Case 1
A 43-year-old lady presents with urinary incontinence and vaginal pain associated with intercourse. An initial CT scan is performed. Case courtesy of Radswiki, Radiopaedia.org, rID: 12056.

Case courtesy of Radswiki, Radiopaedia.org, rID: 12056
- What is the clinical diagnosis from the imaging?
- How common are these in women?
- How do they usually present?
- How are these diagnosed?
- How are they classified?
Case 2
On performing a pelvic examination in a female you see the following.
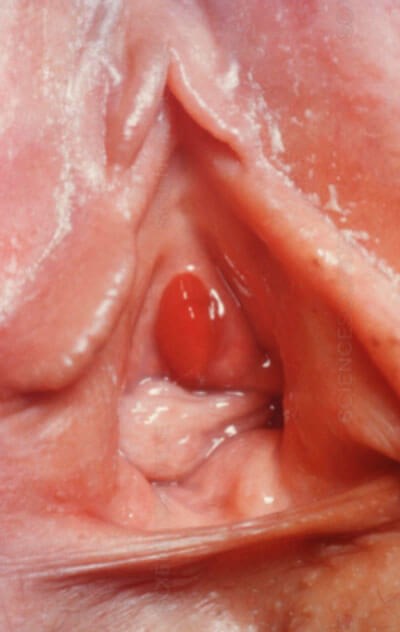
- What is the diagnosis?
- Define this condition.
- What is the underlying pathophysiology?
- What is the differential diagnosis?
- What are the treatment options?
Case 3
While performing a cystoscopy for haematuria, the following are encountered in the male urethra:
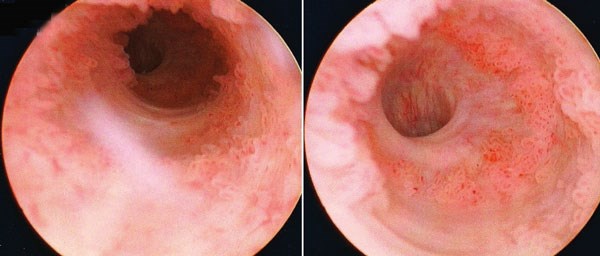
- What is the likely diagnosis?
- What are the risk factors for this?
- How common is this?
- What is the T-stage classification?
- What factors affect overall disease survival?
References
1. Greenwell TJ, Spilotros M. Urethral diverticula in women. Nature Reviews Urology 2015; 12:671-80.
2. Clark J, Olson L, Kujawa M. A review of the diagnosis and management of urethral caruncles. Urology News 2017;22(1):28-29.
3. Gakis G, Witjes JA, Compérat E, et al. EAU Guidelines on Primary Urothral Carcinoma. Eur Urol 2013;64(5):823-30.
Urethral pathology: answers
Case 1
-
Female urethral diverticulum.
-
0.02–6%.
-
A high index of clinical suspicion aids the diagnosis. Classically they present with dysuria, dribble and dyspareunia (3Ds) – 20% of female cases. Urinary incontinence, recurrent urinary tract infections (UTIs), frequency, urgency, urethral / vaginal lump may be other symptoms.
-
MRI is the imaging of choice, but they can be diagnosed on micturating cystourethrogram, video urodynamics, cystourethroscopy, ultrasound, CT imaging and clinically detected.
-
Multiple classifications have been reported [1-3] but an anatomical classification via MRI is often helpful. This incorporates: simple, horseshoe or circumferential diverticula.
Case 2
-
Urethral caruncle.
-
A small single quadrant urethral prolapse, typically affecting the posterior urethral meatus.
-
Reduced oestrogen levels, causing the urethral smooth muscle to lack support for the urethral mucosa. Another theory is secondary to an inflammatory process following recurrent or chronic inflammation
-
Urethral prolapse / polyp, para-urethral cyst, urethral diverticulum, condyloma, urethral carcinoma.
-
Conservative therapy: sitz-bath, topical oestrogens, anti-inflammatories or steroids. Surgery: excision if conservative methods failed, symptomatic or diagnostic uncertainty
Case 3
-
Urothelial carcinoma (UC) of the urethra.
-
Bladder UC, chronic inflammation after clean intermittent self catheterisation (CISC) / urethroplasty, radiotherapy, radioactive seeds, chronic urethral inflammation post sexually transmitted infection (i.e. HPV 16 related). In female specifically urethral diverticulum and recurrent UTIs.
-
Estimated to be 1.6 per million (males) and 0.6 per million females.
-
Tx Primary tumour cannot be assessed. Tis Carcinoma in situ. T0 No evidence of primary tumour. Ta Non-invasive papillary carcinoma. T1 Tumour invades subepithelial connective tissue. T2 Tumour invades any of the following structures: corpus spongiosum, prostate, peri-urethral muscle. T3 Tumour invades any of the following structures: corpus cavernosum, invasion beyond prostatic capsule, anterior vaginal wall, bladder neck. T4 Tumour invades other adjacent organs.
-
Age, tumour stage and grade, nodal stage, presence of distant metastasis, histological type, tumour size, tumour location, and type and modality of treatment.




