Background: the concept of trainee-led research
Over the past five years a novel and exciting collaborative approach to delivering research has been developed in the UK. Trainee-led regional and national research networks have been introduced, with the greatest success seen in specialities such as general surgery and neurosurgery. Trainee-led research is research where trainees are the primary drivers of the design, implementation and delivery of a study.
As a smaller speciality than general surgery, it was proposed that a national urology network, akin to our neurosurgical colleagues, might provide the critical mass required to allow the success of a trainee-led research collaborative in urology. Hence the British Urology Researchers in Surgical Training (BURST) research collaborative was founded.
Why is there a need for a trainee-led research collaborative?
The acquisition of research skills is essential for the professional development of trainees and is a requirement of Completion of Certificate of Training in Urology. Obtaining this experience as a trainee working in isolation can be challenging. Often trainees do not know where to start, find it difficult to come up with an idea and have limited supervision. Thus, they approach the research process in a haphazard manner, which may not necessarily lead to high quality work and may deter trainees from wanting to get involved [1]. However, trainees are highly motivated and resourceful individuals and if engaged correctly and offered appropriate guidance, can form an extremely powerful network.
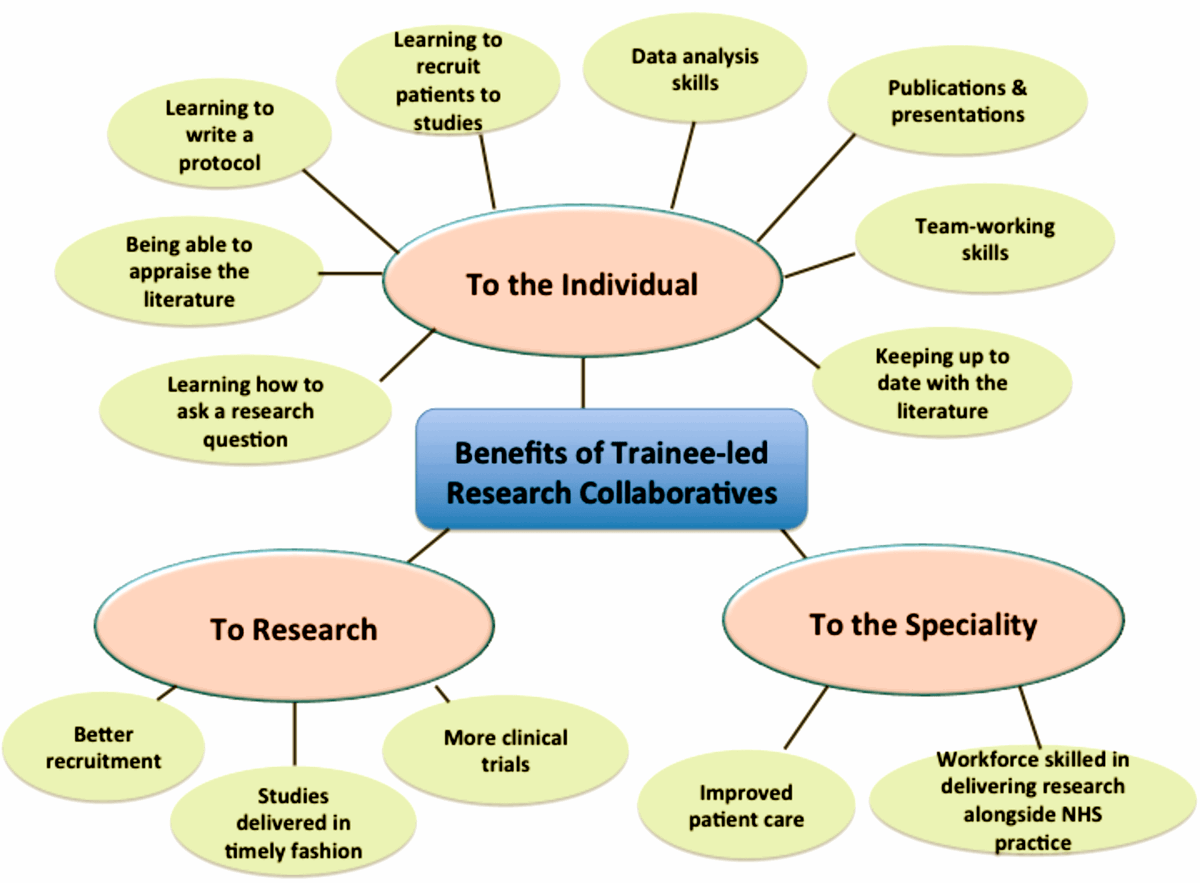
Figure 1: Benefits of trainee-led research collaboratives.
