As prostate cancer rates increase, many urology departments rely on multi-professional teams to diagnose and manage patients with prostate cancer. The aim of this article is to highlight the skills, training and preparation required for nurse practitioners to undertake trans-rectal ultrasound (TRUS) and biopsy independently.
The term ‘nurse practitioner’ will be used throughout this article although it is recognised that the title may vary from one trust to another. It is hoped that this article will reinforce the need for nurse practitioners learning TRUS biopsy to use an accepted framework for learning and assessment, and to demonstrate to doctors delegating this procedure the learning and assessment steps that have been undertaken.
Introduction
The widespread use of prostate specific antigen (PSA) testing has resulted in an increasing number of patients being referred to urologists with potential prostate cancer. This has led to an increased demand for trans-rectal ultrasound-guided prostatic biopsy. Government targets dictate that patients must be seen, diagnosed and treated within a specific timeframe. In order to meet these targets urology centres throughout the UK are diversifying their approach to both diagnostics and treatment.
There is also widespread recognition and utilisation of the skills of nurse practitioners and associate health professionals who have been instrumental in achieving key milestones to create an efficient healthcare system. These principles include a reduction in waiting times, improving access, enhancing patient satisfaction, improving health outcomes and provision of value for money services [1,2,3]. In 2005, the Cancer Services Collaborative Improvement Partnership produced a document, Applying High Impact Changes to Cancer Care in which the importance of increasing the role of advanced practice nurses (nurse practitioners) in the diagnosis and follow-up care of patients with cancer was highlighted.
A specific area suggested as a high impact change was sonographer-led prostate biopsy [4]. Although sonographers were highlighted in this document we feel that nurse practitioners who are familiar with the diagnosis, treatment and care of men with prostate cancer are better placed to appropriately counsel and consent patients regarding the risks and benefits of undergoing a prostate biopsy.
Current UK practice
Trans-rectal prostate biopsy was one of the first diagnostic procedures in the field of urology to be carried out by urology nurse practitioners. The first nurse to document attainment of a measured level of competency was in 2003 [5]. A training period was completed with a summative assessment by an external consultant urologist who assessed the ability of the nurse practitioner on technical, academic and administrative aspects of service provision. Since then the competence of nurse practitioners carrying out prostate biopsies has been scrutinised, audited and written about many times.
Nurses have consistently been able to demonstrate a significant contribution to improving the patient’s prostate cancer diagnostic experience without an increase in morbidity [1,5,6,7].
The number of nurse practitioners undertaking prostate biopsy is increasing. The benefits of a nurse practitioner service include:
- Improved prostate cancer diagnostics
- Continuity of care for the patients
- A robust teaching programme for trainees
- Effective multi-professional working
A review of the literature has revealed no negative data comparing nurse practitioner to urologist (or urological trainees) carrying out prostate biopsies. Decision making regarding the management of patients diagnosed with prostate cancer and which definitive treatment to offer them should, however, remain the remit of the multidisciplinary team.
Nurse practitioner
The only nursing title protected by law is the term ‘registered nurse (RN)’. Nurse titles are usually decided by the employer but nurses are legally free to use any title suggesting an advanced level of knowledge and skill; as such the titles nurse practitioner, clinical nurse specialist, specialist nurse, advanced nurse practitioner and nurse consultant are often used interchangeably (however, the most senior titles with greatest autonomy are advanced nurse practitioner and nurse consultant). As such, a situation has arisen where, although using a title suggesting an advanced level of education, knowledge, skill and the required tools to work independently, the individual nurse may not be able to demonstrate this. It is for the individual organisation to determine this. However, the Royal College of Nursing and theNursing and Midwifery Council (NMC) oppose the use of the term ‘advanced nurse practitioner’ unless the individual and organisation can demonstrate the nurse has met the required educational preparation [8]. Confusion reigns and it is no wonder that such terms cause confusion to patients and other healthcare professionals.
