these procedures may make ureteroscopic access more challenging.
- Long-term indwelling catheterisation can result in a small contracted bladder. Care should be taken to avoid over-distension or rupture during cystoscopy.
Conclusion
It is important to be aware of the many physiological complications that can occur following SCI, in order to reduce the risk of adverse events during hospital admission.
In many cases, patients with an established SCI can be managed in non-specialist centres without any problems. However, physicians who are caring for these patients should ideally maintain a low threshold for contacting the local SCI unit for specialist advice if necessary.
References
1. Hasler RM, Exadaktylos AK, Bouamra O, et al. Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J 2011;20(12):2174-80.
2. Spinal Cord Injury Statistics. Accessed from:
http://www.apparelyzed.com/
statistics.html
3. Donnelly C, McColl MA, Charlifue S, et al. Utilization, access and satisfaction with primary care among people with spinal cord injuries: a comparison of three countries. Spinal Cord 2007;45(1):25-36.
4. Preserving and Developing the National Spinal Cord Injury Service. Accessed from:
http://www.spinal.co.uk/
userfiles/images/uploaded/
pdf/234-242491.pdf
5. Welk B, Fuller A, Razvi H, Denstedt J. Renal stone disease in spinal-cord-injured patients. J Endourol 2012;26(8):954-9.
6. Subramonian K, Cartwright RA, Harnden P, Harrison SC. Bladder cancer in patients with spinal cord injuries. BJU Int 2004;93(6):739-43.
7. Moemen MN, Fahmy I, AbdelAal M, et al. Erectile dysfunction in spinal cord-injured men: different treatment options. Int J Impot Res 2008;20(2):181-7.
8. Deforge D, Blackmer J, Garritty C, et al. Male erectile dysfunction following spinal cord injury: a systematic review. Spinal Cord 2006;44(8):465-73.
9. Mortenson WB, Miller WC; SCIRE Research Team. A review of scales for assessing the risk of developing a pressure ulcer in individuals with SCI. Spinal Cord 2008;46(3):168-75.
10. Gall A, Turner-Stokes L; Guideline Development Group. Chronic spinal cord injury: management of patients in acute hospital settings. Clin Med 2008;8(1):70-4.
11. Elbasiouny SM, Moroz D, Bakr MM, Mushahwar VK. Management of spasticity after spinal cord injury: current techniques and future directions. Neurorehabil Neural Repair 2010;24(1):23-33.
12. Mohammed I, Hussain A. Intrathecal baclofen withdrawal syndrome- a life-threatening complication of baclofen pump: a case report. BMC Clin Pharmacol 2004;4:6.
13. Sheel AW, Reid WD, Townson AF, et al.; Spinal Cord Rehabilitation Evidence Research Team. Effects of exercise training and inspiratory muscle training in spinal cord injury: a systematic review. J Spinal Cord Med 2008;1(5):500-8.
14. CG92 Venous thromboembolism - reducing the risk: full guideline. Accessed from:
http://www.nice.org.uk/
nicemedia/live/12695/
47920/47920.pdf
15. Yoo K, Hwang J, Jeong S, et al. Anaesthetic requirements and stress hormone responses in spinal cord-injured patients undergoing surgery below the level of injury. Anesth Analg 2006;102(4):1223-8.
16. Petit JS, Delahaye JM, Malinovsky JM. Perioperative management of traumatic spinal cord injured patients after the acute phase. Ann Fr Anesth Reanim 2008;27(5):416-25.
17. Vaidyanathan S, Soni B, Singh G, et al. Use of Flexible Cystoscopy to Insert a Foley Catheter over a Guide Wire in Spinal Cord Injury Patients: Special Precautions to be Observed. Adv Urol 2011;538750.
TAKE HOME MESSAGE
-
All members of the health care team should be aware if a patient is at risk of autonomic dysreflexia and be familiar with the appropriate treatment measures to take.
-
Individual regimes for bowel and bladder management should be established and adhered to where possible.
-
Close attention needs to be paid to skin care especially in those with previous pressure ulcers.
-
The surgical team must consider the perioperative issues and liaise with anaesthetic team to determine the safest technique for surgical intervention.
Declaration of competing interests: None declared.