Genital gender affirmation surgery (GAS) is the final step in the transition journey for transgender men. Genital GAS involves a combination of procedures to surgically align physical characteristics with one’s gender identity. These needs change between each individual depending on their gender identity (see below), desire for childbearing, personal preferences and tolerance for potential complications relating to these operations.
What is gender identity and gender dysphoria?
Terminology in the field of gender identity is constantly evolving but an understanding of the nomenclature is helpful when interacting with transgender patients. Sex assigned at birth refers to the sex assigned to a newborn baby by a clinician based on external genitalia and / or through prenatal diagnostics like ultrasound. Gender identity refers to a person’s psychological sense of their gender as female, male or non-binary. Increasingly, the concept of gender identity is changing from binary concepts (female or male) to a more fluid spectrum. Gender dysphoria results when the sex assigned at birth is incongruent with the gender identity of the person resulting in psychological distress. Sexual orientation is distinct to gender identity and is defined by the types of person towards whom one is sexually and / or emotionally attracted to.
Referral pathway for gender affirmation surgery
The medical care (including monitoring of testosterone supplementation) and psychological support for transgender men are both provided by gender dysphoria clinics. Patients require a ‘two signature referral’ by two gender physicians in order to access services for genital GAS. Genital GAS for the UK has been centralised at St Peter’s Andrology in London. The patient would need to be aged 18 or over, have lived in the gender role that is congruent with their gender identity for greater than a year and used gender affirming hormone therapy for greater than a year prior to referral. These criteria are mandated by the World Professional Association for Transgender Health (WPATH) Standards of Care version 7 published in 2011 [1]. Version 8 is due for release in 2021.
Goals of surgery
Genital GAS further ameliorates gender dysphoria in the properly selected patient. Body satisfaction scores were higher following gender affirming hormone therapy with surgery compared to hormone therapy alone [2]. Transgender men receiving hormone therapy while awaiting genital GAS had lower satisfaction scores compared to men receiving hormone therapy who did not wish to have genital GAS. Importantly, not all transmen desire or request any or all of the procedures encompassing genital GAS. Broadly speaking, these involve the removal of the female reproductive organs (vaginectomy, hysterectomy and / or salpingo-oophorectomy) and reconstruction of the male sexual organs including penile reconstruction, urethral lengthening (joining the phallus urethra to the native urethra), glansplasty (fashioning a glans for the neophallus), clitoral transposition (repositioning or burying the clitoris) and scrotoplasty (reconstruction of a scrotum) followed by insertion of an erectile device and testicular prosthesis.
Surgical considerations
The role of the surgeon is to guide the patient to make the right choice for their needs taking into account what is surgically achievable. There is no ‘one size fits all’ approach to GAS given that around a third of transgender men do not seek genital GAS due to the complex surgery required and risk of complications [3].
Our preference is to perform the surgery in several stages. Some centres abroad offer so-called ‘single stage’ phalloplasty by combining penile reconstruction, scrotoplasty, glansplasty and urethral lengthening. The erectile and testis prosthesis are always inserted at a later stage. We prefer to perform urethral lengthening in the second stage of the operation to allow any complications to be more easily managed in a routine fashion without needing urinary diversion or any additional stages.
We reconstruct a neophallus in the first stage of genital GAS. The two options for penile reconstruction available to the transgender man are metoidioplasty or phalloplasty.
Metoidioplasty
Metoidioplasty is where the clitoris is lengthened to form a micropenis following hypertrophy in response to gender affirming hormone therapy (testosterone). We recommend at least two years of testosterone supplementation in order to achieve maximal hypertrophy of the clitoris prior to surgery. The metoidioplasty normally measures between 4cm and 10cm (median 5.7cm) [4]. Metoidioplasty is therefore best suited for transmen who are of smaller stature and build (body mass index <25kg/m²). Most will be able to void while standing (87-100%) but most patients will continue to void in a cubicle (rather than at a urinal) and penetrative intercourse is rarely possible (Figure 1).

