Patients presenting for urological surgery range from the young and fit to the elderly with multiple, and often significant, coexistent diseases. This latter cohort can present a significant challenge in the perioperative period, sometimes irrespective of the type of surgery.
Amongst our population lies a hidden subgroup of high-risk patients – the disparity in outcome for them stark. These patients account for 80% of in-hospital deaths after a surgical procedure and represent approximately 10% of our inpatient surgical workload [1].
The first crucial step is to accurately identify those ‘at risk’. This is something that previous reports have highlighted as a shortfall [1,2].
Traditionally anaesthetists have used simple risk indices such as the American Society of Anaesthesiologists (ASA) score (grades I-V based on the anaesthetist’s subjective assessment of the severity of comorbidities). This may be complemented by the evaluation of preoperative functional capacity, widely viewed as a key element of perioperative risk assessment. Historically this is done by the determination of a patient’s Metabolic Equivalent of Task (MET), with 4 METs equating to the ability to walk up one flight of stairs (1 MET = amount of oxygen consumed at rest = 3.5ml kg-1 min-1). More objective measurement of functional capacity, and now commonplace in most UK hospitals, is achieved by cardiopulmonary exercise testing (CPET). CPET helps to quantify an individual’s functional ability to respond to increased metabolic demand of surgery by evaluating cardiovascular, respiratory and circulatory systems. However, CPET takes time and interpretation of the complex measures derived requires specific expertise.
Ideally risk assessment begins at the earliest opportunity, in the outpatient clinic, when surgical intervention is initially considered, and can be carried out by the surgeon, junior doctor or allied health professional. Nowadays the smartphone is most certainly ubiquitous and with the availability of numerous well validated, online risk calculators, determining an individual’s risk is quick and easy to do, and allows us to more accurately inform our patients.
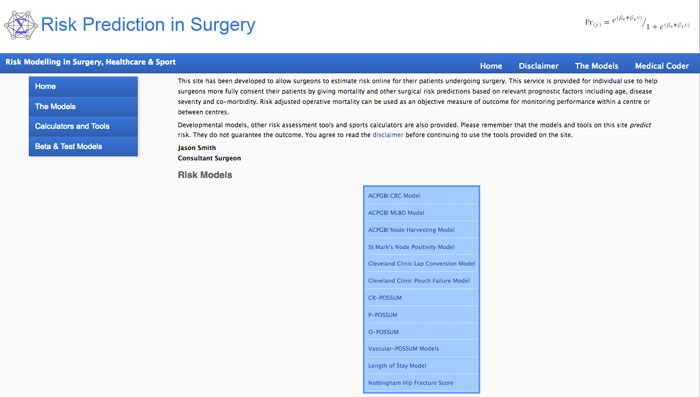
Risk calculators include ‘general’ and ‘specialty-specific’ models. There are no specific urological risk calculators but several more general tools may be applied.
One of the most widely validated scoring systems is the Portsmouth Physiological and Operative Severity Score for the enumeration of Mortality and Morbidity (P-POSSUM). This incorporates 18 (12 physiological and 6 operative) variables to predict morbidity and mortality. One of the key ways it differs from other scoring systems is by using variable weighting – factors with the strongest association to a poor outcome ‘count’ for more. Another key advantage with P-POSSUM is that it takes into account intraoperative events (when applied in the preoperative period these parameters can be estimated). Specialty specific variants include CR (colorectal) – POSSUM, O (oesophagogastric) – POSSUM and Vascular-POSSUM. P-POSSUM can be accessed at http://www.riskprediction.org.uk/index-pp.php
Another useful and more current example is the Surgical Outcome Risk Tool (SORT). This was developed in response to the 2011 NCEPOD study on perioperative care [1]. Data from the 16,788 patients included in the study was used to develop and validate the tool [3]. Unlike P-POSSUM, SORT does allow filtering by specialty (‘Urinary system and male reproductive organs’), by sub-group (Kidney / renal pelvic, Ureter, Bladder, Urethra, Prostate, Genitalia), and even the individual procedure. Ultimately the tool provides an estimate of the risk of death within 30 days of an operation. SORT is available as a free app (App store – Apple; Google Play – Android) or alternatively can be accessed at http://www.sortsurgery.com/
In the US the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) have developed a robust risk calculator from >2.7 million operations from 586 hospitals from 2011-14. The tool uses 20 patient predictors and the planned procedure to estimate the chance of an ‘unfavourable outcome’ (complication or death) after surgery. A similar multidisciplinary initiative is underway in the UK, the Perioperative Quality Improvement Programme (PQIP) [4]. The ACS NSQIP Surgical Risk Calculator can be accessed at
http://riskcalculator.facs.org/RiskCalculator/index.jsp
Although the above examples of risk calculators are all well validated, they provide estimates only. That said, there is no doubt they may be used as useful adjuncts in perioperative risk assessment that can be used to help us better inform our patients facing a surgical procedure. Give them a try!
References
1. Findlay GP, Goodwin APL, Protopapa KL, et al. Knowing the risk: a Review of the Peri-Operative Care of Surgical Patients. National Confidential Enquiry into Patient Outcome and Death; London, 2011. Accessed 18 May 2017 from
www.ncepod.org.uk/2011report2/
downloads/POC_summary.pdf
2. The Royal College of Surgeons of England / Department of Health. The higher risk general surgical patient: towards improved care for a forgotten group. Accessed 18 May 2017 from
www.rcseng.ac.uk/library-and
-publications/college-publications/
docs/the-higher-risk-general-surgical-patient/
3. Protopapa KL, Simpson JC, Smith NCE, Moonesinghe SR. Development and validation of the Surgical Outcome Risk Tool (SORT). Br J Surg 2014;101:1774-83.
4. Perioperative Quality Improvement Programme (PQIP). NIAA-HSRC. Accessed 7 June 2017 from
https://pqip.org.uk/Content/home





