Peyronie’s disease (PD) describes an acquired disease of the penis, which is characterised by a number of signs and symptoms. These include penile pain, curvature, palpable plaques, wasting or narrowing of the penile shaft, a hinge deformity and potentially catastrophic erectile dysfunction. It is thought to be caused by atypical wound healing, which causes the formation of a fibrous plaque within the tunica albuginea (TA). This article aims to discuss the current understanding about the pathogenesis, management strategies and potential future areas for therapy.
Prevalence
The prevalence rates of PD are estimated to be between 3-9% in adult men [1-3]. However, the rates may be higher in older men and those with co-morbid conditions such as erectile dysfunction (ED) and diabetes [4]. There is also a higher incidence in men following pelvic surgery.
Pathophysiology
The exact aetiology of PD remains elusive. The most accepted theory is that it is caused by penile micro-vascular injury and trauma in men with a genetic predisposition to the condition [4,5]. However, the mechanisms are likely to be multifactorial due to:
- Genetic factors
- Trauma
- Tissue inflammation
- Aberrant wound healing [1].
Injury to the tunica albuginea results in an aberrant inflammatory reaction with release of various growth factors and cytokines [1,5]. These molecular factors lead to a disruption in the normal tissue architecture with dedifferentiation of fibroblasts into myofibroblasts and the persistence of fibrin and collagen. These subsequently contribute to the formation of an inelastic scar (plaque) within the bilayer of the tunica albuginea [1,5]. This has contributed to the modern concept that PD is a disorder of wound healing [5].
Natural History
There are two distinct phases of the condition:
- Acute, inflammatory
- Chronic, fibrotic
The acute phase is characterised by painful erections or penile pain in the flaccid state and an evolving penile curvature [4]. The pain usually resolves by 12-18 months in 90% of men [4,6]. A plaque may be palpable but is often described as soft. The chronic phase is characterised by stable curvature, pain resolution and a hard palpable plaque [4]. PD is a progressive disease with 30-50% of men deteriorating over time and 3-13% reporting spontaneous improvement [7-9].
Management options: medical therapy
Oral treatments
Although oral treatments represent an attractive possibility, the overall data from published series has been disappointing. The studies are often contradictory with methodological issues such as limited number of treated men, short follow-up and variable outcome measures [4,5]. Due to the poor existing data available from these studies, a strong recommendation for any oral medication is not possible; both the European Association of Urology (EAU) and International Consultation on Sexual Medicine (ICSM) do not support their use in clinical practice [4,5].
Intralesional therapy: clostridium collagenase (CCH)
CCH consists of purified enzymes (collagenases I and II) produced by the bacterium clostridium histolyticum. The enzymes selectively hydrolyse types I and III collagen which are the primary component of the PD plaque [5,10-12]. CCH also downregulates many genes and molecular factors involved in the pathogenesis of PD [12].
CCH is the only drug approved by the US Food and Drug Administration (FDA) for the treatment of PD where there is a palpable plaque and a curvature of 30 degrees or greater [1]. It was also approved for use by the European Medicines Agency (EMA) in 2014 [1].
The efficacy has been reported in two large randomised placebo-controlled trials in Europe, New Zealand, Australia and North America (IMPRES I & II) [10-12]. Men were treated with four treatment cycles six weeks apart. Each cycle consisted of two injections. The trials reported a 34% improvement in penile curvature and a significant reduction in the PD bother scores [10,11]. The best results were observed in men with a curvature of less than 60 degrees, absence of plaque calcification and good erectile function [1]. The results of a new modified protocol which aims to reduce patients’ visits and costs has recently been published [12]. The group were able to use one injection per cycle at four weekly intervals. This resulted in the use of a total of three injections of a higher drug concentration (0.9mg vs. 0.58mg) over a 12-week period (vs. 24 weeks in IMPRESS) [12]. The efficacy and safety outcomes were comparable with those observed with the IMPRESS trials [12].