Figure 1: Patient following completion of metoidioplasty GAS.
Metoidioplasty in the UK is performed in three stages. The clitoral ligaments and urethral plate are divided to lengthen the clitoris with the laying of a buccal mucosa onlay graft on the extended portion as a first stage urethroplasty. The metoidioplasty is then completed in the second stage by urethral plate / buccal graft tubularisation and urethral lengthening, micropenis formation, scrotoplasty and removal of the female reproductive organs (if desired). Testicular prostheses are inserted in the third stage and mons resection is offered (if needed) to improve the relative size of the metoidioplasty.
Metoidioplasty is preferred by some transmen because recovery is significantly quicker (three weeks off work compared to six to twelve weeks for free flap phalloplasty) while the micropenis retains full erogenous, tactile sensation and natural erections. The procedure also causes less local scarring and avoids a large donor site wound that some transmen find stigmatising.
Phalloplasty
Phalloplasty or penile reconstruction offers transgender men the most complete genital transformation currently available and is the preferred option for transmen who intend to have penetrative intercourse. The ideal neophallus should be aesthetically pleasing and sensate (to both erogenous and tactile stimulus) while allowing standing micturition and penetrative intercourse. The ideal technique should achieve these goals in a single operation with minimal donor site morbidity. Disappointingly, no contemporary technique satisfies all of the above requirements.
The type of flaps offered in the UK are the radial forearm free (RFF) flap, anterolateral thigh (ALT) flap and suprapubic flap [5]. Distant tissue flaps require microsurgical techniques (free flaps) or the transfer of the flap while preserving the original blood supply (pedicled flaps). The phallus urethra is integrated in the flap by using a tube-in-tube design. The integrated urethra is better vascularised (than other urethral reconstruction techniques) and is the current gold standard due to the lower risk of urethral complications.
Strict criteria must be met prior to penile reconstruction in addition to those mandated by WPATH. Smokers are required to stop for six months prior to surgery. The body mass index has to be below 30 and hair removal of the urethral segment has to be completed prior to surgery. Hair removal requires several sessions over the course of a year (laser hair removal) but transmen who are fair-haired or with very dark skin will require more prolonged treatment by electrolysis.
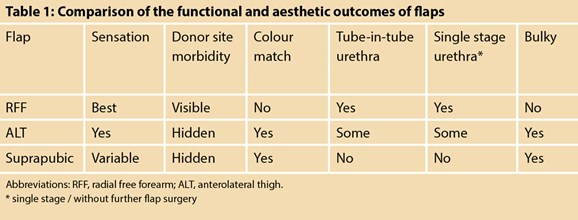
Radial forearm free flap phalloplasty
The RFF flap is the flap most commonly used for phalloplasty. The technique satisfies many of the goals for penile reconstruction and usually results in an aesthetically pleasing neophallus (Table 1). However, transmen with limited subcutaneous fat may find that the neophallus lacks satisfactory girth. The exposed donor site is resurfaced by full thickness skin grafts harvested from the buttocks for the best cosmetic outcome. Nevertheless, the donor site is perceived to be a stigma by some transmen although the scarring can be well-hidden by a sleeve tattoo.
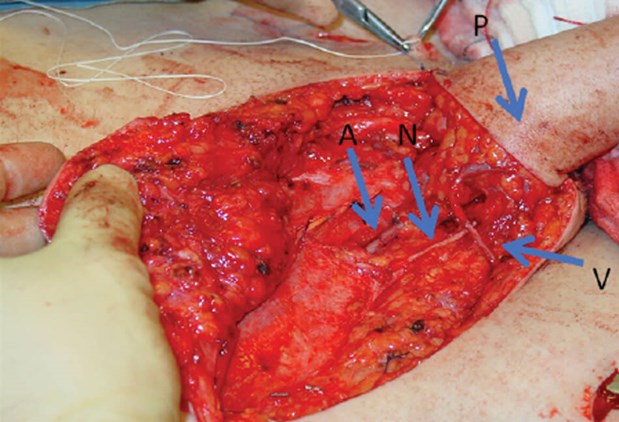
Figure 2: Arterial (A), venous (V) and neural (N) microsurgical anastomoses for the radial forearm free flap phalloplasty (P).
