Introduction
Complex ureteric strictures present a significant challenge with some patients undergoing multiple separate urological and radiological procedures to try to cross a stricture without success. Cross-departmental collaboration with uroradiology may allow a decrease in the number of separate interventions. Often failure is secondary to a fixed stricture with a mobile or tortuous ureter above or below resulting in kinking of wires and an inability to progress. The rendezvous technique involves using a combined antegrade and retrograde approach to cross or bypass difficult ureteric strictures or ureteric disruption.
Table 1: Causes of ureteric strictures
-
Malignancy (intraluminal)
-
Malignancy (extrinsic compression)
-
Lymphadenopathy
-
Radiotherapy
-
Urolithiasis
-
Retroperitoneal fibrosis
-
Periureteric fibrosis secondary to AAA
-
Infection
-
Endometriosis
-
Trauma
-
Iatrogenic surgical trauma – direct injury or ischaemic (commonly colorectal surgery, hysterectomy, vascular surgery, endourological surgery)
-
Bladder wall hypertrophy
-
Prostatic enlargement
-
Idiopathic
-
Congenital
Background
Bagley et al. first described the use of a combined antegrade and retrograde approach in the literature, when they reported a combined percutaneous and flexible ureteroscopic approach for management of an obliterated pelviureteric junction (PUJ), resulting in successful treatment with endopyelotomy [1]. Subsequently, Watson et al presented their point of technique article describing the ‘rendezvous’ procedure in 2002 [2].
More recently, the rendezvous technique has been used to cross the transected ureter in cases of delayed presentation of iatrogenic ureteric injury [3-5]. The majority of reported studies have been case studies or case series, highlighting the small volume of patients that have these complex strictures.
How is the rendezvous technique performed?
General anaesthesia is the norm, although it has been reported under epidural and intravenous sedation [6], in a supine oblique position (such as modified Galdakao-Validivia position) and with intravenous antibiotic prophylaxis with an emphasis on covering skin commensals.
The patient will often already have a percutaneous nephrostomy in place allowing a nephrostogram to delineate the anatomy of the stricture. Cystoscopy and then semi-rigid ureteroscopy is performed to the level of the stricture and concurrently, a hydrophilic antegrade wire is passed down to the level of the stricture. Antegrade methylene blue can be used to aid the endourologist in identifying the lumen of the stricture which can be subsequently treated using a holmium laser.
If an antegrade wire is identified at ureteroscopy, a basket can be used to snare the end of the wire and pull it through. Alternatively, if the antegrade wire passes the stricture, then it can be grasped with the cystoscope and biopsy forceps / stent graspers, pulled through and anchored, to straighten the ureter, which may aid ureteroscopic access.
With a safety wire in place, the stricture can be dilated, lesion biopsied or calculi treated. The variations on this technique have been presented, including using antegrade nephron-ureteroscopy and, pulling the wire antegradely instead of retrogradely (Figure 1-3).
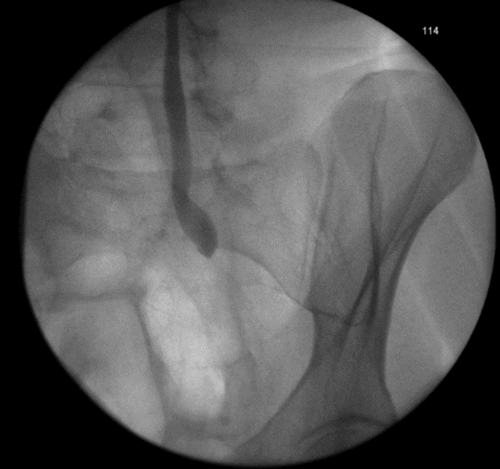
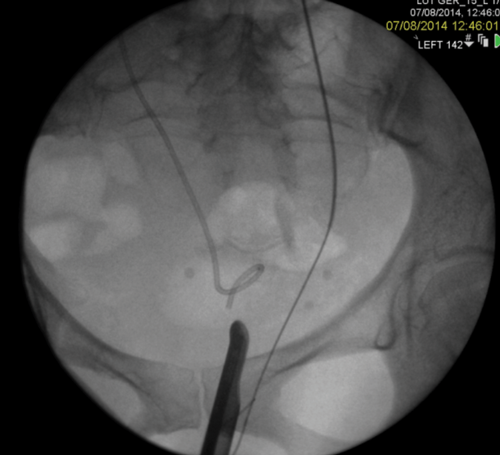
Figure 1: An example of the rendezvous procedure for an iatrogenic injury to
distal ureter during a laparoscopic pan-proctocolectomy for ulcerative colitis.
