Human health is intrinsically linked to environmental health, making the ever-pressing climate crisis fundamentally a public health emergency. The healthcare sector is responsible for 8% of the UK’s greenhouse gas (GHG) emissions worldwide [1]. As the largest publicly funded healthcare system globally, the NHS has a responsibility to lead the international push for better environmental sustainability.
Approximately 62% of the NHS carbon footprint comes from its supply chain, whilst 24% arises from the delivery of care, and 10% from staff and patient-related travel [1]. In 2020 NHS England issued the target to become carbon ‘net zero’ by 2050. To address this challenge, they utilised the three GHG protocol (GHGP) scopes, which reflect the source and aid measurement of GHG emissions (Table 1).
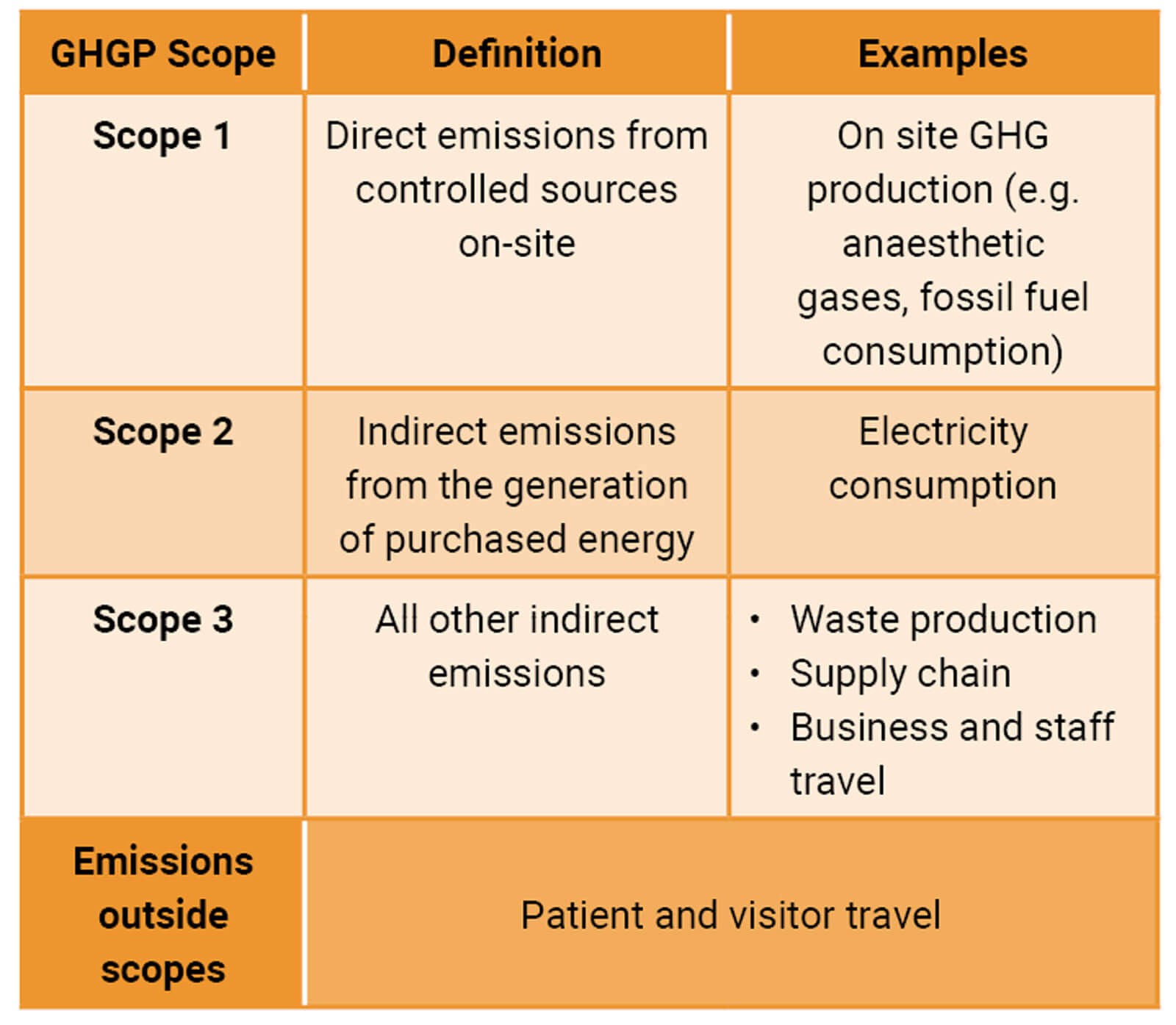
Table 1: Key components of the NHS Carbon Footprint [2].