The RFF flap is based on the radial artery while venous outflow is via the cephalic and basilic veins. The radial artery is anastomosed to the inferior epigastric artery via a groin incision while the veins are anastomosed to branches of the ipsilateral saphenous vein using interrupted 8/0 or 9/0 nylon (Figure 2). Tactile and erogenous sensation in almost 90% of patients is achieved by neurorrhaphy between the lateral antebrachial cutaneous nerves of the forearm with the clitoral and ilio-inguinal nerves [6] using 8/0 nylon. Operative time is between seven to ten hours.

Figure 3: Patient following anterolateral thigh flap phalloplasty (second stage).
Anterolateral thigh flap phalloplasty
The ALT flap was first offered in London for penile reconstruction in 2009. The nature of the flap allows for a more easily hidden donor site and greater flexibility in the length of the neophallus (Figure 3). In contrast to the RFF flap, the ALT flap is best suited for transmen with little subcutaneous fat because the distribution of fat is thicker around the thigh. The neophallus and urethra can’t be tubularised if there is too much subcutaneous fat.
The ALT flap is a pedicled flap and does not require microvascular anastomosis thereby reducing the risk of arterial complications. The flap is dependent on perforators originating from the lateral circumflex femoral artery and is at risk of venous congestion and infarction. Sensation to the flap is usually via a single nerve (the lateral femoral cutaneous nerve) and around 60% are sensate.
The vascular anatomy can be variable and the ALT flap may not proceed if not enough perforators are identified at the time of surgery. Also, the pedicle of the lateral circumflex femoral artery may not be long enough, necessitating a free flap. The arterio-venous anastomoses are performed in a similar fashion to the RFF flap. Operative time is between six to eight hours but may be longer if microvascular anastomoses are required.
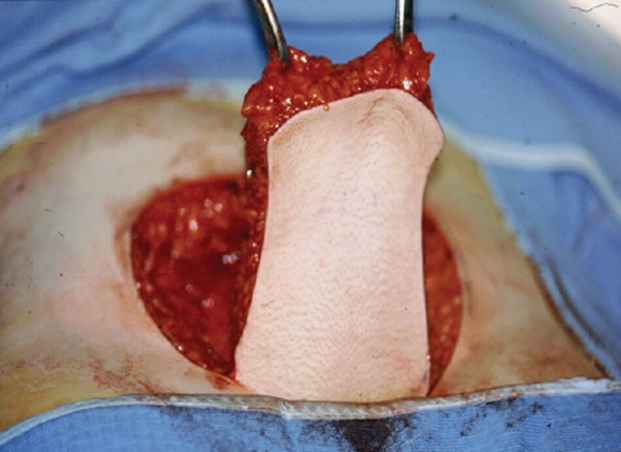
Figure 4: The suprapubic flap is raised from the lower anterior abdominal wall.

Figure 5: Six months following pubic phalloplasty.
Suprapubic (pubic) phalloplasty
The pubic phalloplasty was the first type of flap offered in the UK. It is a pedicled flap raised from the lower anterior abdominal wall and is vascularised by branches of the superficial epigastric artery (Figure 4). Venous drainage is via cutaneous veins and the superficial external pudendal vessels are preserved at the base of the flap if possible. The defect in the anterior abdominal wall can be closed primarily for better cosmesis and is easily hidden by clothing (Figure 5). Sensation is limited to the proximal neophallus because the cutaneous nerves more distally are divided when the flap is incised. Erogenous sensation is absent.
