Epidemiology
Extramammary Paget’s disease (EMP) is a rare intraepithelial neoplasm, which is rarely invasive and has an incidence of six per million person-years as calculated by a European SEER analysis [1]. It usually affects apocrine gland-bearing areas, especially the vulvar, perianal skin and axilla, but peno-scrotal EMP accounts for only 14% of reported cases [2-5]. The first description of penoscrotal EMP was by Crocker in 1889 [3]. From 1973 to 2007 the European SEER analysis found 197 cases of scrotal and 82 cases of penile EMP [1].
Clinical presentation
EMP of the peno-scrotal area is frequently misdiagnosed as other benign skin conditions such as seborrheic dermatitis, contact dermatitis, lichen sclerosus, Bowen disease, eczema, psoriasis or a superficial fungal infection [2,3,6]. It usually appears as a well-circumscribed erythematous pruritic plaque which can also ulcerate, bleed and form crusts (Figure 1). It can sometimes be present for over a decade before it undergoes malignant transformation [4]. Published cases in the literature report a prolonged failed treatment period with topical steroids in primary care prior to referral to dermatology specialists, where the diagnosis is made [3-5].
Figure 1.
Diagnosis and histopathology
Diagnosis of EMP is preceded by a high index of suspicion and diagnostic biopsy with immunohistochemistry [2,6]. Microscopically EMP is characterised by the presence of Paget cells which are atypical glandular-like cells, larger than keratinocytes with a granular amphophilic to basophilic cytoplasm, round or oval nucleus and with one or more prominent nucleoli [7,8] (Figure 2). They form nests in the basal and parabasal zones of the skin [7,8].
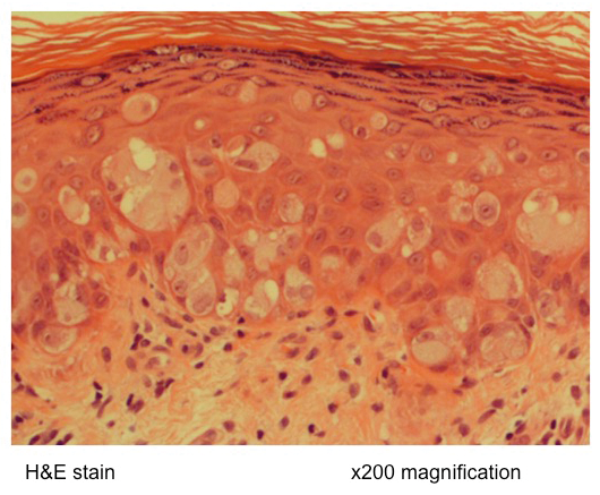
Figure 2.
Immunohistochemistry usually tests positive for haematoxylin and eosin which differentiates EMP from malignant melanoma and Bowen’s disease [7,8]. Immunohistochemical tests provide the definitive diagnosis as well as ensuring clear surgical margins following surgical excision. They show a positive staining for CK7 and consistently negative staining for high-molecular-weight cytokeratins [4,6,9].
Investigations
Staging and screening investigations include CT imaging and endoscopic evaluation of the large bowel and urinary tract. Peno-scrotal EMP has been associated with cancers of the urinary and gastrointestinal tract in approximately 11% of cases [2,3,5].
Management
EMP of the peno-scrotal area should be managed in a tertiary centre with expertise in this condition, as no clear diagnostic and treatment guidelines are currently available.
Following the histological diagnosis, all cases are reviewed in a multidisciplinary setting with input from dermatologists, plastic surgeons and urologists depending on the expertise for peno-scrotal reconstruction.
Wide local excision of the lesions with reconstruction combined with frozen section analysis of mapped biopsies adjacent to the resection margins or Mohs micrographic surgery can reduce the risk of residual disease and therefore local recurrence [2,3,5]. Often the adjacent skin may look macroscopically normal but still contain Paget cells. Recurrence rates range from 16-25% and adjuvant treatment with topical agents such as 5-fluorouracil (5-FU), 5% Imiquimod cream or laser vaporisation and photodynamic therapy can be used in non-invasive lesions [3,5-8].
Invasive EMP is usually an adenocarcinoma and once lymphovascular invasion occurs, the prognosis is poor [2,3]. Surgical lymphadenectomy is indicated in cases of infiltrative disease or suspicious metastases to the groins without evidence of spread to the pelvic nodes but in cases of disseminated malignant disease radiotherapy and systemic chemotherapy should be considered [8,10].
Options for metastatic disease have been reported with limited response [1]. Chemotherapy regimens reported in the literature include systemic 5-FU with mitomycin C, Carboplatin plus 5-FU and Leucovorin, low dose 5-FU and cisplatin, docetaxel, mitomycin C plus epirubicin, vincristine and cisplatin, and 5-FU alone [2,10]. Establishing whether HER2, ER and PR factors are expressed in the immunohistochemistry are important and can assist in selecting the appropriate chemotherapy agents [8].
Conclusion
EMP disease is rare and requires a high index of suspicion. Although non-invasive disease can be surgically excised, the options for metastatic disease are limited with a poor prognosis. Patients require endoscopic evaluation of the gastrointestinal tract and urinary tract.
TAKE HOME MESSAGE
-
In the early stages of peno-scrotal extramammary Paget’s disease, the appearance is similar to eczema. Clinicians should seek specialist input such as a dermatologist with experience in genital dermatological diseases when the lesion fails to respond to topical steroid treatments
-
Due to the rare incidence of this disease no clear diagnostic and treatment guidelines are available and long-term follow-up in a specialised centre is required to monitor for progression to invasive carcinoma as well as other EMP-associated malignancies
References
1. Master VA, Herrel L, Johnson TV, Delman KA. Extramammary Paget’s disease of the penis and anogenital area: seer analysis. J Clin Oncol 2011;29(Suppl 7): Abstract 220.
2. Beleznay KM, Levesque MA, Gill S. Response to 5-fluorouracil in metastatic extramammary Paget disease of the scrotum presenting as pancytopenia and back pain. Curr Oncol 2009;16(5):81-3.
3. Ekwueme KC, Zakhour HD, Parr NJ. Extramammary Paget’s disease of the penis: a case report and review of the literature. J Med Case Rep 2009;3:4.
4. Isrow D, Oregel KZ, Cortes J, et al. Advanced extramammary paget’s disease of the groin, penis, and scrotum. Clin Med Insights Oncol 2014;8:87–90.
5. Kanitakis J. Mammary and extramammary Paget’s disease. J Eur Acad Dermatol Venereol 2007;21:581–90.
6. Quinn AM, Sienko A, Basrawala Z, Campbell SC. Extramammary Paget Disease of the Scrotum With Features of Bowen Disease. Arch Pathol Lab Med 2004;128:84–6.
7. Londero AP, Bertozzi S, Salvador S, et al. A review of extramammary paget’s disease: Clinical presentation, diagnosis, management and prognosis. J Med Med Sci 2013;4(4):134-48.
8. Moretto P, Nair VJ, El Hallani S, et al. Management of penoscrotal extramammary Paget disease: case series and review of the literature. Curr Oncol 2014;20(4):e311-20.
9. Li Y-C, Lu L-Y, Yang Y-T, et al. Extramammary Paget’s disease of the scrotum associated with hepatocellular carcinoma. J Chin Med Assoc 2009;72(10):542–6.
10. Parada D, Moreira O, López C, et al. Extramammary Paget’s disease of scrotum: a case with local lymph node metastasis. Arch Esp Urol 2005;58(1):85-9.