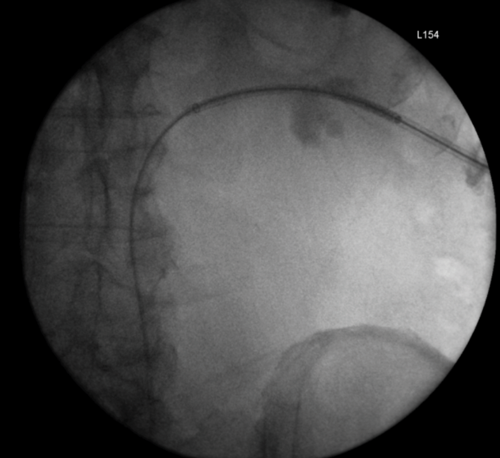
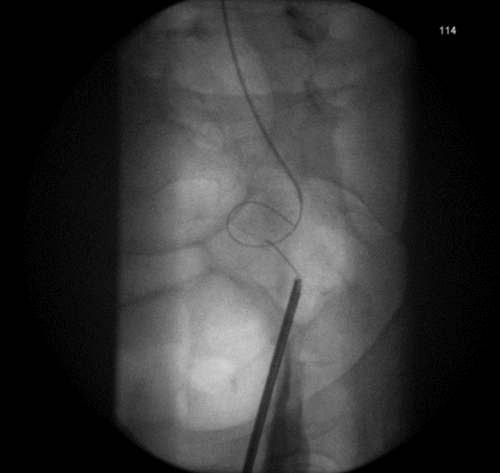
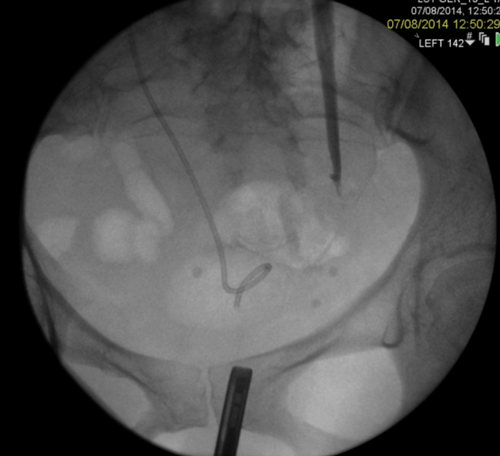
Figure 2: A Rendezvous in a patient with prostate cancer obstructing the left ureteric orifice, a partial staghorn calculus in the left kidney and left lower ureteric stones. Resection of tumour over ureteric orifice and antegrade wire.
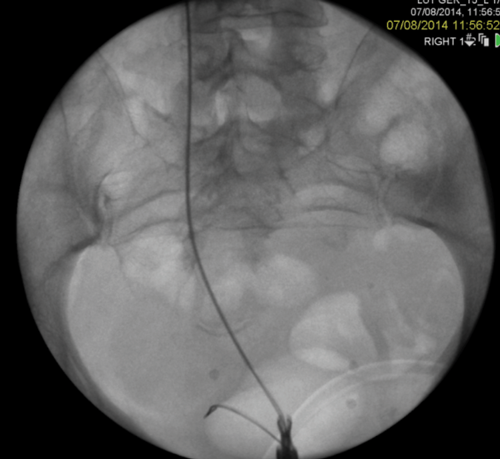
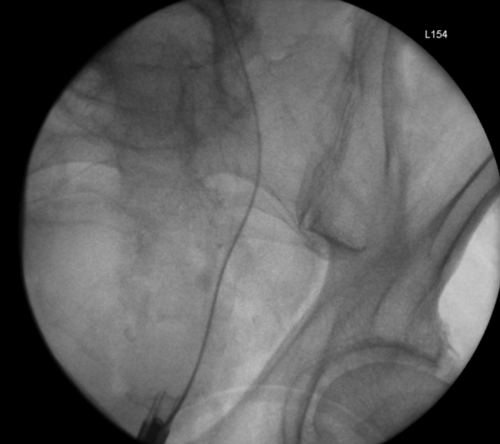
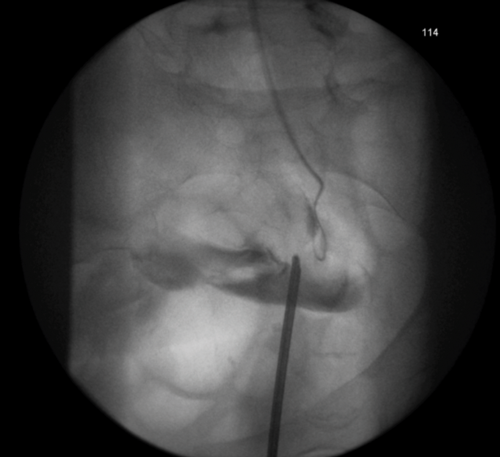
3a. Right antegrade wire insertion and pull-through.
