Background
Pelvic floor imaging is an important part of both gastrointestinal and functional urology / urogynaecological departments. Symptoms such as obstructive defecation, incontinence and sphincter complex disorders have a significant impact on patient lifestyle and physical / mental well-being [1,2].
Imaging studies include colonic transit to assess bowel motility. Fluoroscopic and MR proctography is used for assessment of the pelvic floor and its relation to the pelvic organs with physiological effects of micturition and defecation. Endoanal ultrasound and associated physiologic manometry studies also play an important role for the precise evaluation of pelvic floor musculature.
Anatomy
Pelvic floor
The pelvic floor separates the pelvic cavity from the perineum and is formed by muscles and fascia. Two levator ani muscles attach peripherally to the pelvic walls and is joined at the midline by connective tissue. They form a funnel shaped structure called the pelvic diaphragm, which is completed posteriorly by the coccygeus muscles. The coccygeus muscles overlie the sacrospinous ligaments and pass between the margins of the sacrum, the coccyx and the ischial spine. The anal canal passes from the pelvis to the perineum through a posterior circular orifice in the pelvic diaphragm. The pelvic floor is supported anteriorly by the perineal membrane, and muscles in the perineal pouch. The perineal membrane is a thick, triangular fascia that fills the space between the arms of the pubic arch, and has a free posterior border. The deep perineal pouch is a narrow region superior to the perineal membrane. The margins of the U-shaped defect in the pelvic diaphragm merge into the walls of the associated viscera and with muscles in the deep perineal pouch below. The vagina and the urethra penetrate the pelvic floor to pass from the pelvic cavity to the perineum.
Pelvic cavity
The pelvic viscera are located in the midline of the pelvic cavity. The bladder is anterior and the rectum is posterior; in women, the uterus lies between the bladder and rectum. The bladder is referred to be in the anterior compartment with the uterus / vagina in the middle compartment. Posteriorly, the rectum and anus constitute the posterior compartment.
Proctography
Fluoroscopic proctography is still the mainstay for assessing patients with defecating difficulties because it is able to demonstrate the defecation process in real-time, allowing functional assessment. It also has the advantage of being widely available and less expensive than MR proctography. On the other hand, MR proctography has the specific advantages of avoiding use of ionising radiation which makes it typically the favoured modality in younger females, provides higher spatial resolution and better soft-tissue contrast, and also evaluate the anterior and middle compartments [3].
Findings and procedure details of fluoroscopic proctogram
The main indication for fluoroscopic proctography is obstructed defecation with assessment of the pelvic floor for excessive descent, anterior rectocoele formation, recto-rectal intussusception / prolapse and enterocoele.
Before the procedure, it is very important to explain every step of it to the patient in order to make them feel comfortable and to be able to perform the examination correctly. The presence of a chaperone is also very helpful. Eliciting the clinical details from the patient is equally important and may help the accuracy of final diagnosis.
To achieve opacification of small bowel loops in fluoroscopic proctography, approximately 300ml of oral barium suspension is given 45 minutes prior to the beginning of the procedure. This is useful for the diagnosis of possible enterocoele (loops of small bowel in the pelvis). An initial digital rectal examination is performed with the patient in left lateral decubitus position in order to assess the tone of the sphincter complex and to confirm the safety of inserting a rectal tube. Approximately 200-300ml of thick barium paste is injected into the rectum via the tube. The entire examination is recorded through videofluoroscopy. Several video recorded images are obtained in left lateral and in supine positions with the patient responding to requests of ‘squeeze up’, ‘bear down’ and ‘cough’. This is to evaluate the response to increased intra-abdominal pressure. Subsequently, the patient is asked to sit on a specially designed chair and is instructed to empty the rectum completely. This part of the procedure is also video recorded and additionally spot images taken. The whole examination lasts approximately 10-15 minutes. Evaluation of the posterior compartment (rectum) with assessment pelvic floor descent is assisted by using an imaginary line drawn in the lateral views from the pubic bone anteriorly to a fixed segment of coccyx posteriorly (Figure 1).