Construction of the flap is quicker than the other flaps (two to three hours) and patients can be discharged after three days (rather than seven days). We recommend pubic phalloplasty for patients with cardiovascular co-morbidities or who are unable to stop smoking because they are unable to have an RFF or ALT flap. Pubic phalloplasty is also an option for patients wishing to avoid a large donor site defect. Radial artery urethroplasty can be offered as a separate procedure if they wish to void while standing meaning that a much smaller flap is raised from the forearm (see below).

Figure 6: Radial artery urethroplasty integrated into a pubic phalloplasty.
Radial artery urethroplasty is a smaller free forearm flap that is tubularised to form a vascularised urethra. It can be integrated into a neophallus constructed without a urethra but requires a separate staged procedure (Figure 6). The flap has a width of 4cm and is raised from the volar aspect of the forearm, which tends to be relatively hairless. The defect is resurfaced with a split skin graft (Figure 7).

Figure 7: Donor site scar following radial artery urethroplasty.
Microvascular anastomoses of the radial artery and cephalic veins to the inferior epigastric artery and saphenous vein respectively is performed in a similar fashion to the RFF flap. More than half the time, a cutaneous nerve can be incorporated in the flap and may improve the sensation of the neophallus.
Adjunctive procedures
We recommend a period of at least six months following penile reconstruction before progressing to the second stage. This period allows the flap to heal and mature before further surgery is undertaken. In the second stage (or third stage, following radial artery urethroplasty) laparoscopic hysterectomy and salpingo-oophorectomy is requested by most transmen. Urethral lengthening is also performed in addition to glansplasty (using the modified Norfolk technique, Figure 8), clitoral transposition (hidden at the base of the neophallus), scrotoplasty and ablation vaginectomy, if desired by the patient.

Figure 8: Appearance of neophallus following glansplasty (forearm flap).
A further period of at least six months is recommended before the final stage of GAS. An inflatable penile prosthesis is inserted in the majority of transmen with the pump acting as a testis in one hemiscrotum with a testicular prosthesis in the contralateral hemiscrotum (Figure 9). Malleable penile prostheses are generally not recommended due to the high risk of erosion. A minority of men decline a penile prosthesis and instead opt for bilateral testicular prostheses. Polyethylene terephthalate (Dacron) graft (Maquet Intergard Silver, Maquet, UK) or hernia mesh (Ultrapro mesh, Ethicon, Livingston, UK) is used to anchor the penile prosthesis cylinders to the pubis and glans due to the lack of corpora cavernosa.

Figure 9: Neophallus (forearm flap) following insertion of inflatable penile prosthesis and left testicular prosthesis.
Outcomes
Patient satisfaction
Transmen are generally satisfied following genital GAS (94-100% satisfaction) [7]. They report a good quality of life and improvement in gender dysphoria following surgery. Outcomes from our unit confirmed that no regret was experienced following genital GAS [8]. All patients that could experience orgasm prior to GAS continued to experience orgasm after clitoral transposition. Almost all (>90%) reported masturbation with their neophallus.
Penile prosthesis insertion and sexual activity
Satisfaction remains high following penile prosthesis insertion. The majority of transmen are satisfied with the aesthetic appearance and are able to engage in penetrative intercourse (>80%). The primary reason for not engaging in penetrative intercourse was the lack of a partner. However, rates of mechanical failure, device infection and erosion are significantly higher when compared to devices in men assigned male at birth. The five-year device survival was 78% in our centre [9].
General advice for urologists
Patient interactions
Trangender patients have historically been stigmatised and marginalised. Understandably, urologists may be uncomfortable interacting with transmen especially when it is not part of their routine practice. An easy way to establish rapport is to use the correct pronouns when addressing transgender patients (just politely ask for their preference). It is also helpful to not have pre-conceived ideas of what is necessarily ‘right’ or ‘normal’ and to respect the spectrum of fluidity in gender identity.