A pooled safety analysis of 1044 treated men across six studies found that most had at least one adverse event [13]. These were generally localised to the penis or groin, were mild or moderate and resolved within 14 days. The most common adverse events observed were:
- Penile haematoma: 50.2%
- Penile pain: 33.5%
- Penile swelling: 28.9%
- Injection site pain: 24.1% [13]
Penile traction devices
The use of traction or vacuum pumps may alter connective tissue as a result of cellular proliferation and expansion of the extracellular matrix [5,14]. Studies have revealed that its regular use may be associated with reduction in penile curvature, increase of flaccid penile length and improvement in penile pain [15-23]. However, more studies are required to define an optimal protocol, the efficacy of the different devices available and which men are most likely to obtain maximal benefit [1].
Management options: surgical therapy
Patient counselling
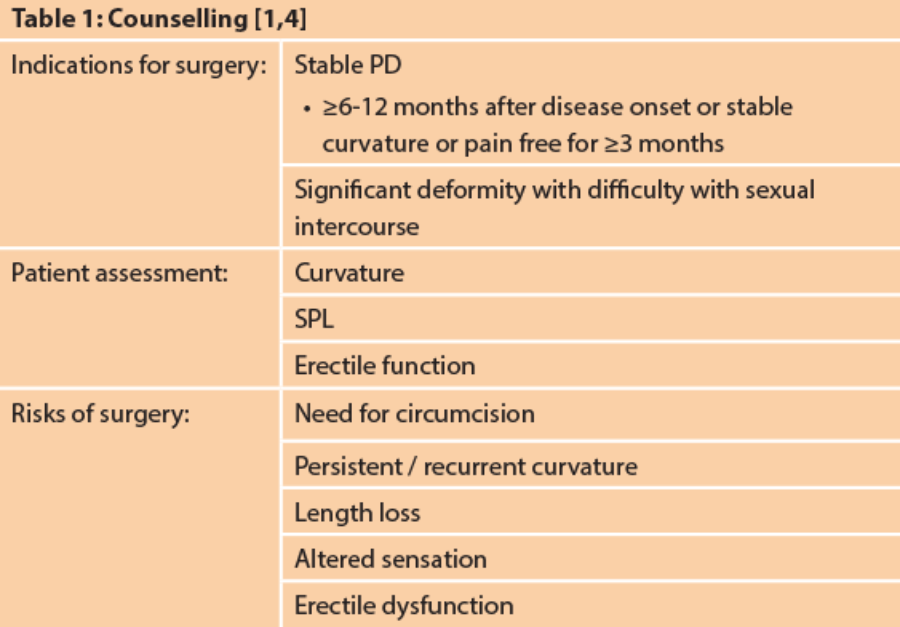
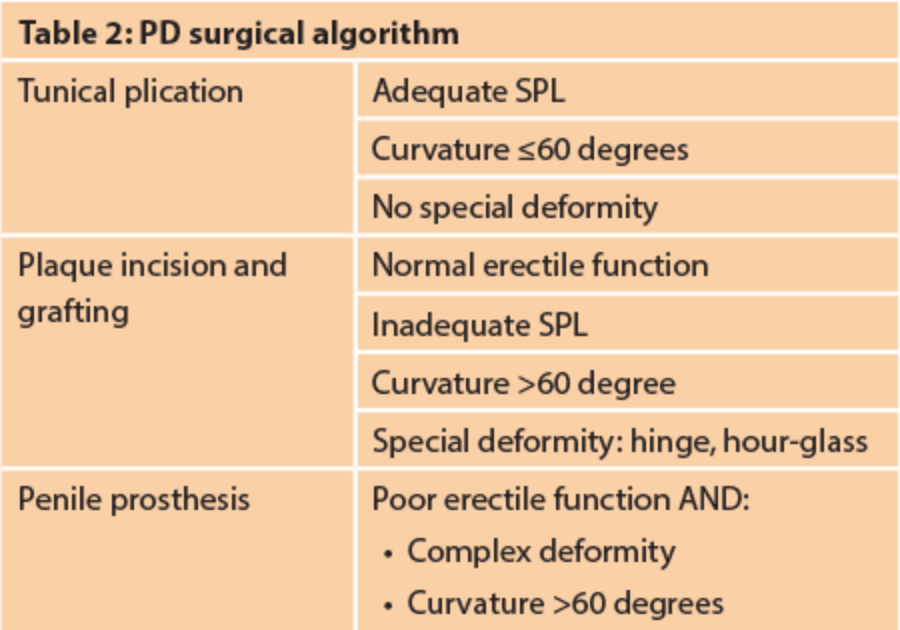
This can be a very difficult group of patients and therefore preoperative counselling is vital before surgical intervention. The indications for surgery and the likely outcomes from surgery must be fully explained to the patient. In particular, penile length loss is a common complaint with PD and this loss is usually not regained with most surgical procedures. We would advise that the exact curvature and stretched penile length (SPL) is documented prior to surgery. The erectile function should be recorded ideally with the use of a validated questionnaire such as the International Index of Erectile Function (IIEF). However, the IIEF is not validated in PD populations. In men with sub-optimal erections, the use of phosphodiesterase type 5 inhibitors (PDE5i) and penile Doppler is useful to determine the degree of vascular ED and whether this can be adequately treated. The aim of surgery is to produce a functionally straight penis, which can be sufficiently turgid to allow penetrative intercourse. Functional straightness is defined loosely as being a residual curvature of less than 20 degrees [1]. Lastly, complications of surgery should be discussed including the possible need for a circumcision.
