Purple urine bag syndrome (PUBS) is an uncommon phenomenon where the tubing and urinary catheter bag is noticed to undergo purple discolouration. This has been linked with urinary tract infections (UTI), chronic debilitated states and prolonged catheterisation.
PUBS was noticed a long time ago, as doctors tending to King George III recorded blue urine during a bout of constipation. This has historically been ascribed to porphyria, medication containing gentian and chronic constipation [1]. However, it was not until 1978 that the phenomenon was reported in the medical literature [2]. Although uncommon, some reports suggest a prevalence of 9.8% or higher in institutionalised patients with long-term urinary catheters [3].
Purple urine bag syndrome is typically a complication of urinary tract infections with bacteria which metabolise products of tryptophan to produce red and blue pigments. Several bacteria have been implicated, mostly gram negative, and include Providencia stuartti and rettgeri, Pseudomonas aeruginosa, Proteus mirabilis, Escherichia coli, Klebsiella pneumoniae, Enterococci, Morganella, Citrobacter species, and Group B Streptococci. These bacteria produce indoxyl phosphatase or sulphatase, an enzyme that converts indoxyl sulphate (a tryptophan metabolite) for indirubin (coloured red) and indigo (coloured blue). These two substances, when mixed, produce purple coloration of the urine [1,4,5].
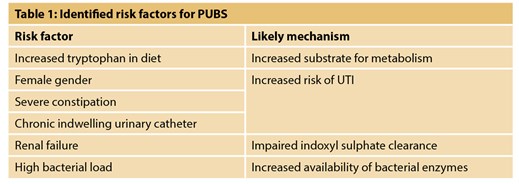
Identified risk factors implicated are in Table 1. Much of this is evidenced from case reports. Increased intake of tryptophan in the diet increases the substrate for PUBS-causing bacteria and alkalinised urine facilitates the oxidation of indoxyl sulphate although the latter may not always be a requirement as evidenced by a case report of PUBS in acidic urine [6]. Elderly individuals with multiple co-morbidities are more likely to be catheterised long-term, which increases their risk of urinary infection, with an added inherent risk from female urinary anatomy. Chronic renal failure and haemodialysis [7], nephrostomy tubes and ileal conduits have been associated from case reports [8]. Severe constipation may predispose to urinary retention as well as increase faecal bacterial load. Long-term catheters are well known to increase the risk of UTI, but PUBS seem to be more common in those in whom polyvinylchloride (PVC) catheters have been used [9].
Although PUBS is a relatively easy spot diagnosis provided the clinician is aware of the phenomenon, it may be misdiagnosed if other causes of urine discolouration are not taken into consideration and excluded. Urine may be discoloured by food (e.g. beetroot), drugs (e.g. rifampicin), poisons, porphyria, alkaptonuria, myoglobinuria, rhabdomyolysis and haematuria; it follows therefore that these require different investigations and treatments. These can be ruled out by taking a medical history and basic laboratory diagnostics. In our recent experience we encountered a 75-year-old diabetic with a long-term catheter who presented with purple urine associated with pseudomonas urinary infection (Figure 1).

Figure 1.
A careful history and basic diagnostic work-up are key to successful management. Establishing a timeline may identify an association with dietary factors, and other symptoms may provide clues to an alternative diagnosis. Medication history is extremely important. Urinalysis and microbiology and a blood screen will usually confirm the diagnosis. Catheter-associated UTI is managed as per guidelines, typically with antibiotics guided by urine culture sensitivities, catheter change for non-PVC catheters and bags, reinforcement of good catheter hygiene, and addressing underlying risk factors such as constipation. There are no guidelines for the management of PUBS, which has to be individualised.
The question remains as to whether asymptomatic individuals with PUBS need to be treated. It has been suggested that PUBS may be associated with increased chances of morbidity and mortality than UTIs without PUBS [10], and cases have been reported of PUBS concurrent with Fournier’s gangrene that required aggressive debridement [11]. Consequently therefore, although in the majority of individuals PUBS follows a benign course, it may not always do so.
References
1. Arnold WN. King George III’s urine and indigo blue. The Lancet 1996;347(9018):1811-3.
2. Barlow GB, Dickson JAS. Purple urine bags. The Lancet 1978;28:220-1.
3. Dealler SF, Belfield PW, Bedford M, et al. Purple urine bags. Journal of Urology 1989;142(3):769-70.
4. Pankau EF. Purple urine bags. J Urol 1983;130:372.
5. Fain-Ghironu N, Le Gondiec P, Schaeffer M. Purple urine bag syndrome. Presse Med 2003;32:985-7.
6. Chung SD, Liao CH, Sun HD. Purple urine bag syndrome with acidic urine. International Journal of Infectious Diseases 2008;12(5):526-7.
7. Aycock RD. A case of purple urine bag syndrome in a patient with an ileal conduit. International Urology and Nephrology 2010;2(4):580-3.
8. Su FH, Chung SY, Chen MH, et al. Case analysis of purple urine-bag syndrome at a long-term care service in a community hospital. Chang Gung Medical Journal 2005;28(9):636-42.
9. Pillai RN, Clavijo J, Narayanan M, Zaman K. An association of purple urine bag syndrome with intussusception. Urology 2007;70(4):812.e1-812.e2.
10. Pillai BP, Chong VH, Yong AML. Purple urine bag syndrome. Singapore Medical Journal 2009;50(5):e193-4.
11. Tasi YM, Huang MS, Yang CY, et al. Purple urine bag syndrome, not always a benign process. The American Journal of Emergency Medicine 2009;27(7):895-7.
Declaration of competing interests: None declared.