Trainee-led research has a number of benefits for the individual trainee, to the quality of research and to the speciality as a whole (Figure 1). For the individual trainee, being part of a network allows diffusion of expertise between members of the collaborative. Supervision is offered by trainees with specific research experience to those trainees who require development in certain areas, which helps to overcome common difficulties and barriers. The workload can be shared between members of a network reducing the burden on a single individual and increasing the chances of successful completion.
In a supportive network, trainees will better learn how to appraise the literature, identify areas where further research is likely to be of benefit, learn how to ask a research question, learn how to design a research study and write a protocol. They will experience recruitment of patients to studies under the NHS regulatory framework and overcome other barriers in running a clinical study. Trainees will apply their team-working skills to a research project, particularly around prioritisation, delegation and collaborative leadership towards a common goal. They will also get the opportunity to present their work at national and international conferences and publish this work in peer-reviewed journals.
From a research point of view, highly motivated trainees are distributed in different hospitals in a region and across the UK, giving access to large target populations for specific studies. Thus, trainee-led networks can lead to timely recruitment to sample size target, enabling rapid dissemination of the results and ready application to the relevant patient population. Learning from the experience of those within the network potentially allows for more carefully considered research with more robust methodology and much greater impact. As a specialty, the trainee-led network will lead to a consultant workforce that is skilled at delivering research alongside clinical NHS practice, which should ultimately lead to better patient care.
What have other research collaboratives achieved?
In general surgery, the National Appendicectomy Audit prospectively recruited 3326 consecutive patients undergoing appendicectomy from 95 centres during two months [2]. This gave some of the best data presently available on current UK practice in one of the most common surgical emergencies and demonstrates the potential power of a large trainee-led network on recruiting a large number of patients across a large number of centres in a short period of time.
The West Midlands research collaborative completed ROSSINI (Reduction of Surgical Site Infection using a Novel Intervention), a randomised controlled trial in 760 patients from 21 centres assessing the impact of wound edge protection devices in reducing surgical site infection [3]. For this work they were awarded nationally competitive research funding of £232,200 from the NIHR research for patient benefit funding stream. This study recruited ahead of schedule and demonstrated that if trainees are empowered in the design and delivery of prospective clinical trials, then these trials can be completed successfully on schedule.
The ROCSS (Reinforcement of Closure of Stoma Site) study is a randomised controlled trial assessing the impact of a biological mesh at the sight of stoma closure on clinical hernia rate at two years [4]. It has completed its industry-funded pilot phase in 90 patients at 10 sites and is rolling out to a full phase study in a further 470 patients in 30 sites. This study demonstrates the ability of trainees to collaborate with industry whilst delivering complex interventions as part of a randomised trial.
What is the BURST Research Collaborative?
BURST Research Collaborative is a national trainee-led urology research group. Our goals are to develop a national network delivering high quality audit and research answering important clinical questions. We also aim to equip trainees with research skills required to understand, contribute to and deliver research that can improve clinical practice throughout their careers.
Our membership currently comprises urological registrars, core surgical trainees, foundation year doctors, medical students and urological consultants. We do not limit membership to the UK and welcome international members. Membership is free and anyone can join BURST by emailing admin@BURSTurology.com. The majority of our members are interested in robust research without necessarily being ‘academics’. BURST is ideal for trainees who want to gain research competencies and contribute to multicentre research studies. Members do not need to already have strong research backgrounds although amongst our members are trainees with a formal academic component in their timetable.
What does BURST do when a trainee suggests an idea for project proposal?
Once an outline idea for a proposal is put to us, our committee will work through the idea with the trainee to assess suitability for putting forward as a national collaborative project and to help the trainee develop a protocol. After internal peer review by the BURST committee, proposals that are taken to the next stage are sent to our external peer review panel consisting of leading UK academic clinicians and specialist peer reviewers. The peer review process will allow the lead trainee to consider the strengths and weaknesses of their proposal and suggest ways of improving the proposal to make it more robust. A decision on whether to take the proposal to the next stage will be made on the basis of the peer review recommendations. If it passes to the next stage, we will launch the proposal in a pilot phase in several centres in a smaller number of patients to test the feasibility of components of the study. Depending on the pilot phase outcomes, we will decide whether or not to launch the project nationally thereafter.
Challenges in establishing BURST
Although there are significant benefits of a national research collaborative, there were significant challenges in its establishment. Some of these are summarised in Table 1 along with how the challenges were overcome.
Table 1: The challenges in establishing a national trainee-led urology research collaborative.
Challenge
Developing a constitution for the operating of BURST Research Collaborative.