Transgender patients have an extensive peer network and are usually very well informed regarding their care and have a clear understanding of their preferences. They are also understandably fully invested in their healthcare and prefer open and frank communication. It is important to manage their expectations, bearing in mind what may or may not be surgically possible.
Typical presentations to urologists
In general, most urologists would encounter transmen following genital GAS when there has been a complication or to assist with urethral catheterisation. Urethral complications are very common (46% after median follow-up of 3.9 years) and predominantly present as urethral strictures or fistulae [10]. Repair can be challenging due to the lack of well-vascularised native tissue. Consequently, we would recommend urinary diversion by suprapubic catheter during the acute presentation (if indicated) followed by referral to us for definitive urethroplasty.
Transmen following ablation vaginectomy can continue to secrete from residual vaginal mucosa. The secretions collect and transmen can present with pelvic discomfort and a growing bulge in the perineum particularly following sexual excitement. Sometimes, these collections can also be associated with urethral fistulation and urine leak into the cavity. The first response is usually to insert a radiological percutaneous drain but draining the post-vaginectomy cyst complicates repair and we would discourage this unless the patient is septic.
Urgent transfer to London is usually indicated for definitive management of an infected or eroded penile prosthesis. The patient should be resuscitated, and broad-spectrum antibiotics started. Explant of an infected device can be challenging due to the complex anatomy following penile reconstruction.
Lastly, urethral catheterisation is difficult following phalloplasty and urethral lengthening. The skin-based urethra stretches over time leading to a tortuous urethra. A urologist may be called to assist with urethral catheterisation. Our suggestion is to attempt this by flexible cystoscopy with the aid of a guidewire, plenty of water-soluble lubricant and a 14-french catheter. Similarly, retrograde access for urological instrumentation is challenging and we would recommend close discussion with our unit for the optimal strategy.
Summary
Genital GAS is increasingly sought after and represents several procedures that are tailored to the individual needs of each patient. Transmen choose between a full-size penile reconstruction or a micropenis that are complemented by adjunctive procedures like urethral lengthening, scrotoplasty and insertion of an erectile device. Patients are usually satisfied despite a high complication rate.
References
1. Selvaggi G, Dhejne C, Landen M, Elander A. The 2011 WPATH Standards of Care and Penile Reconstruction in Female-to-Male Transsexual Individuals. Adv Urol 2012;2012:581712.
2. Van De Grift TC, Elaut E, Cerwenka SC, et al. Effects of Medical Interventions on Gender Dysphoria and Body Image: A Follow-Up Study. Psychosom Med 2017;79(7):815-23.
3. Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int Jour of Trans 1999;3(3).
4. Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: Techniques and outcomes. Transl Androl Urol 2019;8(3):248-53.
5. Lee WG, Christopher N, Ralph DJ. Penile Reconstruction and the Role of Surgery in Gender Dysphoria. Eur Urol Focus 2019;5(3):337-339.
6. Garaffa G, Christopher NA, Ralph DJ. Total phallic reconstruction in female-to-male transsexuals. Eur Urol 2010;57(4):715-22.
7. van de Grift TC, Elaut E, Cerwenka SC, et al. Surgical Satisfaction, Quality of Life, and Their Association After Gender-Affirming Surgery: A Follow-up Study. J Sex Marital Ther 2018;44(2):138-48.
8. Garcia MM, Christopher NA, De Luca F, et al. Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: the Institute of Urology, London U.K. experience. Transl Androl Urol 2014;3(2):156-62.
9. Falcone M, Garaffa G, Gillo A, et al. Outcomes of inflatable penile prosthesis insertion in 247 patients completing female to male gender reassignment surgery. BJU Int 2018;121(1):139-44.
10. Lee WG, Li V, Ralph D, Christopher N. Novel classification of urethral complications in female to male gender affirming surgery. BJU Int 2020;125(Suppl 1):4.
Declaration of competing interests: None declared.