Scope 1 encompasses direct emissions from controlled sources on-site, such as use of anaesthetic gases and fossil fuel consumption. Scope 2 covers indirect emissions from the generation of purchased energy. Scope 3 includes all other indirect emissions, such as emissions from the supply chain, medical waste, and water usage [2]. The GHGP scopes allow global standards to be set and international comparisons to be made, offering an efficient mechanism to evaluate the healthcare sector’s carbon footprint. The term ‘carbon dioxide equivalent’ (CO2e) is often used to quantify the global warming impact of different GHG emissions collectively as one common unit. Whilst individual trusts and specialties contribute relatively minor amounts to overall emissions, all have a role in reducing their own ‘footprint’. Surgical specialities such as urology are resource intensive, with high energy consumption and waste production through operating theatres, diagnostics and outpatient activity. Urology is in an optimal position to make changes and an impact through climate-smart actions to reduce their environmental burden.
Scope 1: Direct emissions from the operating theatre
Approximately 17% of the healthcare sector’s carbon footprint originates directly from healthcare sites [3]. Up to half of the contributions from the operating theatre are due to use of volatile anaesthetic gases, such as desflurane and nitrous oxide which are potent GHGs. One direction to reduce urology’s environmental impact is to work with anaesthetic colleagues to increase the use of spinal anaesthetic, propofol-based intravenous anaesthesia and to introduce new technologies to facilitate greater use of local anaesthetic (LA). There are already numerous examples of a shift away from general anaesthesia within urology, with the potential to go further. Most cystoscopy procedures can be performed using intraurethral lidocaine gels, LA blocks or intravenous sedation. One example highlighted in the Getting It Right First Time (GIRFT) report in 2022 was transurethral laser ablation (TULA®) of non-muscle invasive bladder cancer under LA, which the report suggests should be accessible in all units.
Use of this technique in outpatients would reduce the impact from treatment duration and hospital admissions and thereby reduce GHG emissions. Symptomatic benign prostatic hyperplasia (BPH) is a further area where change to practice could lead to environmental benefits. New emerging technologies for surgical treatment of BPH including Rezum™, Urolift® and prostatic artery embolisation, can all be performed in an outpatient setting. Robotic-assisted and minimally invasive surgery (MIS) forms a large part of urological operating time, and it has been assumed that use of CO2 for insufflation would increase the CO2e production. However, there is surprisingly little data on this, and it remains unknown as to the environmental impact of MIS. With up to 84% of NHS robotic procedures performed by urologists, the speciality should lead on data acquisition to establish practices to ensure CO2e remains ‘as low as reasonably achievable’ during MIS [4].
Scope 2: Electricity consumption
The operating theatre is three to six times more resource intensive than the rest of a hospital, due to the need for stringent heating, ventilation, lighting and equipment [5]. This carbon footprint can be reduced through attention to simple strategies, including turning off lights and equipment, keeping doors closed and utilising power save modes. Initiated in 2013, Barts Health NHS Trust and Global Action Plan undertook a behaviour modification programme titled ‘Operation TLC: turn off, lights out, close doors’. This programme involved staff education and commitment to simple climate-smart behaviour changes, for example, using energy saving methods in theatre during unoccupied periods. It demonstrated reduced CO2e emissions of 2200 tonnes / year, in addition to a significant financial benefit saving the trust £105,000 a year [6]. Appropriate energy saving steps should be taken when using energy-intensive specialist equipment, such as the lasers used by urology, to ensure ‘as low as reasonably achievable’ in all cases. Additionally, new technology, including the thulium lasers, may help reduce energy consumption [7].

Simple steps such as ensuring theatre lights are switched
off when not in use should become routine.

Discarded irrigation bags that could have been recycled.
Cross-sectional imaging consumes a huge amount of energy and its use within urology is expanding. An obvious example of this is the increased use of multiparametric MRI in the diagnosis and surveillance of prostate cancer. Ultrasound scanning (USS) consumes less energy in both production and medical use as compared to CT and MRI. USS produces approximately 1kg CO2e per abdominal examination, compared to abdominal CT producing 6kg and MRI 20kg [8]. The increased use of MRI within urology comes with a significant carbon burden which should be considered as new imaging protocols are developed. To help aid sustainability, urological departments should minimise unnecessary imaging and opt for USS if clinically feasible. Improvements in the resolution of USS have enhanced its utility in diagnostic and interventional urology. Novel USS-based modalities including elastography, contrast enhanced (CEUS), computer assisted, and 3D ultrasound are now accessible to urologists [9]. Evidence is accruing for their role as an alternative to CT or MRI in areas such as CEUS in renal tumour ablation procedures [10].