How challenge was overcome
Understanding the workings of existing successful research collaboratives by:
-
Discussions with West Midlands Research Collaborative and National Neurosurgery Research Collaborative.
-
Attendance at Annual General Meeting of London Surgical Research Collaborative and the annual National Research Collaborative meeting.
Challenge
Ensuring direction, goals and targets of BURST were appropriately set.
How challenge was overcome
Establishing an Advisory Board consisting of leading UK academic clinicians.
Challenge
Developing an infrastructure for delivery of BURST Goals.
How challenge was overcome
National call for BURST Research Collaborative Committee Members. Appointment of Webmaster, Secretary, Treasurer, Education Lead and National Site Coordinator.
Challenge
Creation of a communications portal by which members can contact BURST, see what is going on that they can get involved in.
How challenge was overcome
Creation of website: www.bursturology.com
Creation of twitter account: @BURSTurology
Challenge
Funding for core BURST Research Activities.
How challenge was overcome
Application for and awarding of research funding from British Association of Urological Surgeons, BJU International and The Urology Foundation.
Challenge
Giving trainees a forum for presentation of their research ideas and feedback to help develop them.
How challenge was overcome
-
Collaboration with BAUS and Academic Section.
-
Dragon’s Den presentation of shortlisted ideas at BAUS Annual Meeting 2015 and BAUS Academic Section meeting 2014 and 2015.
-
Research Proposal proforma made available on the website to allow submissions all year around.
Challenge
Quality assurance in the development of methodologically strong collaborative proposals.
How challenge was overcome
Development of peer review process and panel consisting of internal peer review by committee and external peer review by advisory board and other specialist members (e.g. methodologist, statistician, anaesthetist, biomedical scientist).
What role can a trainee play in BURST?
A trainee can present their own ideas for studies to BURST as a Project Lead Investigator. In this role they would drive the idea forward and take prime responsibility for first draft of the study protocol.
As a Project Committee Member, trainees can contribute to literature searches and assist the Project Lead Investigator in the writing of key trial documents, regulatory approvals and funding applications.
As Local Investigator a trainee can carry out the study at their site and obtain approvals required.
As a Writing Committee Member, trainees would be responsible for writing of the paper and critical revisions. Usually those with key roles in the design, implementation and analysis of the study form the writing committee.
Trainees should look at our website www.bursturology.com for details on how to get involved in specific projects.
How are contributors acknowledged in BURST research?
BURST aims to recognise all trainees who have contributed to a study as PubMed indexed collaborators on publications and presentations related to the study. Specific authorship policy will be specified in advance of each study. Journal requirements may influence how authorship is presented.
What work is BURST currently carrying out?
MIMIC (A multicentre cohort study evaluating the role of inflammatory markers in patients presenting with acute ureteric colic), led by trainee Taimur Shah, was awarded best collaborative proposal at the BAUS Academic Section Annual Meeting in 2014. It is a cohort study that was developed through peer review to produce a protocol and analysis plan. The pilot phase has commenced, with data for over 100 patients in six centres having already been collected. The full phase of the study in over 800 patients and approximately 30 centres will open in due course. Trainees interested in collecting data at their site can still get involved and should contact us via the website.
A systematic review and meta-analysis (PROSPERO registration number CRD42015017543) on the role of MRI-targeted prostate biopsy in the diagnosis of prostate cancer is underway, led by trainee Veeru Kasivisvanathan. Eight BURST members are involved in review, primarily to screen articles for inclusion in the review and subsequently data extraction. A national call for screeners was announced and more than 30 applicants applied for the role.
Alastair Lamb was the winner of the best collaborative proposal at the BAUS Annual Meeting 2015 with his proposal of a cohort study investigating the relationship between preoperative patient anxiety and intraoperative blood loss. The project has been through peer review and the pilot was launched at Addenbrookes. Data for over 1000 patients was collected and following analysis it was concluded that there was no statistically significant relationship between preoperative anxiety and intraoperative blood loss. It was decided not to launch the study nationally.
Costa Healy was the winner of the best collaborative proposal at the BAUS Academic Section Annual Meeting 2015 for his project proposal entitled IDES (Inappropriate Delays for Exploration of the Scrotum). This project has been discussed at the National Research Collaborative Meeting with collaborations formed between the Paediatric Surgery Network, General Surgery Network and BURST. The protocol is in development and due to undergo peer review.
What is the vision for BURST?
BURST welcomes new research proposals from trainees at all times. To contact BURST with an idea the Research Proposal Proforma available on the website can be completed. The features of an ideal project proposal in the early stages of a research collaborative are given in Table 2. The projects that are most likely to work are ones with short-term outcome data collection and where the pathology being investigated is common. Observational designs are easier to implement but if an interventional study is being proposed, the intervention should be simple and clinicians (including consultants) should have equipoise.