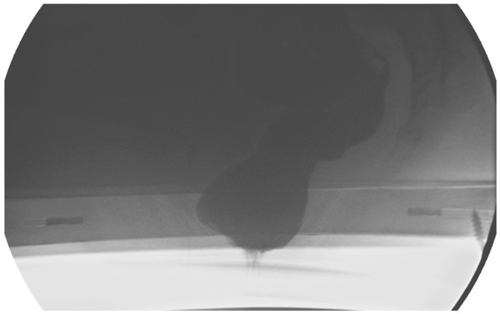
Figure 1a: Baseline on fluoro proctogram.
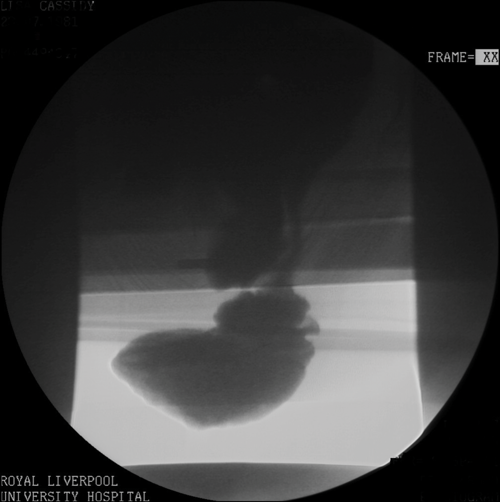
Figure 1b: Pelvic floor descent with an enterocoele.
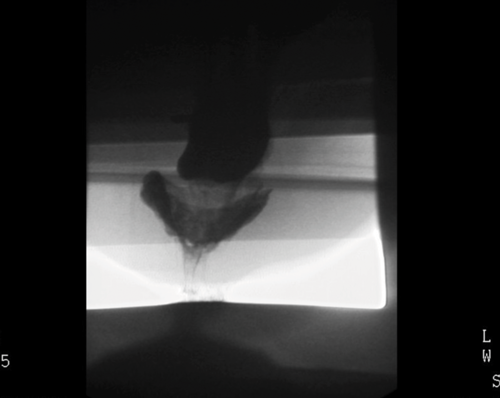
Figure 1c: Intussusception on fluoro proctogram.
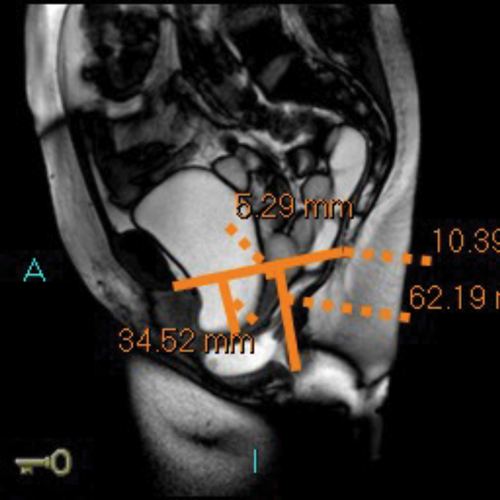
MR defecating proctograms are performed in a 1.5 Tesla MR scanner (Philips Sense). A similar detailed explanation of the procedure and consenting process takes place, so the patient knows what to expect during the three ‘cine’ scans of ‘squeeze up’, ‘bear down’ and ‘empty out’. The urinary bladder must be empty as far as possible during the MR scan.
After an initial digital rectal examination, 120mls of ultrasound jelly is instilled into the rectum via a rectal tube with the patient in the left lateral position. The patient is then turned to lie supine and positioned so that the top of the Sense-body coil is at same level with the iliac crest. The MRI scan protocol includes T2 axial and coronal sequences and sagittal ‘cines’ squeeze, bear down and two defecatory attempts with a couple of minutes rest in between. In cases of incomplete evacuation, a repeat evacuation may be needed or a coronal cine.
In addition the anterior and middle compartment is assessed, particularly for the presence and anatomy of a cystocoele or vault prolapse. The T2 sequences also allow pelvic evaluation for other incidental pathologies (Figure 2).