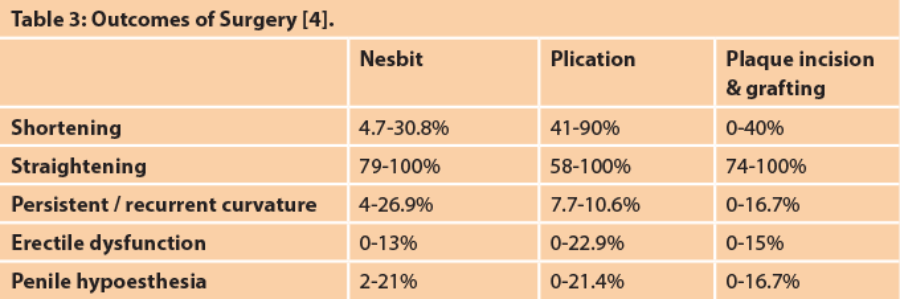
Tunical plication
The first plication technique was described in 1965 by Nesbit [1]. This involved the excision of an ellipse from the tunical albuginea of the convex side of the penis at the level of the maximal curvature followed by closure of the tunical edges with non-absorbable sutures. The original technique has undergone several modifications including the Yachia, 16/24 dot and tunical albuginea plication (TAP) [1]. The Yachia involves either single or multiple small longitudinal incisions in the tunica which are subsequently closed transversely. The main advantage of this approach is that it widens the penis which is a good option if minor waisting or narrowing is present [24]. The 16/24 dot was popularised by Gholami and Lue [1,5]. It involves two or three rows of pairs of plication sutures without any tunical excisions or incisions [1,5]. The TAP technique involves creating a pair of transverse parallel incisions in the tunica. Sutures are then placed from one tunical edge to the other [5].
The major disadvantage of all plication techniques is that they all shorten the long side of the penis to create a straight penis. It is estimated that there is 1cm of length loss for every 20 degrees corrected [24].
Plaque incision and grafting
This involves an incision into the plaque or a partial excision of the plaque. The resultant tunical defect is then covered with a graft; the graft and tunical edges are sutured to each other. There are three types of incision techniques described: double Y, H-shaped and Egydio [1]. The type of graft used is usually surgeon dependant and consists of:
- Autografts
- Allografts / xenografts
- Synthetic grafts
The use of autografts may lengthen operating time while the use of other types of grafts may be associated with increased costs. There is no perfect graft and all are associated with advantages and disadvantages.