The nursing regulator, the NMC decided that an advanced practice register was not required in the UK as advanced practice by nurses has not caused harm to patients and therefore further regulation is not required. Many advanced practice nurses feel that this is a failure by the NMC and as such individual professional organisations, such as the British Association of Urological Nurses (BAUN) which represents urological nurses in the UK, are exploring the option of certification and what it would mean for members. BAUN supports the development and maintenance of specialist and advanced practice nursing roles and acknowledges the lack of formal, nationally agreed accreditation for urology nurse practitioners. Although in its infancy, the work undertaken so far seems encouraging and exciting. It is acknowledged that certification would help doctors, who delegate tasks to nurse practitioners, feel comfortable that a standard of education and skill exists that is of a nationally recognised standard.
A recent document issued by the Department of Health on behalf of the Chief Nursing Officer has finally given some guidance as to what is expected (but not legislated) from the advanced practice nurse (Figure 1) [9].
-
Educated to Masters level.
-
Practise autonomously and are self-directed.
-
Assess patients holistically such as physical examination and ordering and interpreting diagnostic investigations.
-
Plan and manage complete episodes of care, delegating or referring as appropriate.
-
Provide evidence-based therapeutic intervention including prescribing medication and monitoring the effectiveness of intervention.
Figure 1: Elements of advanced nursing practice [14].
We feel that it is of great importance that these elements are considered when job descriptions and person specifications are developed for advanced level practice. It is potentially dangerous to give an advanced practice title to a nurse who is unable to fulfil the expectations that the title suggests. It is also important that lead clinicians and their medical teams enforce such expectations to help ensure that their patients receive a high standard of care.
Legal protection
In many UK urology departments, a variety of interventional and diagnostic procedures are now delivered by nurse practitioners, complementing the delivery of a modern urology service. However, while many clinicians agree that an overlap exists between the work of doctors and nurse practitioners, caution is necessary to ensure that any proposed extended role seeks to improve quality of care without exposing the patient to additional, unnecessary risk. The nurse practitioner must be able to demonstrate that a period of supervised practice and formal assessment has been undertaken before performing any advanced practice skills autonomously.
Clinical governance is the system through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care [10]. For nurse practitioners to be confident that their hospitals support their extended practice role, the trust clinical governance committee is currently the only recourse practitioners have to safeguard their professional indemnity. Therefore, it is paramount that the organisation supports the individual nurse practitioner to undertake prostate biopsies and we recommend that this is specifically included in the nurse practitioner’s job description and that it is discussed and documented with his/her nursing manager and the head of department. The consultant urologist must be confident that this process is adhered to and that he/she is happy with the individual practice of the nurse. We must acknowledge that the training of nurse practitioners will come from doctors as nurse practitioners, although expert nurses are often practising in the field of medicine.
Nurse practitioners must also be open to scrutiny and it is important that they audit elements of their practice just as medical colleagues are proficient at doing. The field of prostate biopsies in the diagnosis of prostate cancer is developing with new imaging techniques and it is paramount that the nurse practitioner is given the opportunity to attend courses or conferences in relation to his/her advanced practice. Nurses are legally and professionally accountable for their practice and are bound by ‘The Code: standards of conduct, performance and ethics for nurses and midwives’ [11]. The Code states that “as a professional, you are personally accountable for your actions and omissions in your practice and must always be able to justify your decisions. You must always act lawfully…failure to comply with this code may bring your fitness to practise into question and endanger your registration.”
Training and competency
Trans-rectal ultrasound and prostate biopsy as a technique is challenging to learn and requires competency in both ultrasound imaging and needle placement technique [5,12]. In fact, when surveyed, 68% of urology trainees felt they did not receive enough training to carry out the procedure safely, highlighting the necessity of a structured robust programme in TRUS biopsy training for both urologists and / or the nurse practitioner [12]. BAUN has developed a training programme for nurse practitioners (and other healthcare professionals) to undertake prostate biopsy. It is accepted that unlike urology trainees, nurses and other healthcare professionals are likely to need training and education in areas where the trainee doctor is already proficient such as anatomy, physiology and prescribing.
