Case 1
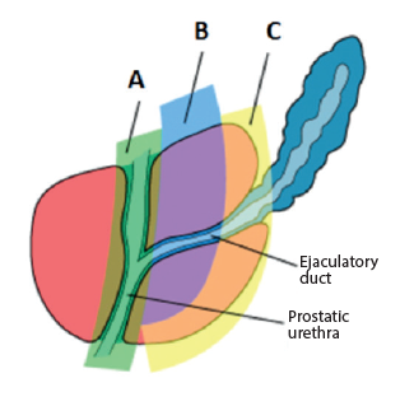
- Define the zonal anatomy of the prostate: A, B and C
- What is the significance of Zone A and Zone C?
- Clasify the types of lower urinary tract symptoms (LUTS)
- Which investigations should be routinely undertaken for a patient presenting with uncomplicated LUTS in the primary care setting?
Case 2

- What is this device called?
- Can you describe the different ways in which such devices work?
- Describe the different types of artefacts that can occur when using this device.
- What are the necessary criteria to make sure the test is valid and reliable?
Case 3
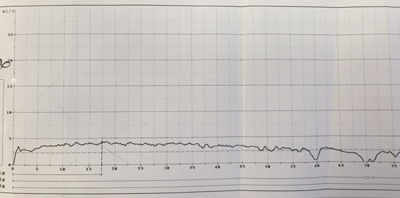
Flow rate of a 27-year-old male complaining of a poor flow.
- What is the likely diagnosis?
- How can this be managed?
- What is the likely success rate of surgical treatment at 12 months?
- What is the best primary treatment option? 5. What is the definitive treatment option for failed primary treatments?
Case 4
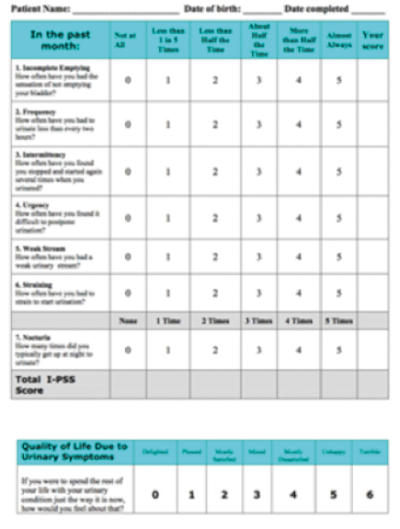
- What is this questionnaire?
- What does the questionnaire assess?
- What are the three different scoring categories and their ranges?
- What does NICE recommend be offered to men with bothersome to severe voiding LUTS and prostate size estimated to be greater than 30g?
Answers
Case 1
-
A – transition zone, B – central zone, C – peripheral zone.
-
Zone A (transition zone) is predominantly associated with benign prostatic hyperplasia. Zone C (peripheral zone) is predominantly associated with the prostatic adenocarcinoma.
-
Voiding LUTS, storage LUTS and post-micturition dribble.
-
The following should be undertaken routinely for investigating uncomplicated LUTS (NICE guidelines): urine dipstick, frequency / volume chart, assessment of their baseline symptoms with a validated symptom score (e.g. IPSS) and prostate specific antigen PSA testing after appropriate counseling.
Case 2
-
Flow-rate machine or uroflowmeter.
-
Rotating disc – spins at constant speed, higher flow rates means higher current to maintain constant speed; Gravimetric (weight transducer); Electric automatic microprocessor dipstick (capacitance).
-
Squeeze artefact – caused by the patient compressing their own penis during micturition; Cruising artefact – if patient allows the urinary flow to wander around the receiving funnel; Straining artefact – forced voiding using abdominal wall muscles.
-
Pass an adequate voided volume of >150ml. The study must be postponed if active urinary tract infection UTI. Pharmacotherapy must be stopped >48 hours prior to testing.
Case 3
-
Urethral stricture: this flow trace demonstrates a characteristic plateau shape.
-
Surgical management: optical urethrotomy or urethral dilatation, +/- intermittent urethral dilation / catheterisation or definitive urethroplasty.
-
Stricture <2cm: 60% success rate; 2-4cm stricture: 50% success rate; >4cm stricture: 20% success rate.
-
There is no significant difference in outcome between dilation and urethrotomy as initial treatment for strictures (Steenkamp JW, Heyns CF, de Kock MY. Internal urethrotomy versus dilation as treatment for male urethral strictures: a prospective, randomized comparison. J Urol 1997;157(1):98-101).
-
Urethroplasty (anastomotic or substitution).
Case 4
-
International Prostate Symptom Score (IPSS).
-
Seven questions: four on voiding symptoms and three for storage symptoms, plus an overall quality of life question.
-
<8 is considered mild, 8-19 is moderate and 20-35 is severe.
-
Combination of an alpha-blocker and a 5-alpha reductase inhibitor.