Table 2: Features of ideal projects for the early stages of a research collaborative.
Feature
Short-term data collection e.g. primary outcome at one month or less.
Explanation
The shorter the length of the study, the easier it is to engage rotating trainees to complete data collection.
Feature
Common pathology.
Explanation
The more common the problem the easier it will be to recruit large numbers of patients across many centres.
Feature
Observational studies.
Explanation
Hypothesis-generating studies which may often avoid the need for ethical approval and funding, which reduces barriers to running the study although impact is less.
Feature
In interventional studies:
-
Simple intervention
-
Equipoise
Explanation
A simple intervention is easier to administer across many centres as part of clinical practice than one that requires extensive expertise and / or training.
Clinicians (particularly consultants) must not have a strong preference for treating patients in a fixed way and must be willing to randomise patients to any of the interventions under investigation.
BURST plans to establish the network with the national launch of the MIMIC cohort study. Once completed, BURST will present the results at national and international conferences leading to publication in a peer-reviewed journal.
In the meantime, BURST intends to develop a protocol for an interventional study and look to obtain approvals and funding to launch it. More complex study designs and greater flexibility in time points for data collection will be considered. Alongside project development, BURST intends to support the educational needs of trainees to empower them to take part in research. This will be through content on the website, through running research methodology courses and by lobbying urology programme directors to consider including research training such as good clinical practice as part of regional teaching programmes.
References
1. Kasivisvanathan V, Tantrige P, Webster J, Emberton M. Contributing to medical research as a trainee: the problems and opportunities. BMJ Careers 2015.
2. Collaborative NSR. Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. The British journal of surgery 2013;100(9):1240-52.
3. Pinkney TD, Calvert M, Bartlett DC, et al. Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI Trial). BMJ 2013;347:f4305.
4. Bhangu A, Futaba K, Patel A, et al. Reinforcement of closure of stoma site using a biological mesh. Tech Coloproctol 2014;18(3):305-8.
TAKE HOME MESSAGE
-
BURST is the national trainee-led urology research collaborative and has several on-going projects that trainees can get involved in. They are advertised on the website at www.bursturology.com
-
BURST welcomes the submission of new project proposals all year round and offers twice yearly submission opportunities for presentation at the BAUS Annual Meeting and BAUS Academic Section Meeting.
Declaration of competing interests: V Kasivisvanathan is funded by a Doctoral Research Fellowship from the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Funding: No funding was required to produce this work but BURST would like to acknowledge funding from the British Association of Urological Surgeons, the BJU International and The Urology Foundation.
Feedback from trainees involved in BURST
"I submitted an idea for a collaborative project which I presented at the BAUS 2015 Dragon's Den. The idea was to investigate whether there was link between patient anxiety levels and blood loss in surgery. The BURST team put the proposal through a couple of rounds of review, including both peers (fellow SpRs), senior urologist academics and invited specialists (an academic anaesthetist) which allowed me to refine the question and protocol of investigation. We conducted a pilot study of 750 men in Cambridge and found no concrete evidence for a link between stress and blood loss and so decided not to proceed with the study.
I thought the process was conducted in a professional and business-like fashion with appropriate attention to detail from the BURST team. Nonetheless, there was never a sense of the project being 'taken out of my hands'.
I wholeheartedly recommend that other trainees submit ideas for consideration to the BURST Research Collaborative and I have no doubt there will soon be a small number of highly successful nationwide projects answering simple yet clinically relevant research questions."
Alastair Lamb, Urology SpR, University of Cambridge
"I submitted an abstract for my project called MIMIC to the ‘Urology’s got talent’ section of the BAUS academic meeting in December 2014. Since that day I have been developing it with the help of BURST, who have assisted me in developing the project from conception to commencement. Initial use of the project proposal proforma guided me in writing my idea in a clear and concise manner which would be legible to a scientific audience. Subsequent critiquing during the BAUS academic presentation by a panel of academic experts allowed me to develop and focus the project outcomes. We have now completed the initial pilot with the full national roll-out due to happen shortly.
We all have ideas for audits and research projects but they rarely become big enough or focused enough to change practice. Through the process set up by BURST, I have learnt how to take an initial idea and make it into a full project. This process has taught me the importance of a clear research plan, research questions and outcome measures. In addition, I have made links with various units, consultants and trainees from around the country. I managed to secure a place on the committee and I now help to develop other proposals. This has been an invaluable learning experience for me in my future career."
Taimur Shah, Urology SpR, University College London