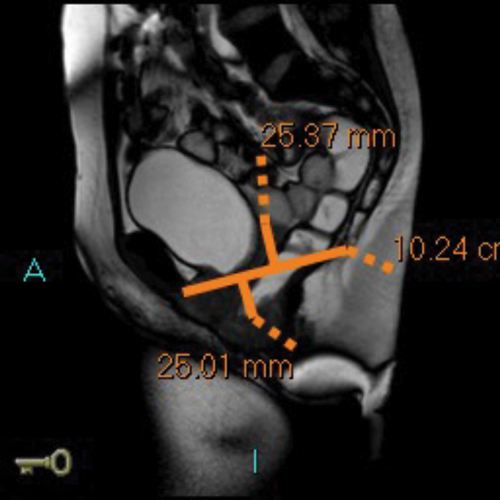
Figure 2a: Baseline MR proctogram.
Figure 2b: Pelvic floor descent MR proctogram.
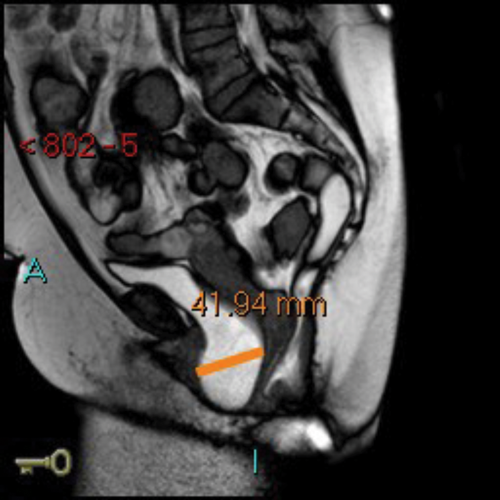
Figure 2c: Large cystocoele MR proctogram.
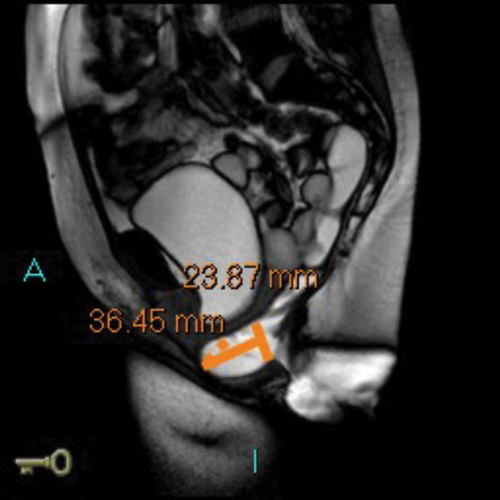
Figure 2d: Large rectocoele on MR proctogram.
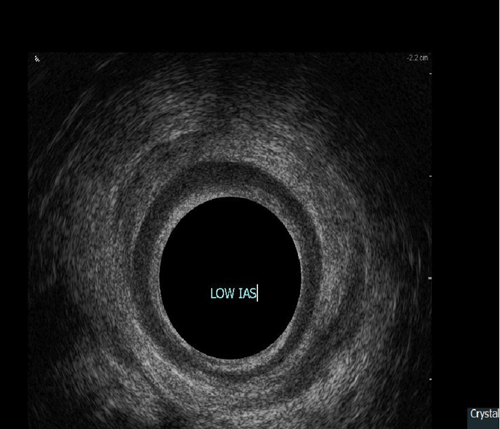
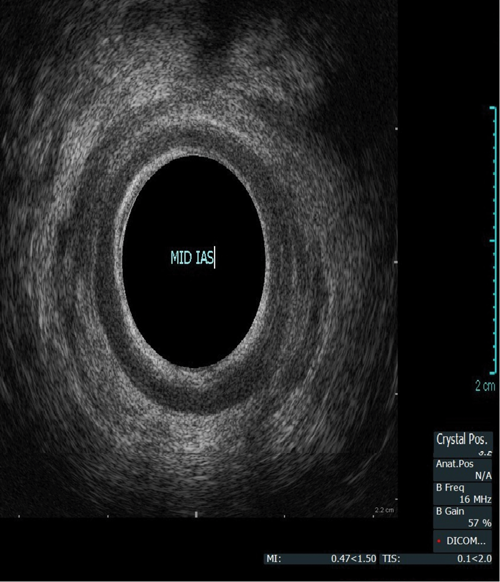
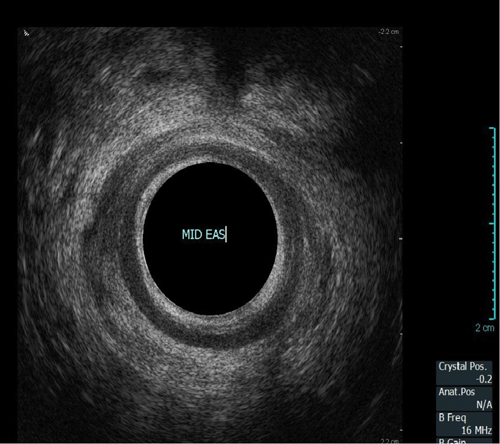
Endoanal ultrasound
This procedure is indicated for assessment of the anal sphincter in patients with incontinence. This allows evaluation of the internal and external anal sphincters (sphincter thickness, length and scarring). It is pertinent to obtain history of obstetric trauma as well as any surgeries / intervention to aid assessment.
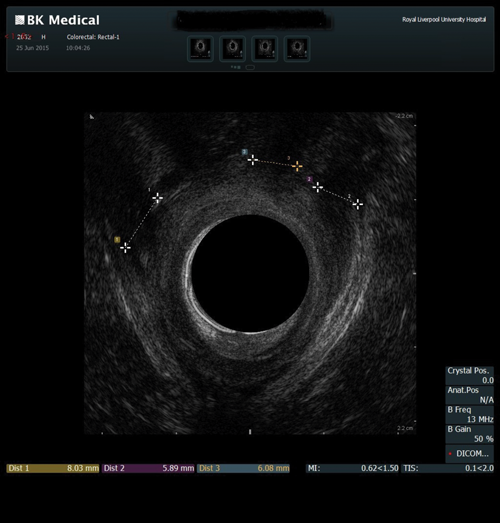
As with the proctogram technique, the procedure is explained in detail and consent obtained prior, and the presence of a chaperone makes the patient more comfortable. Digital rectal examination is performed as a reference to assess anal tone. Still images as well as cine of the ultrasound are taken to assess the sphincter complex (Figure 3).