The factors associated with poor outcomes from this type of surgery are:
- Preoperative ED
- Large graft used
- Ventral curvature
- Age >60 years [25]
Graft contracture may result in long-term failure leading to re-operation rates of 17% [26]. Most andrologists would therefore advocate a postoperative rehabilitation regime to reduce graft contracture and minimise postoperative ED. This may include penile massage, nocturnal PDE5i and penile traction devices. Penile massage may begin two weeks after surgery twice daily for four to six weeks. PDE5i usage starts one week after surgery and traction devices after three to four weeks [1].
Penile prosthesis
This is an excellent option for men with PD and poor erectile function, which does not respond to medical therapy [5]. The insertion of a penile prosthesis allows for correction of PD curvature and simultaneous treatment of ED [5]. The insertion of an implant may correct the curvature in 58-81% of men [24]. This may be as a result of dissection of tethering fibrotic tissue during corporal dilatation. Men with a residual curvature of 10-20 degrees may be reassured that they will experience further penile straightening with regular cycling of the implant over the following 6-12 months [27-8]. Men with more significant curvature may be corrected with additional manoeuvres which include modelling, releasing incisions and grafting [24].
Modelling was first described by Wilson et al. and involves bending the penis in the contralateral direction to the curvature for 60-90 seconds [29-30]. There is a risk of urethral injury and therefore caution must be exercised with this manoeuvre [24]. Adequate penile straightening may be achieved in up to 89.6% where an inflatable penile prosthesis is placed [31]. Releasing incisions are made when modelling fails to correct a residual significant curvature. This involves incisions made in the tunica on the concave side of the penis [1]. Again, caution must be exercised on this occasion to avoid inadvertent injury to the prosthesis. Lastly, if releasing incisions fail or there is a defect of over 2cm in the tunica, a graft may be placed. This should not be a synthetic graft due to the unacceptably high risk of graft infection or failure which will compromise the longevity of the penile prosthesis [1].
Sliding technique
Penile shortening remains the biggest concern for men undergoing surgery for PD. In addition to the incision and grafting techniques already described as ‘lengthening procedures’, surgical techniques to give extra length have also been explained. The earliest descriptions were published in 1995, detailing circumferential albugineal incisions, followed by the traction of the glans until the maximum stretch of the NVB is achieved [32]. Good results have been described with this procedure. Rolle et al. have recently reported a personal modification of this surgical approach, the so-called ‘sliding technique’ [32]. A double ventro-dorsal incision of the tunica albuginea connected to two longitudinal incisions was described. In addition to providing early stabilisation of the shaft placing two absorbable sutures laterally on the two longitudinal sides, this approach allowed for stabilisation of the shaft during the dilation required for the penile prosthesis implantation. This reduced the risk of stretching both the NVB and the urethra [33]. There is significant risk of vascular compromise with these procedures and patients must be warned about the growing descriptions of the necrotic glans and lost penis.
However, these techniques are complex and difficult procedures to carry out. We recommend that they should ideally be performed in high-volume, expert centres.
Stem cell research
There is increasing focus on the use of stem cells (SC) in the treatment of a variety of acquired pathologies with the body. SCs have been shown in the preclinical setting to counteract fibrosis acting in multiple steps. This characteristic makes SCs potentially an exciting treatment modality in PD.
Adipose stem cells (ADSC) have been injected into the tunica albuginea of rats, who have experimentally induced PD. Five weeks after the ADSC local injection into the site of inflammation, the rats had less elastosis and fibrosis of the TA compared to the untreated rats and, surprisingly, no erectile dysfunction [34]. Although much of the research on SCs has been shown to possibly prevent the infiltration of TA fibrosis, there are only a few experimental studies showing that the SCs treatment is efficacious to reverse TA fibrosis.
Stem-cell therapy offers a promising new treatment, but is yet to be licensed or used in the clinical setting.
