Physiotherapy should be included in first-line management options for pelvic organ prolapse and urinary incontinence in women [1,2]. Additionally, referral to physiotherapy is widely practised for the management of urinary incontinence in men, faecal incontinence, defecation disorders and various pelvic pain conditions in both men and women.
Readers may routinely refer their patients for physiotherapy as per national or speciality association guidelines or accepted best practice [2,3]. If the referring medical practitioner, whether a GP, urologist, urogynaecologist or colorectal surgeon, has an in-depth understanding of what specific treatments involve and what skills the physiotherapist has to offer, the adherence to treatments by the patient may be much improved. The referring practitioner is encouraged to explain to patients why they are being referred to physiotherapy, helping to create a dynamic and integrated framework of care in which the patient actively engages with their conservative management. Adherence to a pelvic floor muscle training (PMFT) programme will be improved if the patient understands the rationale for referral and the referrer has considered other potential barriers to compliance such as time restraints and family commitments [4,5].
What is physiotherapy, and what does a physiotherapist do for pelvic floor dysfunction?
The training and expertise required for this specialist area will be acquired primarily at a postgraduate level, as the opportunity to gain experience at undergraduate level is very limited. Many of the physiotherapists in the UK working in continence care and pelvic floor dysfunction are members of Pelvic Obstetric and Gynaecological Physiotherapy (POGP), a professional network of the Chartered Society of Physiotherapy (CSP) offering training and support, and providing a benchmark for excellence in this clinical area. POGP is one of the biggest and oldest special interest groups of the CSP. In spite of this the level of awareness of the exact role of the pelvic floor physiotherapist remains low amongst other physiotherapists, health professionals and the public; it is not uncommon for patients with continence or prolapse to be surprised that they have been referred to physiotherapy and they wonder what might be asked of them, perhaps something similar to when they had their babies: ‘pelvic exercises’, or they arrive ready for mat-based exercises.
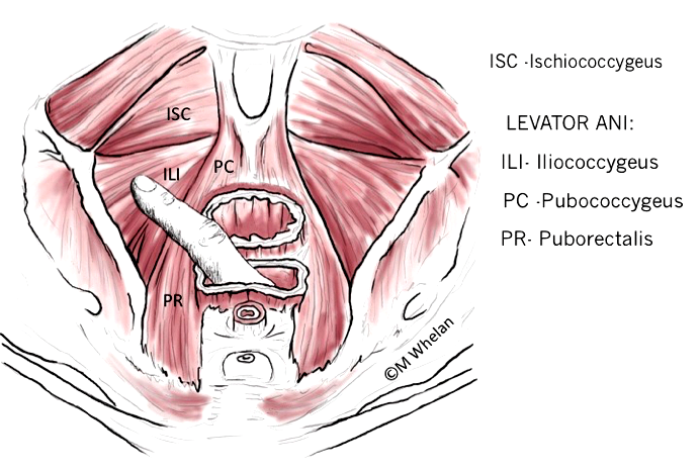
Helping patients to understand exactly what the pelvic floor muscles do and where they are can be an important first step in learning that specific pelvic floor muscle exercises may help. Physiotherapists perform vaginal and rectal examinations as part of the pelvic floor assessment similar to the in depth assessment of the function of any other part of the body, such as a knee or the back.
Various definitions of physiotherapy include:
- “Physiotherapists help people affected by injury, illness or disability through movement and exercise, manual therapy, education and advice.” (CSP)
- “Physiotherapy helps restore movement and function when someone is affected by injury, illness or disability. It takes a holistic approach that involves the patient directly in their own care.” (NHS Choices)
- Finally, the Collins dictionary defines physiotherapy as: “the therapeutic use of physical agents or means.”
In the context of treating men and women with bladder and bowel symptoms of pelvic floor dysfunction, what then is physiotherapy?
The basic tenets of form and function underpin pelvic physiotherapy, and the emphasis is on knowledge of normal anatomy and function in order to promote a better understanding of dysfunction. Rehabilitation is the process of regaining function using these first principles.
Many specialist physiotherapists in this area have undergone theoretical and practical training, often using each other as models, so they become highly competent in vaginal and rectal examination [6]. This unusual learning method, not adopted by any other medical or allied health professional body, affords key benefits in the context of developing an understanding of and skills related to empathetic and therapeutic relationships: “do unto others as you would have them do to you”, a maxim much quoted, less often practised.
Pelvic floor evaluation
The vagina is a suspended muscular tube held in place by the fascial, muscular and ligamentous structures of the endopelvis with functions related to sexual intercourse, menstruation, and childbirth. The urogenital hiatus is the largest potential hernial portal of the body [7].
The rectum is a muscular tube reflected backwards beyond the anal canal at the anorectal junction, remaining empty until loaded prior to defecation. Deferment of defecation should be possible with the anal sphincters providing closure and squeeze pressure to assist the stool to return to the upper rectum until a suitable time for bowel opening occurs.
The anatomical basis for pelvic floor muscle disorders is assessed by performing a pelvic floor muscle assessment by vaginal or rectal examination. A detailed assessment of the form, function and efficacy of the biomechanics relating to continence, defecation, pelvic organ support and pain is undertaken. Some of the key questions asked in this evaluation are: Are the muscles weak? Do the muscles generate sufficient closure? Are the superficial pelvic floor muscles overworking? Is there adequate fascial support? Is there asymmetry of muscle bulk or sensation?
