The widespread use of prostate specific antigen (PSA) testing has led to diagnostic difficulties for patients and urologists. The sensitivity and specificity characteristics of PSA are far from optimal. To try and improve the predictive accuracy of PSA measurements, nomograms and artificial neural networks have been created by various groups across the world.
By combining PSA measurements with various examination and investigation findings these predictive models have shown to be superior to PSA alone [1]. Initially these models were available as paper-based nomograms or as calculators via the internet but now this form of prediction can be produced on any smartphone or tablet.
One of the app’s creators, Dr Monique J Roobol, Erasmus University Medical Centre, Netherlands and the lead author on many of the publications relating to the prostate cancer risk calculator.
Rotterdam Prostate Cancer Risk Calculators (RPCRC)
The Rotterdam Prostate Cancer Risk app was released through the Prostate Cancer Research Foundation, Rotterdam (SWOP), in partnership with the European Randomized Study of Screening for Prostate Cancer (ERSPC). The app can be downloaded as a smartphone or tablet app, available on Android or iOS (£1.49), or via a series of free calculators at:
http://www.prostatecancer-riskcalculator.com
As the study, upon which the app and calculators are based, began in 1993, the app and calculators provide a risk of sextant biopsy detectable prostate cancer [2].
The website version of the risk calculators are meant for use as a decision aid for lay people, general practitioners and urologists [3]. On the website there are six calculators which provide a risk of prostate cancer based upon age, family history, and urinary complaints (calculator 1) or PSA alone (calculator 2). Calculators 3-6 are designed for use by urologists and require information typically gathered in an outpatient setting such as digital rectal examination (DRE) findings and volume, transrectal ultrasound findings (TRUS) and volume and previous biopsy status.
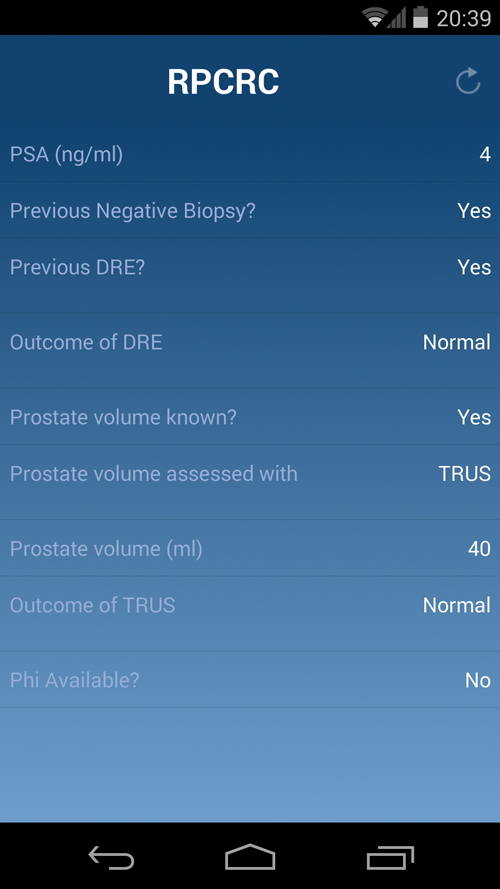
The mobile application was developed in order to improve the user friendliness and accessibility of the risk calculators. It manages to combine many of the website-based calculators into one easy to use application [4]. The parameters used to improve prostate cancer risk assessment include PSA level, previous biopsy status, DRE findings, TRUS volume and TRUS findings and Phi (if available). If the patient has not had a TRUS, then volume can be estimated according to DRE findings instead.
Does this apply to my patients?
The data for the RPCRC was gathered from the Dutch section of the ERSPC, and are based on a population aged 55-74 years. The analyses are based on the biopsy outcomes of 3616 men screened for the first time, 24.5% of whom had prostate cancer detected. A further cohort of 2896 men was used to compile data on those men who had previously been screened, 34.1% of these men already had negative biopsies at first screening. Although the risk calculator has yet to be validated in a UK population it has been validated in a small contemporary clinical cohort despite significant differences between the screening group and the clinical cohort [5].