Conclusion
Peyronie’s is a complex disease process, with a variety of presentations and level of bother caused. It can be associated with significant psychosexual anxiety in men, and the treatments themselves can also have considerable impact on the psychological wellbeing of the patient. This must all be put into context in the initial consultation and treatment plan.
The exact aetiology is unclear but there does appear to be a genetic predisposition in men, who appear to have an abnormal response to microvascular trauma during sexual activity.
“Peyronie’s is a complex disease process, with a variety of presentations and level of bother caused.”
Evidence is poor for oral pharmacological treatments and tends to concentrate on use in early stages of the disease. There is level 1b evidence for the use of oral treatment with potassium para-ambinobenzoate for treating penile pain as well as aiding stabilisation of the penile curvature, however it is not currently recommended by the EAU guidelines. Vacuum pumps and manual traction devices have been shown to have some use but rely on patients to use them regularly and can impact on daily life significantly.
Stem cell treatment has shown promising results in rat models but further research in humans is needed.
Intralesional injections with CCH are the only FDA-approved drug for treatment of PD, and have been shown to improve penile curvature and symptom bother.
Surgical repair may be indicated in men whose curvature and pain is stable. We would recommend surgery be reserved for men who find sexual intercourse difficult due to their level of curvature. The type of surgery depends on the level of curvature present and the degree of erectile dysfunction. Procedures range from simple plications to more extensive sliding techniques / penile prosthesis insertion which should be carried out at high volume centres due to the risks and complications involved.
References
1. Chung E, Ralph D, Kagioglu A, et al. Evidence based guidelines on Peyronie’s disease. JSM 2016;13:905-23.
2. Schwarzer U, Sommer F, Klotz T, et al. The prevalence of Peyronie’s disease: Results of a large survey. BJU Int 2001;88:727-30.
3. Mulhall J, Creech S, Boorjian S, et al. Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol 2004;171:2350-3.
4. Hatzimouratidis K, Giuliano F, Moncada I, et al. EAU guidelines on erectile dysfunction, premature ejaculation, penile curvarture and priapism.
www.uroweb.org/wp-content/
uploads/EAU-guidelines-male
-sexual-dysfunction-2016-3.pdf.
5. Levine LA, Burnett AL. Standard operating procedures for Peyronie’s disease. J Sex Med 2013;10:230-44.
6. Hartzell R. Psychosexual symptoms and treatment of Peyronie’s disease within a collaborative care model. Sex Med 2014;2:168-77.
7. Kadioglu A, et al. A retrospective review of 307 men with Peyronie’s disease. J Urol 2002;168:1075.
8. Gelbard MK, et al. The natural history of Peyronie’s disease. J Urol 1990;144:1376.
9. Mulhall J, et al. An analysis of the natural history of Peyronie’s disease. J Urol 2006;175:2115.
10. Levine LA, Cuzin B, Mark S, et al. Clinical safety and effectiveness of collagenase clostridium histolyticum injection in patients with Peyronie’s disease: A phase 3 open-label study. J Sex Med 2015;12:248-58.
11. Gelbard M, Goldstein I, Hellstrom W, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie’s disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. JU 2013;190:199-207.
12. Raheem A, Capece M, Kalejaiye O, et al. Safety and effectiveness of collagenase clostridium histolyticum (CCH) (Xiapex®) in the treatment of Peyronie’s disease using a new modified shortened protocol. BJU Int [Epub ahead of print].
13. Carson CC 3rd, Sadeghi-Nejad H, Tursi JP, et al. Analysis of the clinical safety of intralesional injection of collagenase Clostridium histolyticum (CCH) for adults with Peyronie’s disease (PD). BJU Int 2015;116:815.
14. Chung E, De Young L, Solomon M, et al. Peyronie’s disease and mechanotransduction: An in vitro analysis of the cellular changes to Peyronie’s disease in a cell-culture strain system. J Sex Med 2013;10:1259-67.
