The second article in this series of challenging cases in endourology describes some stent-related problems.
Case 1
A 76-year-old male with end stage renal failure due to obstructive uropathy from benign prostatic enlargement was transferred from a referring hospital. A right ureteric stent had been placed and a left sided stent was sited too far proximally in the ureter (Figure 1). Comorbidity included ischaemic heart disease, cardiac failure and the patient was anti-coagulated. There had been one failed attempt to re-position the stent.

Figure 1.
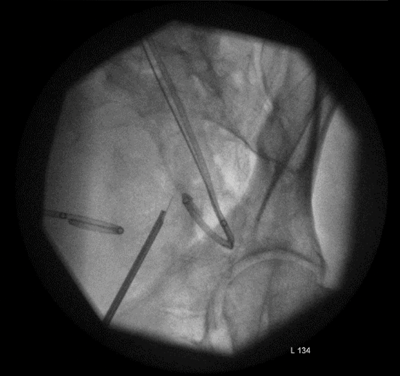
Figure 2.
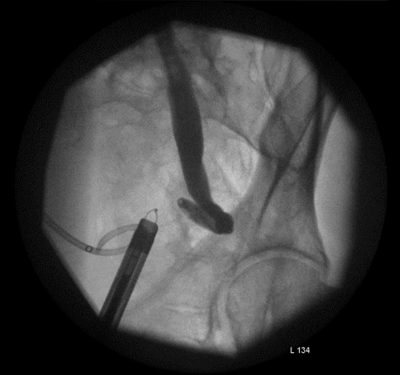
Figure 3.
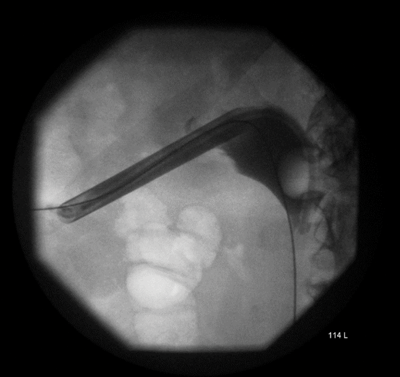
Figure 4.
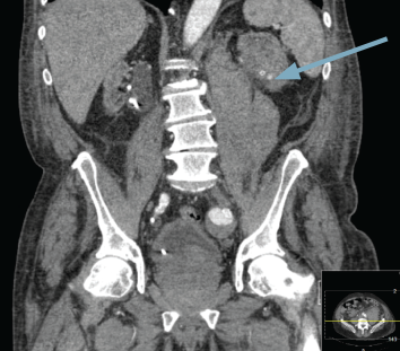
Figure 5.
Blush of contrast in left kidney during arterial phase CT.
A nephrostomy was placed into the obstructed left kidney and a radiological attempt to ‘lasso’ the stent failed. The patient was taken to the operating theatre for a combined antegrade and retrograde approach to ureter. No ureteric lumen was visible beyond 1cm at ureteroscopy and multiple attempts at antegrade and retrograde wire placement failed.
The lower ureter was tortuous and of the ‘fish-hook’ type. A nephrostogram revealed a stricture at the vesicoureteric junction (VUJ) and incision of the VUJ using a Collins knife failed to demonstrate the lumen (Figure 2 and 3).
A percutaneous puncture removed the stent, the radiological nephrostomy tube was removed and a 16F urethral catheter was inserted as a permanent nephrostomy in a patient who was now dialysis dependent (Figure 4). The patient bled post-procedure requiring embolisation (Figure 5).
Learning point
-
The final stage of the placement of a ureteric stent is observation of the stent in the bladder
Case 2
A 53-year-old male presented with multiple calculi in his right renal pelvis (Figure 1) having had an open pyelolithotomy 10 years prior. He had a supra-pubic catheter in place for an atonic bladder. A right percutaneous nephrolithotomy (PCNL) cleared the stones and an antegrade ureteric stent was placed (Figure 2).

Figure 1.
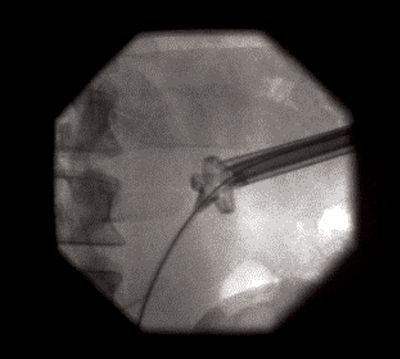
Figure 2.
The patient was lost to follow-up and presented with the stones demonstrated in Figure 3, which is a poorly centred radiograph.
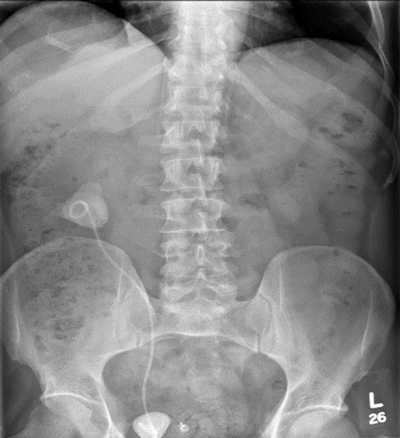
Figure 3.
A DMSA scan demonstrated 34% function in the kidney and following discussion at an X-ray meeting, a right open pyelolithotomy, pyeloplasty and cystolitholopaxy were performed.
The kidney was grossly inflamed and it was very difficult to identify the anatomy. The surgeon considered a nephrectomy but persevered to complete the repair. The patient remained in hospital for two weeks postoperatively with low grade pyrexia and a CT revealed a clot in the collecting system and possible calyceal perforation (Figure 4) and extravasation. This was seen to have improved on a subsequent CT (Figure 5).
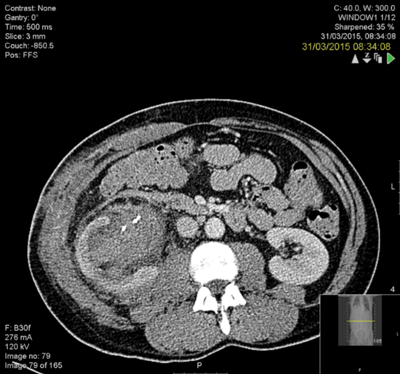
Figure 4.
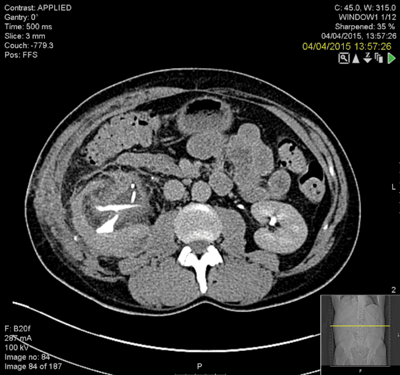
Figure 5.
The stent was removed at three months and a retrograde examination in theatre and live fluoroscopy revealed good drainage.
Learning points
-
Forgotten stents can be a source of significant morbidity
-
Every attempt should be made to preserve nephrons
-
Open surgery still has an occasional role in stone disease
-
When postoperative bleeding is anticipated, use the widest possible ureteric stent
-
Clot in the renal pelvis will dissolve with time
Declaration of competing interests: None declared.