3b. Right JJ stent in situ. Failed left antegrade wire passage.
3c. Left intraoperative nephrostogram showing obliterated left distal ureter.
3d. Right nephrostogram one week postoperative.
Figure 3: A 51-year-old woman, initially presenting with acute kidney injury, with bilateral distal ureteric obstruction secondary to locally advanced cervical cancer. Bilateral rendezvous, technically successful on right but failed on left secondary to ureterovaginal fistula.
A review of the literature
In 2002 Watson et al. [2] presented their ‘point of technique’ with a case series of 20 patients with a range of underlying pathology including complications of previous open surgery, strictures with stones, prostate cancer, bladder cancer and bladder wall hypertrophy. Technical success in crossing the stricture was reported in 20/20 patients. Two patients stented for malignancy were left with palliative stents whilst receiving adjuvant treatment and three cases required further surgical treatment (one had a Boari flap reconstruction, one required revision of ileal conduit and one underwent nephrectomy). Five patients with co-existing stones were treated in the same sitting, and all five were stone and stent-free at the end of follow-up. Seven out of fifteen surviving patients were stent-free at the end of the follow-up period (mean 15 months; range 12-36 months).
A series of 16 ureters / 11 patients with a range of pathologies (ranging from relapsing dehiscence of cystostomy after transvesical adenomyectomy, postoperative ureterovesical junction (UVJ) fibrosis, displaced percutaneous catheter postoperative pyeloplasty, UPJ stricture, obstruction secondary to prostate cancer, iatrogenic injury post hysterectomy and extrinsic compression by rectal cancer) was presented by Macri et al. in 2005 [7]. Sixteen of sixteen were technically successful, with no morbidity or mortality, with an increased stenting success rate as compared to antegrade approach, but no follow-up data were included.
In addition to these series, there have been several case studies and small series published, which highlight a range of different clinical scenarios where a combined approach has been successful.
Postoperative urinary diversion
complications In 2005 Anderson et al. [8] described a rendezvous procedure in a patient with an obstructed left ureter and infected urinoma, who presented one month after a laparoscopic cystectomy and formation of ileal conduit. After a period of nephrostomy free drainage, a combined antegrade and transconduit retrograde approach, with balloon dilatation of the stricture and stenting with tailed nephrostomy tube was performed. After 20 weeks of free drainage, this patient was converted to a Memokath 051 metal stent with good result but no long-term follow-up data was reported.
Intra-urinoma rendezvous procedures have also been described by Gray et al. (1992) for managing a ureteric leak with fistulae to colon and vagina in a patient with ovarian cancer; in this procedure, a guidewire was inserted retrogradely up to the urinoma and snared antegradely to be withdrawn through the proximal ureter to allow stenting [9].
Other urinary diversion-associated pathology
In 2010 Delvecchio [10] presented a small case series of five patients with urinary diversion-associated pathology, including obstructing ureteral stone in a man with a uretero-sigmoidostomy, two patients with valve stricture in hemi-Kock urinary diversions, anastomotic stricture in a man with an ileal loop diversion and a long left ureteroenteric stricture in a man with a right colon pouch diversion. Antegrade insertion of guidewire, then retrograde semi-rigid or flexible ureteroscopy and subsequent laser incision of stenotic segments or fragmentation of calculus was successful. One of the five procedures failed when the stent was removed.
In cases where stenotic segments may be hidden by a mucosal fold, a combined approach to access may enable more rapid identification of the ureter and stenotic segment.
Trauma
Postoak et al. (1997), reported a case of traumatic ureteral transection (secondary to gunshot wound), using a combined approach to snare a retrogradely inserted wire and pull it proximally through the percutaneous access site and subsequently insert an antegrade JJ stent [11].
"Impassable strictures and complete transections of the ureter present a significant challenge to the endourologist and uro-radiologist."