Scope 3: Other indirect emissions
Medical waste is an escalating problem, with the operating theatre generating 20-33% of a hospital's total waste [11]. Whilst 85% of the waste is classed as non-hazardous, up to 90% of this is incorrectly disposed of in the operating theatre [12,13]. This is a particular problem within urology due to the high use of plastic irrigation containers, generating substantial waste that could be recycled. In Newcastle, the Freeman Hospital undertook a theatre recycling project in 2017, which involved staff education and adding specific blue bags into urology theatres to enable recycling of fluid bags. Over one year, the project resulted in recycling of 1.85 tonnes of plastic that would have been incinerated previously. Similarly, at the annual BAUS meeting in 2022, the team from Raigmore Hospital examined the environmental impact of irrigation fluid disposal in urology theatres. Through the use of a dedicated fluid waste management system, 3203kg of CO2e emissions were saved over eight months [14].
Evidence for the environmental benefit of reusable versus single-use devices has been demonstrated and the government has encouraged less reliance on single-use products [2]. However, these remain widespread in urology with ureteroscopes and cystoscopes increasingly being single use. The companies selling reusable devices emphasise the benefits in terms of sterility and infection risk but often downplay the environmental burden. Whilst the carbon footprint of a reusable flexible cystoscope was found to be approximately five times lower than a single-use disposable cystoscope [15], there is an apparent paradox, relating to high energy cost of re-sterilisation of reusable equipment. Indeed, the literature available on the carbon footprint of reusable scopes remains unclear. Going forwards any case for new urological equipment must consider its environmental impact including the efficiency of a trust’s sterilisation process. Much of the waste from medical devices comes from disposal of the plastic packaging. Waste and sterilisation costs may be reduced through vigilant operating theatre practice, to ensure packaging is only opened when it is required [16].
One exciting area for urology is the development of biodegradable devices. Urology uses a high number of plastic-based, non-reusable indwelling prostheses, including urethral catheters and ureteric stents. The option of making these biodegradable is attractive clinically and environmentally. The first biodegradable urethral catheter (EmtevaPure®) has been developed, which dissolves in water reducing the environmental impact from disposal of standard catheters. In addition, preliminary work on animal models has shown the feasibility of developing biodegradable ureteric stents, which could reduce environmental impact as well as reducing infection and the risk of ‘forgotten’ stents [17].
Travel
The NHS accounts for 5% of all road transport emissions in the UK [2]. The GIRFT report (2022) highlighted key components in optimising outpatient experience and outcomes, with an emphasis on supporting sustainability and reducing travel. Catalysed by the COVID-19 pandemic, virtual consultations and monitoring have become important components of this. Remote monitoring and at-home assessment of patients will reduce travel and allow follow-up to be initiated when clinically indicated. During the pandemic, virtual clinic consultations rose from 1% to 70% [18]. Urology can embrace what was learned and optimise use of virtual assessments where appropriate. To further reduce travel and maximise efficiency, urology outpatients present an ideal setting to configure one-stop assessment and diagnostic clinics [19]. Progressive developments such as these could potentially be wheeled out internationally. One final consideration must be to reduce travel to conferences and meetings. Whilst there may be personal and academic benefits for face-to-face meetings, videoconferencing, webinars, and online lectures can arguably all provide the same educational component without the need for national and international travel.
Conclusion
Environmental sustainability is becoming an increasingly relevant and important topic to current and future generations of doctors. There has been a positive shift in attention towards evaluating medical practice, technology, and procedures with a goal of reducing GHG contributions. Each trust, specialty and clinician have responsibilities to help achieve the goal of a ‘net zero’ healthcare system. Although there remain challenges within urology from increased use of high energy cross-sectional imaging and advanced surgical technology, the specialty is well positioned to evaluate and adapt practice to achieve sustainability. Whilst many of the mentioned strategies may seem minor, particularly compared to the environmental burden of the healthcare supply chain, they represent marginal changes which over time and nationally would amass to substantial improvements in sustainability.