Figure 3a: (Top, middle and bottom) Normal endoanal ultrasound.
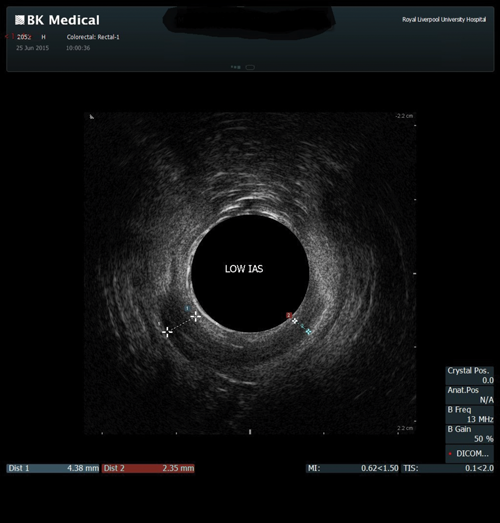
Figure 3b: Abnormal / deficient low internal anal sphincter.
Figure 3c: High External anal sphincter scars due to obstetric trauma.
Summary
Pelvic floor imaging is an important part of colorectal, functional urology and uro-gynaecological management of patients, particularly in females as the symptoms of urinary / faecal incontinence and prolapse have a significant impact on the quality of life. Proctography and endoanal ultrasound play an important part in diagnosis and management when this is used in conjunction with good history-taking and physical examination findings.
References
1. Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 1997;89:501-6.
2. Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of gastrointestinal disorders: prevalence, sociodemography, and health impact. Dig Dis Sci 1993;38:1569-80.
3. Tunn R, Paris S, Taupitz M, et al. MR imaging in posthysterectomy vaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 2000;11:87-92.