Case 1

1. What machine is seen in the picture?
2. What is the standard dose schedule for radiotherapy for prostate cancer?
3. What are the complications of radiotherapy?
Case 2
1. How does haemorrhagic cystitis develop?
2. What are the common causes of haemorrhagic cystitis?
3. How can haemorrhagic cystitis be graded?
4. What treatment options for haemorrhagic cystitis are supported by evidence-based medicine?
Case 3

1. What is shown in the picture?
2. How does the treatment delivered from the machine help in radiation cystitis?
3. What are the absolute and relative contra-indications to this treatment?
Case 4
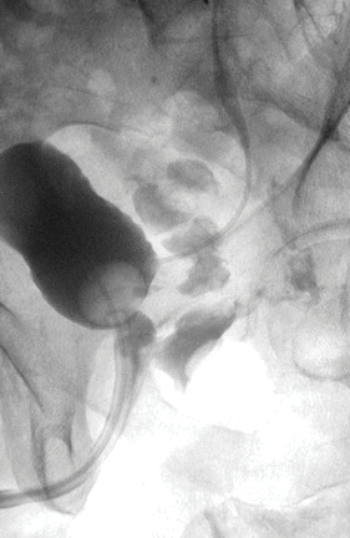
1. What is this investigation and what is demonstrated?
2. How may this patient present?
3. What are the possible causes of this?
4. How can it be managed?
Urologic complications of radiotherapy – answers
Case 1
-
Conventional modern radiotherapy machine.
-
74Gy, given in 37 fractions.
-
Radiation proctitis / enteritis, loose bowels, lower urinary tract symptoms (LUTS), urethral / ureteric strictures, incontinence, erectile dysfunction, radiotherapy induced cancers, haemorrhagic cystitis, fistula, radiation dermatitis.
Case 2
-
Defect in the glycosaminoglycan (GAG) layer, leading to a loss in the barrier protection becoming permeable and allowing inflammatory and hypersensitisation to develop.
-
Radiotherapy, chemotherapeutic agents (e.g. Cyclophosphamide, ifosfamide), intravesical chemotherapy (Mitomycin C), Bacillus Calmette–Guérin (BCG), ketamine.
-
I: non-visible haematuria II: Macroscopic haematuria III: Macroscopic haematuria with small clots IV: Gross haematuria with clots causing urinary tract obstruction requiring instrumentation for clot evacuation.
-
Intravesical hyaluronic acid (preventative and active treatment) and hyperbaric oxygen therapy.
Case 3
-
A hyperbaric oxygen chamber.
-
Hyperbaric oxygen therapy increases the amount of oxygen delivered to radiation-damaged areas of the bladder, which is thought to promote neo-angiogenesis and tissue healing.
-
Absolute contra-indications: untreated pneumothorax, current or recent use of certain chemotherapy agents (e.g. cisplatin, doxorubicin). Relative contra-indications include: airway disease, eustachian tube dysfunction, seizures, fever, pregnancy, congenital spherocytosis, pacemakers, claustrophobia.
Case 4
-
A cystogram demonstrating a recto-urethral fistula. Ureteric stent is visible.
-
Pneumaturia, faecaluria, anal urinary discharge, urinary tract infections, voiding difficulties.
-
Surgical injury, radiation damage (including brachytherapy), focal prostate treatments, unrecognised injury at prostatectomy, inflammatory bowel disease, trauma, malignancy.
-
Faecal diversion and urinary catheterisation. Surgical approaches include transperineal repair with muscle interposition or layered closure of the fistula.
Further reading
Payne H, Adamson A, Bahl A, et al. Chemical- and radiation-induced haemorrhagic cystitis: current treatments and challenges. BJUI 2013;112:885-9.