Is it better than PSA and DRE?
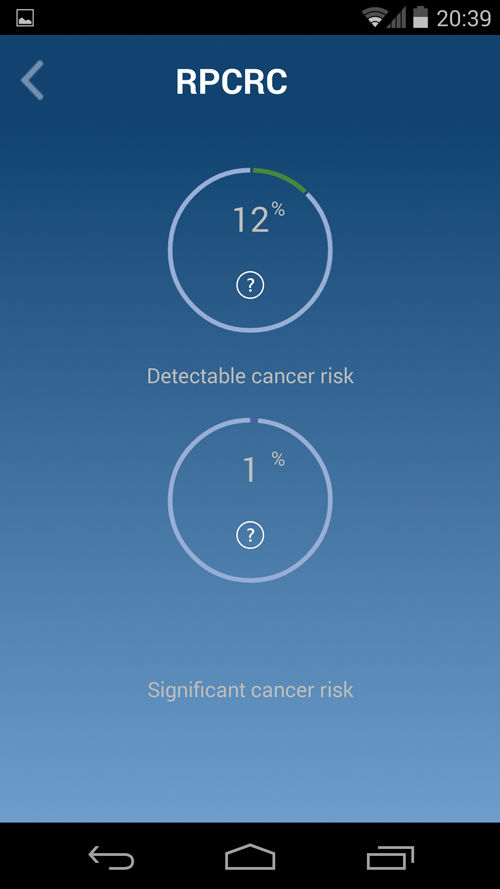
Recently published data at the 29th Annual EAU Congress in Stockholm [4] shows that the more information that is entered pre-biopsy the more accurate the application is in predicting prostate cancer on biopsy. At initial screening, the RPCRC area under curve is significantly better than the combined findings of PSA and DRE (0.79 vs. 0.73, respectively) for predicting prostate cancer. This effect is repeated for detecting serious prostate cancer and in those who have had a previous PSA test and / or biopsy. What information does the calculator provide? The calculator provides the detectable prostate cancer risk as a percentage. The risk is given as a score for detectable prostate cancer and for significant prostate cancer. Significant prostate cancer is defined as tumour stage greater than T2b, and / or having a Gleason biopsy score of equal to or greater than 7. The percentage risk of prostate cancer leads to the following recommended actions:
- <12.5% – no prostate biopsy
- 12.5-20% – consider prostate biopsy depending on co-morbidity and more than average risk of high grade prostate cancer (>4%)
- 20% or more – prostate biopsy recommended
Should you ever forget this information, it is easily accessed within the app, by touching the encircled question mark, under the percentage risks.
Conclusion
Although there is a paucity of studies to externally validate the RPCRC app it provides robust data from a large cohort of men which are likely to be genetically similar to the UK population. The app is well thought out, easy to use in any outpatient clinic and provides a clear recommendation for further investigation. I would recommend the RPCRC app as an essential tool for all urologists and any practitioners involved in PSA assessment.
References
1. Schröder F, Kattan MW. The comparability of models for predicting the risk of a positive prostate biopsy with prostate-specific antigen alone: a systematic review. Eur Urol 2008;54(2):274-90.
2. Clarke NW. Coming up for air: follow-up and risk stratification after negative prostate cancer screening. Eur Urol 2013;63(4):634-5.
3. Roobol MJ, van Vugt HA, Loeb S, et al. Prediction of prostate cancer risk: the role of prostate volume and digital rectal examination in the ERSPC risk calculators. Eur Urol 2012;61(3):577-83.
4. Roobol M, Salman J, Azevedo N. The Rotterdam prostate cancer risk calculator: improved prediction with more relevant pre-biopsy information, now in the palm of your hand. 2014.
http://www.uroweb.org/
index.php?id=108&AID=49681
Last accessed May 2014.
5. Van Vugt HA, Kranse R, Steyerberg EW, et al. Prospective validation of a risk calculator which calculates the probability of a positive prostate biopsy in a contemporary clinical cohort. Eur J Cancer 2012;48(12):1809-15.