Case 1

Image A.
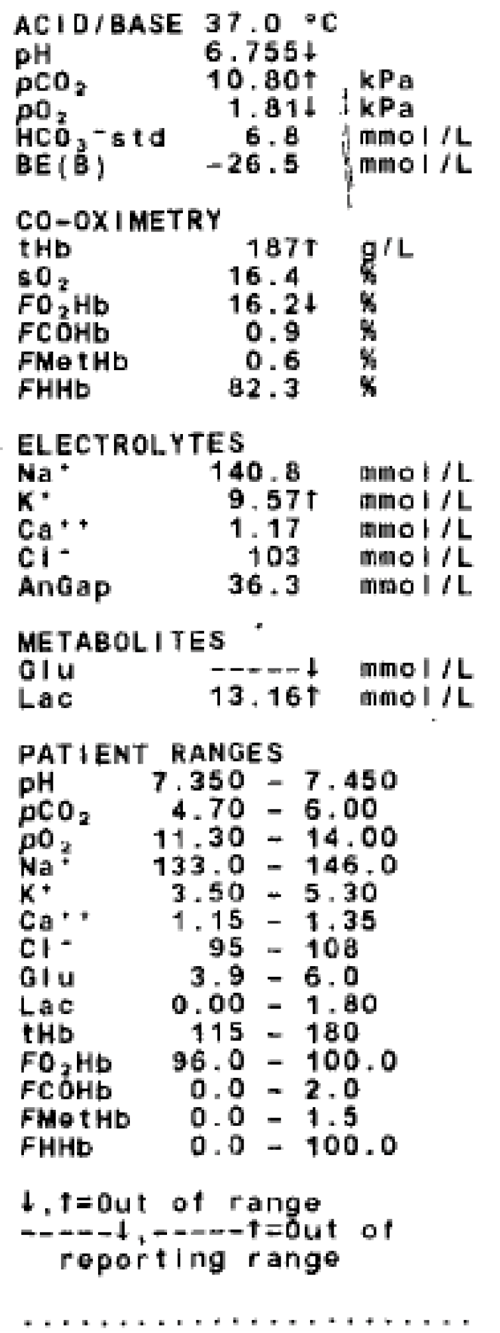
Image B.
- Who is the mythological figure depicted in image A and how does he relate to a urological emergency?
- Define priapism and list five causes.
- In the context of a patient presenting with priapism, what test has been performed (Image B) and what do the results imply?
- In combination with aspiration / drainage of the corpora, what class of pharmacological agent can be injected? Describe how it is prepared and given?
- What is the overall resolution rate of aspiration and irrigation, combined with intra-corporeal pharmacological agents?
- When might the surgical insertion of a penile prosthesis be considered?
Case 2
Parameter: Semen volume (mL)
Value: 2.8ml
Parameter: Total sperm number (106/ejaculate)
Value: 0
Parameter: Sperm concentration (106/mL)
Value: 0
Parameter: Total motility
Value: 0
Parameter: Progressive motility (%)
Value: 0
Parameter: Vitality (live spermatozoa, %)
Value: 0
Parameter: Sperm morphology (normal forms, %)
Value: 0
- What does this semen analysis suggest the patient may have?
- Can you define obstructive azoospermia?
- At which level of the spermatic journey is the obstruction most frequently at, and what is the most common congenital cause of obstructive azoospermia?
- What surgical procedure is recommended in patients with iatrogenically acquired post-surgical epididymal obstruction? What are the patency rates associated with this procedure?
- How can sperm be retrieved in patients with congenital bilateral absence of the vas deferens?
Case 3

- What does this Doppler ultrasound image show?
- How are varicocoeles graded in clinical practice?
- What is the investigation of choice to diagnose a varicocoele?
- What is the recurrence rate if the varicocoele is treated via radiological embolisation or laparoscopy?
- What is the likely diagnosis in an adolescent presenting with acute shortness of breath and haemoptysis, three days following embolisation of varicocoele? Why is this likely to have happened?
Andrology – answers
Case 1
-
Priapus – minor Greek God of Fertility, who had a marked permanent erection which gave rise to the medical condition of priapism.
-
Priapism is a disorder of penile erection that persists beyond or is unrelated to sexual interest or stimulation, and by consensus lasting for greater than four hours. Causes include: haematological dyscrasias (e.g. sickle cell anaemia, myeloma), neurogenic disorders (e.g. spinal cord injury, cauda equina syndrome), infiltrating urological neoplasms, medications (e.g. sildenafil, intra-cavernous therapies) and recreational drugs.
-
Penile corporal blood gas analysis. The results are in keeping with ischaemic / low-flow type priapism, the most common type.
-
Alpha-adrenergic agonists. Dilute 10mg of phenylephrine up to 10mls with normal saline (1mg/ml). Inject 0.5mls (500mcg) every five minutes, for up to one hour. Side-effects include tachycardia, hypertension and arrhythmia, therefore need blood pressure, pulse and cardiac monitoring.
-
80%.
-
Intractable, therapy-resistant ischaemic priapism lasting more than 48-72 hours usually results in complete erectile dysfunction and risk of penile deformity.
Case 2
-
Azoospermia.
-
Obstructive azoospermia is the absence of spermatozoa and spermatogenic cells in semen due to bilateral obstruction of the ducts.
-
Obstruction at the level of the epididymis is the most common cause. Congenitally this is due to congenital bilateral absence of the vas deferens, associated with at least one mutation of the CF gene (Chromosome 7).
-
Microsurgical intussusception: epididymovasostomy 60-87%. 5. Microsurgical epididymal sperm aspiration (MESA) can retrieve sperm, which can be subsequently used for intra-cytoplasmic sperm injection (ISCI).
Case 3
-
Left sided varicocoele.
-
Subclinical – not palpable / visible but discovered on ultrasound. Grade 1 – palpable only on Valsalva manoeuvre; Grade 2 – palpable at rest, but not visible; Grade 3 – palpable and visible at rest.
-
Colour doppler ultrasound study.
-
10% radiological, 3-7% laparoscopic.
-
Pulmonary embolism, due to migration of the coil into vena cava and subsequently pulmonary artery.