Additionally, nurse practitioners performing the procedure have raised concerns around a lack of guidelines regarding training and potential litigation should a complication arise. With this in mind a working group was established and developed best practice guidelines on TRUS and biopsy through the European Association of Urology Nurses in 2011 [13]. The guideline was sent to the relevant national societies for comments. The guideline is meant as a handbook for those learning the procedure to assist in the teaching of the required procedural skills but also as a competency document to document the learning and assessment in relation to the procedure.
Prostate biopsy cannot be undertaken in isolation, the assessment of the suitability of the patient to undergo the procedure, informed consent and counselling, regarding the risks and benefits of the procedure, are paramount skills required by the nurse practitioner. As such the nurse practitioner must be highly proficient in counselling patients regarding PSA, undertaking clinical examinations and the complete prostate cancer pathway. It is of paramount importance that the nurse practitioner is able to demonstrate knowledge and understanding in several areas: legislation, clinical expertise, technical knowledge and the ability to communicate effectively to the patient. Additionally, it is paramount that the nurse practitioner is aware of any limitations in knowledge or ability to manage a situation and knows when and how to get help from a doctor. A urologist must be available in case a question or complication arises which the nurse practitioner is unable to manage alone.
Training is required in the following areas:
-
Assessment of suitability and unsuitability of the patient to have a prostate biopsy.
-
Patient consent.
-
Utilisation of ultrasound equipment.
-
Technique.
-
Understanding and managing complications.
Figure 2: Areas of training requirements.
These European guidelines highlighted the need for training in several areas (Figure 2). The guideline also sets out the standards of training that need to be achieved by the nurse practitioner whilst learning to undertake prostate biopsies (Table 1).
Table 1: Standards of training for the nurse practitioner [13].
Nurse practitioners undertaking prostate biopsy should:
-
Be responsible for obtaining informed consent; written consent is considered good practice.
-
Inform the patient of any risk factors specific to them.
-
Be trained by a competent practitioner.
-
Be trained in physical examination including digital rectal examination.
-
Have at least three years of experience working with prostate cancer patients.
-
Carry liability insurance.
-
Be deemed competent after carrying out at least 20 biopsies satisfactorily without supervision at an acceptable speed at level 3 or above (see Table 2).
-
Be supervised directly until deemed competent to undertake the procedure independently.
-
Have final competence assessed and singed off by a senior urologist (or radiologist).
-
Stay abreast of advances in the field and follow continuing education.
-
Be a member of a professional (urological nursing) organisation.
Accompanying the guideline is a competency assessment document that the nurse practitioner uses as a tool to document learning and assessment in the relevant skills related to undertaking a prostate biopsy. The guidelines do not recommend a minimum number of biopsies are carried out before the nurse practitioner is deemed competent but that a minimum number of 20 are undertaken at performance level 3 or above using an accepted criteria (Table 2).
Table 2: Performance levels [13].
Level: 0
Performance Cannot perform this activity in the clinical environment but knows the key principles involved.
Level: 1
Performance: Can perform this activity with constant supervision and some assistance.
Level: 2
Performance: Can perform this activity with some supervision and assistance.
Level: 3
Performance: Can perform this activity satisfactorily without supervision or assistance at an acceptable speed.
Level: 4
Performance: Can perform this activity satisfactorily with more than acceptable speed and quality of work.
Level: 5
Performance: Can perform this activity satisfactorily with more than acceptable speed and quality of work and with initiative and adaptability to special problem situations.