Thermal ureteric injury
Doody et al. (2008) [12] used the rendezvous to treat a patient with a single kidney who sustained a thermal ureteric injury after radiofrequency ablation for a 6cm renal cell carcinoma of the inferior pole of the left kidney.
The patient presented post-procedure with hydronephrosis secondary to an obstruction at the left PUJ but underwent a balloon dilatation and was stented successfully. Six months later, after a change of stent, the patient re-presented with a displaced stent (proximal end of the stent was outside the collecting system in the left perinephric space).
After a failed retrograde attempt to re-stent, a percutaneous nephrostomy was inserted and subsequently a rendezvous procedure was carried out, with an antegrade snare pulling a retrograde wire to the skin surface, followed by an antegrade balloon dilatation and stent.
Reported follow-up was until six months, at which point the patient was being treated with a long-term stent and had creatinine levels that had returned to pre-procedure levels.
Complete UPJ and ureteric strictures
Lopatkin et al. (2000) [6] used a combined approach to treat 21 patients with complete ureteric and UPJ strictures secondary to previous surgery (open kidney or upper ureteric stone removal 10/21, open pyeloplasty 4/21, ureteroscopy for ureteric calculus 4/21, and other surgical or gynaecological procedures in 3/21). Operative time ranged from 40-70 minutes. Patients were initially positioned prone and an antegrade angiographic catheter with a guidewire or a flexible nephroureteroscope was introduced to the stricture level to serve as a guide for a cold knife. The patient was then moved to dorsal lithotomy position and retrograde ureteroscopy performed. A cold knife incision was performed retrogradely in 16/21 cases and antegradely in 5/21 cases, under fluoroscopic guidance, and a super-stiff wire was passed through the stricture to the renal pelvis, and then balloon dilatation was performed. A JJ stent or nephrostomy was left in place and removed at four to six weeks.
Recanalisation was achieved in 17/21 cases. Four of twenty-one failures were UPJ strictures secondary to stone disease, in patients with several prior open procedures for stone disease, with stricture length >1.5cm and subsequently these patients underwent open pyeloplasties. Four of twenty-one developed acute pyelonpehritis treated with intravenous antibiotics; 14/17 were symptoms free; 2/17 had persistent pain (eventually requiring one to undergo pyleoplasty and one to undergo nephrectomy) and 1/17 had recurrent urinary tract infection (UTI).
The authors suggest the primary reasons for failure were stricture length >1.5cm and prominent scarring of the periureteral tissue that complicated identification of the correct direction for the incision. In these cases, pyeloureteroplasty is more likely to be successful.
Iatrogenic ureteric surgical injuries
Yates et al. (2009) [3] presented seven cases of using the rendezvous procedure for complicated iatrogenic strictures with ureteric disruption which were identified postoperatively and treated with a temporary nephrostomy for three to six months to allow peri-ureteric inflammation to improve. They subsequently underwent rendezvous procedures, with the modification that a cobra catheter or laser was used to create a retroperitoneal bypass of the stricture and insertion of a JJ stent. The JJ stent was then kept in situ for six months and then removed. Seven out of seven were technically successful. Only four of the seven patients had MAG3 renogram at 12 months as planned; one of this four had unobstructed kidney, one had an equivocal renogram and two had non-functioning kidneys (both patients had poorly functioning kidneys preoperatively but were symptomatic and the procedure improved pain).
Most recently, Pastore et al. (2015) [4] reported a case series of 18 rendezvous procedures for cases of complete ureteric detachment secondary to iatrogenic injury at time of gynaecological surgery with a mean follow-up for 26.5 months. There was technical success with restoration of ureteral integrity without leakage in 66% (12/18), ureteral stenosis in 22% (4/18), and ureteral leakage in 12% (2/18). The time from surgery to diagnosis was 3-52 days and initial management was with a percutaneous nephrostomy. The average operative time was 69.1 +/- 20.5 minutes. The nephrostomy was removed at five days and the stent left for three months. Two patients required reimplantation.
A variation on the classical rendezvous technique was described by Liu et al. in 2014 [5] who described eight cases of endoscopic realignment of iatrogenic ureteric completely transected ureters, secondary to colorectal and gynaecological pelvic surgeries. These injuries were detected at a median of 3.9 days postoperatively. Under general anaesthesia, in a modified flank roll position, an ultrasound-guided 18Fr percutaneous access was inserted and simultaneous antegrade flexible ureteroscopy and retrograde rigid ureteroscopy was performed, locating the two opposing ends of the ureteral injury, and an antegrade guidewire was inserted into the retroperitoneum through the flexible ureteroscope. Once the guidewire was located by the rigid ureteroscope, it was grasped with an endoscopic grasping forceps and pulled through and anchored outside the body. The rigid ureteroscope then followed the guidewire back to the proximal segment and passed three hydrophilic wires, and then three 5Fr JJ stents were inserted, with a covering nephrostomy and covering urethral catheter.