TAKE HOME MESSAGE
-
Climate change is an ever-pressing public health emergency and the healthcare sector itself is a significant contributor to worldwide greenhouse gas emissions.
-
Surgical specialties such as urology are resource intensive, and therefore play a vital role in reducing the sector’s carbon footprint.
-
Urology can make a positive impact through sustainable use of new technology, recycling and waste reduction within operating theatres, and simple climate-smart behavioural modifications such as turning off lights.
-
Further research is required to determine the environmental impact of single use scopes and robotic surgery within urology.
-
Alongside patient safety and cost-effectiveness, environmental burden of current and future technologies, products and procedures needs to be evaluated.
References
1. Tennison I, Roschnik S, Ashby B, et al. Health care's response to climate change: A carbon footprint assessment of the NHS in England. Lancet: Planetary Health 2021;5(2):e84-e92.
2. NHS England. Delivering a ‘Net zero’ national health service. 2020.
https://www.england.nhs.uk/greenernhs/
wp-content/uploads/sites/51/2020/10/
delivering-a-net-zero-national-health-service.pdf
[Accessed 20 January 2022].
3. Healthcare Without Harm and ARUP. Health care's climate footprint: How the health sector contributes to the global climate crisis and opportunities for action. 2019.
https://noharm-global.org/sites/
default/files/documents-files/5961/
HealthCaresClimateFootprint_092319.pdf
[Accessed 1 February 2022].
4. Lam K, Clarke J, Purkayastha S, Kinross JM. Uptake and accessibility of surgical robotics in England. Int J Med Robot 2021;17(1):1-7.
5. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: A carbon footprinting study of operating theatres in three health systems. Lancet: Planetary Health 2017;1(9):e381-8.
6. Major J, Puddy E. Sustainability: Energy use and water consumption. 2020.
https://www.rcoa.ac.uk/sites/
default/files/documents/2021-12/Energy
%20use%20and%20water%
20consumption%20final.pdf
[Accessed 13 February 2022].
7. Kronenberg P, Traxer O. The laser of the future: Reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol 2019;8(Suppl 4):S398-417.
8. Martin M, Mohnke A, Lewis GM, et al. Environmental impacts of abdominal imaging: a pilot investigation. J Am Coll Radiol 2018;15(10):1385-93.
9. Fulgham PF, Loch T. Standards, innovations, and controversies in urologic imaging. World J Urol 2018;36(5):685-6.
10. Lal A, Naranje P, Pavunesan SK. What's new in urologic ultrasound? Indian J Urol 2015;31(3):176-84.
11. Wyssusek KH, Foong WM, Steel C, Gillespie BM. The gold in garbage: Implementing a waste segregation and recycling initiative. AORN J 2016;103(3):316.e1-.e8.
12. WHO. Health-care waste. 2018.
https://www.who.int/news-room/
fact-sheets/detail/health-care-waste
[Accessed 31 January 2022].
13. Harding C, Van Loon J, Moons I, et al. Design opportunities to reduce waste in operating rooms. Sustainability 2021;13(4):2207.
14. Gunner C, Barker K, Ramsey S. Reducing the environmental impact of fluid waste disposal in urology. J Clin Urol 2022;15(1S):3-95.
15. Koo K, Winoker J, Patel S, et al. The cost of convenience: Estimating the environmental impact of single-use and reusable flexible cystoscopes. J Urol 2021;206(Supplement 3):e683-4.
16. Pradere B, Mallet R, de La Taille A, et al. Climate-smart actions in the operating theatre for improving sustainability practices: A systematic review. Eur Urol 2022 [Epub ahead of print].
17. Soria F, de La Cruz JE, Caballero-Romeu J, et al. Comparative assessment of biodegradable-antireflux heparine coated ureteral stent: Animal model study. BMC Urol 2021;21(1):32.
18. Marshall T. How can we be SMART with virtual consultations? ENT & Audiology News 2020;29(5):35.
19. Coull N, Rottenberg G, Rankin S, et al. Assessing the feasibility of a one-stop approach to diagnosis for urological patients. Ann R Coll Surg Engl 2009;91(4):305-9.
Declaration of competing interests: None declared.
Acknowledgement: This review article is based upon the author's winning BAUS Medical Student Essay 2022 entitled 'The healthcare sector generates about 8% of our greenhouse gases, with much coming from the operating theatre. What steps can urology as a specialty take to become more sustainable?'.