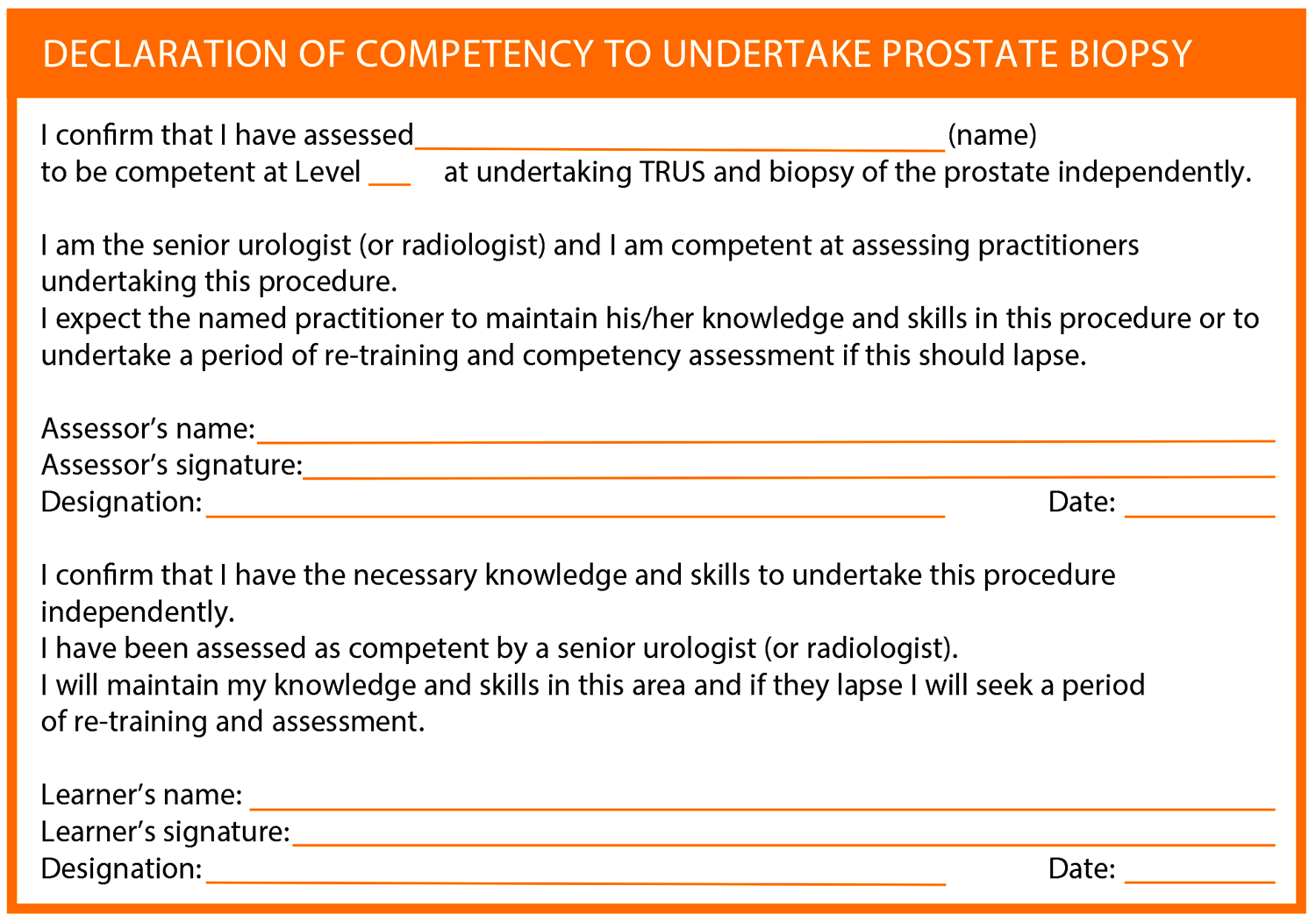
At the completion of training the nurse practitioner should have a declaration of competency signed by a senior urologist (consultant urologist in the United Kingdom) and this should be kept as part of the nurse practitioner’s professional development portfolio – an example from the guideline document can be seen. As discussed above, we also recommend that the nurse practitioner has his/her job description adjusted to specifically recognise that he/she is authorised to undertake prostate biopsies. Depending on local guidelines this may also require a clinical guideline to be developed specific to the organisation.