Eight out of eight patients were technically successful, with average operative time of 132 minutes, no major complications and average hospitalisation time of eight days, with serum creatinine levels returning to normal. Postoperative imaging at two to six weeks showed no ongoing ureteral leak and nephrostomy tubes were removed. Median duration of stent was 6.8 months (5.9-7.1). Six of the eight remained stent free, one required repeat balloon dilatation and one required long-term JJ stents secondary to obstruction secondary to cancer recurrence. Follow-up was to 21.5 months.
Summary
Impassable strictures and complete transections of the ureter present a significant challenge to the endourologist and uro-radiologist. The ultimate aim is to establish internal drainage in order to render the patient nephrostomy free, and ideally stent free in the long term, and a combined endourological approach may provide an alternative option.
This is a heterogeneous population and therefore it is difficult to make comparisons; clearly case selection is of vital importance. Success of the rendezvous procedure is reliant on the correct indications and stricture characteristics, and a multidisciplinary approach to select cases is imperative. The rendezvous procedure may provide an alternative option to avoid open surgical reconstruction in patients where this would not be appropriate.
Whether completely transected ureters can be treated satisfactorily in the long term with minimally invasive strategies is still controversial, as there is no functional reconstruction of the ureter and the fibrotic channel that forms around the stent lacks characteristics of the normal ureter. The short-term outcomes are promising but there is concern regarding increased chance of stricture recurrence, and to date, the case series in the literature have relatively short-term follow-up.
Follow-up post procedure is of importance, with serial imaging and renal function blood tests to identify the patients with progressive dilatation who require reconstructive surgical intervention.
References
1. Bagley D, Huffman J, Lyon E, McNamara T. Endoscopic ureteropyelostomy: Opening the obliterated ureteropelvic junction with nephroscopy and flexible ureteropyeloscopy. J Urol 1985;133:462-4.
2. Watson JM, Dawkins GPC, Whitfield HN, et al. The rendezvous procedure to cross complicated ureteric strictures. BJU international 2002;98:317-19.
3. Yates DR, Mehta SS, Spencer PA, Parys BT. Combined antegrade and retrograde endoscopic retroperitoneal bypass of ureteric strictures: a modification of the ‘rendezvous’ procedure. BJU international 2009;105:992-7.
4. Pastore AL, Palleschi G, Silvestri L, et al. Endoscopic rendezvous procedure for ureteral iatrogenic detachment: report of a case series with long-term outcomes. J Endourol 2015;29(4):415-20.
5. Liu C, Zhang X, Xue D, et al. Endoscopic realignment in the management of complete transacted ureter. Int Urol Nephrol 2014;46:335-40.
6. Lopatkin NA, Martov AG, Gushchin BL. An endourologic approach to complete ureteropelvic junction and ureteral strictures. J Endourol 2000;14(9):721-6.
7. Macri A, Magno C, Certo A, et al. Combined antegrade and retrograde ureteral stenting: the rendezvous technique. Clinical Radiology 2006;60:257-60.
8. Anderson H, Alyas F, Edwin PJ. Intra-urinoma rendezvous using a transconduit approach to re-establish ureteric integrity. Cardiovasc Intervent Radiol 2005;28:95-7.
9. Gray RJ, Intriere L, Dolmatch BL, et al. Combined retrograde antegrade ureteral stent passage: salvage procedure for a ureteral leak. J Vasc Interv Radiol 1992;3(3):557-8.
10. Delvecchio FC, Kuo RL, Iselin CE, et al. Combined antegrade and retrograde endoscopic approach for the management of urinary diversion associated pathology. J Endourol 2000;14(3):251-6.
11. Postoak D, Simon JM, Monga M, et al. Combined percutaneous antegrade and cystoscopic retrograde ureteral stent placement: an alternative technique in cases of ureteral discontinuity. Urology 1997;50(1):113-16.
12. Doody O, Given MF, Harper M, et al. Rendezvous technique following thermal ureteric injury after radiofrequency ablation in a solitary kidney. J Vasc Interv Radiol 2008;19:1112-14.
Declaration of Competing Interest: None declared.