15. Hellstrom W, Montague DK, Moncada I, et al. Implants, mechanical devices, and vascular surgery for erectile dysfunction. J Sex Med 2010;7:501.
16. Martinez-Salamanca JI, Egui A, Moncada I, et al. Acute phase Peyronie’s disease management with traction device: a nonrandomized prospective controlled trial with ultrasound correlation. J Sex Med 2014;11:506.
17. Raheem A, Garaffa G, Raheem T, et al. The role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s disease. BJUI 2010;106:1176-80.
18. Abern M, Levine LA. Intralesional injections with and without penile traction and oral therapies for management of Peyronie’s disease. J Urol 2008;179:408.
19. Abern M, Larsen S, Levine L. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie’s disease. J Sex Med 2012;9:288-95.
20. Gontero P, Di Marco M, Guibilei G, et al. A pilot phase II prospective study to test the ‘efficacy’ and tolerability of a penile extender device in the treatment of ‘short penis’. BJU Int 2009;103:793-7.
21. Gontero P, Di Marco M, Guibilei G, et al. Use of penile extender device in the treatment of penile curvature as a result of Peyronie’s disease. Results of a phase II prospective study. J Sex Med 2009;6:558-66.
22. Levine L, Newell M, Taylor F. Penile traction therapy for treatment of Peyronie’s disease: A single-center pilot study. J Sex Med 2008;5:1468-73.
23. Yafi F, Pinsky M, Stewart C, et al. The effect of duration of penile traction therapy in patients undergoing intralesional injection therapy for Peyronie’s disease. J Urol 2015;194:754-8.
24. Garaffa G, Kuehhas F, De Luca F, et al. Long-term results of reconstructive surgery for Peyronie’s disease. Sex Med Rev 2015;3:113-21.
25. Mulhall, J, Anderson M, Parker M. A surgical algorithm for men with combined Peyronie’s disease and erectile dysfunction: functional and satisfaction outcomes. J Sex Med 2005;2:132.
26. Chun J, McGregor A, Krishnan R, Carson CC. A comparison of dermal and cadaveric pericardial grafts in the modified Horton-Devine procedure for Peyronie’s disease. J Urol 2001;166:185.
27. Levine L, Benson J, Hoower C. Inflatable penile prosthesis placement in men with Peyronie’s disease and drug resistanterectile dysfunction: A single center study. J Sex Med 2010;7:3775–83.
28. Garaffa G, Minervini A, Christopher N, et al. The management of residual curvature after penile prosthesis implantation in men with Peyronie’s disease. BJU Int 2011;108:1152-6.
29. Bonillo M, Garaffa G, Ralph D. Addressing residual penile deformity in the Peyronie’s disease patient during penile implant surgery. Current Sexual Health Report 2007;4:163-6.
30. Wilson SK, Carson CC. Surgical straightening with penile prosthesis. In: Levine L, Tolowa NJ (Eds.). Peyronie’s disease. A guide to clinical management. New York, USA; Humana Press; 2007:249-58.
31. Hsu G, Chen H, Hsieh C, et al. Long-term results of autologous venous grafts for penile morphological reconstruction. J Androl 2007;28:186-93.
32. Rolle L, Ceruti C, Timpano M, et al. A new, innovative, lengthening surgical procedure for peyronie’s disease by penile prosthesis implantation with double dorsal-ventral patch graft: the “sliding technique.” J Sex Med 2012;9(9):2389–95.
33. Rigaud G, Berger R. Corrective procedures for penile shortening due to Peyronie’s disease. J Urol 1995;153(2):368-70.
34. Castiglione F, Hedlund P, Van der Aa F, et al. Intratunical injection of human adipose tissue-derived stem cells prevents fibrosis and is associated with improved erectile function in a rat model of Peyronie’s disease. Eur Urol 2013;63:551-60.
Declaration of competing Interests: David Ralph - Consultant for Coloplast, Boston Scientific and Sobi Pharmaceuticals.