Conclusion
Nurse practitioners are advanced practice nurses who ought to have undertaken formal training programmes in relation to undertaking diagnostic and patient management skills. Many will also have undertaken a Masters level prescribing course. Nurse practitioners work autonomously under the direction of a clinical lead (consultant urologist). Many undertake advanced practice skills historically undertaken by doctors, such as prostate biopsy. Many nurse practitioners also impart their knowledge by teaching urology trainees. The aim of this article is to highlight the training and assessment undertaken by nurse practitioners who undertake prostate biopsy and to urge urologists and other doctors to insist that their nurse practitioners are adequately trained, use recognised guidelines and are members of a professional nursing organisation to ensure competence in this skill is maintained.
“Nurse practitioners who are familiar with the diagnosis, treatment and care of men with prostate cancer are better placed to appropriately counsel and consent patients regarding the risks and benefits of undergoing a prostate biopsy.”
Most recently the authors have been working with Council members from the British Association of Urological Surgeons to develop a national guideline for training and competency assessment for all specialist urology health professionals undertaking trans-rectal prostate biopsy in the UK. Until certification of advanced nursing practice is adopted in the UK we hope that by standardising the learning and assessment of nurse practitioners undertaking specific advanced skills it will ensure that there is an appropriate environment to learn and impart knowledge. We hope that by demonstrating how we learn, doctors will continue to value the role of the nurse practitioner. Finally, we would urge all urologists to view the guideline.
References
1. Turner B, Pati J. Nurse practitioner led prostate biopsy: an audit to determine effectiveness and safety for patients. International Journal of Urological Nursing 2010;4(2):87-92.
2. Lane L, Minns S. Empowering advanced practitioners to set up nurse led clinics for improved outpatient care. Nursing Times 2010;106(13):14 15.
3. Lipley N. National audit office backs nurse led clinics to ease outpatient waiting. Nursing Standard 2001;15(46):6-7.
4. Cancer Services Collaborative Improvement Partnership. Applying High Impact Changes to Cancer Care 2005.
5. Henderson A, Andrich DE, Pietrasik M, et al. Outcome analysis and patient satisfaction following octant transrectal ultrasound-guided prostate biopsy: a prospective study comparing consultant urologist, specialist registrar and nurse practitioner in urology. Prostate Cancer and Prostatic Diseases 2004;7:122-5.
6. Loftus L, Weston V. The development of clinics in cancer-care. Journal of Clinical Nursing 2001;10(2):215-20.
7. Hori S, Fuge O,Trabucchi K, et al. Can a trained non-physician provider perform transrectal ultrasound-guided prostatic biopsies as effectively as an experienced urologist? BJU Int 2012;111(5):739-44.
8. Royal College of Nursing. RCN Competencies: advanced nurse practitioners. London, UK; RCN; 2012.
9. Department of Health. Advanced level nursing: a position statement. London, UK; Department of Health; 2010.
10. Department of Health. Clinical governance: guidance documents and further information. London, UK; Department of Health; 2008.
http://webarchive.nationalarchives.gov.uk/
+/ www.dh.gov.uk/en/Publichealth/Patientsafety/
Clinicalgovernance/DH_081604
Last accessed February 2014.
11. NMC. The Code: standards of conduct, performance and ethics for nurses and midwives. London, UK; NMC; 2008.
12. Lee G, Attar K, Laniado M, Karim O. Trans-rectal ultrasound guided biopsy of the prostate: Nationwide diversity in practice and training in the United Kingdom. International Urology and Nephrology 2007;39:185-8.
13. Turner B, Aslet P, Drudge-Coates L, et al. Evidence-based Guidelines for Best Practice in Health Care. Transrectal Ultrasound Guided Biopsy of the Prostate. Arnhem, The Netherlands; European Association of Urology Nurses; 2011.
http://www.uroweb.org/fileadmin/
EAUN/guidelines/ EAUN_TRUS_
Guidelines_EN_2011_LR.pdf
Last accessed February 2014.
To review the evidence based guidelines for best practice in healthcare:
trans-rectal ultrasound guided biopsy of the prostate visit:
www.uroweb.org/nurses/nursing-guidelines
Declaration of competing interests: None declared.