The detailed subjective assessment will include gaining information about bladder, bowel, pelvic organ prolapse, sexual and pain symptoms.
The objective assessment begins with a detailed visual inspection, noticing asymmetry, puckering, tension, poor perineal quality or descent, obvious prolapse or noticeable skin problems.
The palpating finger can determine muscle strength, power, endurance, bulk and asymmetry. Additionally, information can be gained about fascial tension, pain, and stiffness. Finally, by use of an active cough, bearing down and positioning, the ability of the pelvic floor complex to operate in functional positions can be determined. Other modalities of assessment can be used – such as perineometry, and dynamic ultrasound. Several studies have been conducted to assess inter and intra-rater reliability of digital vaginal assessment, and compared with manometric or other forms of assessment. In general, there is good intra-rater reliability allowing the digital assessment of muscle function to be an objective measure within a treatment programme. Some studies have also found similar results for anal pressure testing in men [8,9].
Pelvic floor muscle assessment
- With the finger under the pubic bone following the line of the urethra and asking the patient to contract her pelvic floor muscles is there sufficient pressure to generate a closure force felt at the urethral level? If yes, can this closure force be maintained whilst coughing?
- With the finger resting on the posterior vaginal wall, left and then right of midline, does the pelvic floor muscle contraction generate lift and indrawing of the palpating finger?
- If there is asymmetry of muscle strength, can the patient feel the difference?
- Does the levator ani attachment anteriorly at the pubic bone feel the same left and right?
- Does deeper, anatomically specific palpation reproduce the patient’s pain or trigger a referred pain that has been reported in the subjective history?
- If there is a prolapse visible at the introitus, can the action of the pelvic floor muscles withdraw the descending wall or cervix?
- With the finger in the rectum and asking the patient to bear down, does the anorectal angle adjust and the external anal sphincter relax mimicking the normal defecation pattern?
- In standing, can the pelvic floor muscle action achieve vaginal closure and a reduction of the hiatal opening?
- If there is no stress leakage on cough in supine, but poor urethral stability, does the patient leak on coughing in standing?
Following assessment, the physiotherapist will record pelvic floor muscle strength and function, and if relevant, areas of pain and grading of pelvic organ prolapse. In common practice, physiotherapists will grade muscle function using a combination of the modified Oxford scale as used in the PERFECT scheme [10] and the International Continence Society (ICS) recommended grading system [11] (Table 1 and 2).
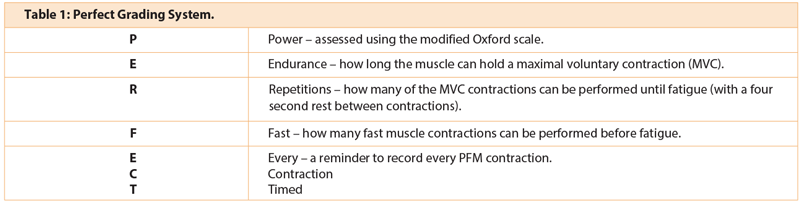
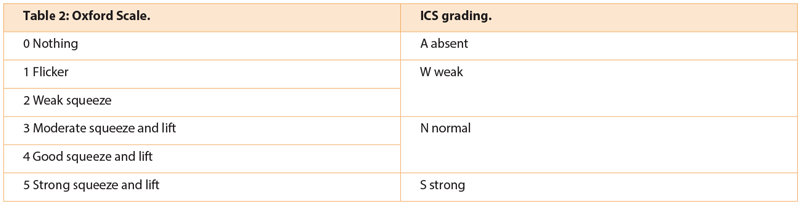
The Oxford scale is widely used but in pelvic floor muscle assessment has been shown to have variable inter-rater reliability. The Laycock PERFECT scheme uses the modified Oxford scale but has additional components that allow a better assessment of the function of the muscles including endurance, and quality of the fast contraction. This becomes relevant when trying to teach the ‘Knack’ (a precontraction of the pelvic floor muscles prior to an increase in intra-abdominal pressure) for symptomatic improvement of leakage on a rise of abdominal pressure [12].
“Explaining the concept of pelvic floor muscle exercises in terms of re-education, and retraining for function can be empowering.”
Crucially the ICS recommendation for muscle assessment includes whether the muscle can relax fully after maximal contraction. Relaxation of the pelvic floor muscles is a key factor in normal voiding of bladder or bowel. A pelvic floor muscle with high resting tone which neither contracts nor relaxes normally, may be the cause of voiding dysfunction with symptoms often reported as incomplete emptying, repeat voids and possibly urinary tract infections (UTIs). Dyspareunia may also be a symptom, less often reported until specifically asked.
Areas of pain and abnormal tension can be recorded on an anatomical chart.
Management
At this point the physiotherapist has gained valuable clinical information, the value of which lies in whether the patient can be helped to understand the link between symptoms and findings. The patient may already have seen the GP, possibly one or more consultant appointments, perhaps urology or gynaecology, with information and explanations probably offered at each point of contact. Medication and advice may have been given and onward referral made. The role of conservative management is to assist the patient with gain symptomatic relief and improved quality of life. Reported ‘cure’ rates in studies vary, quoting up to 70% in some, but it is generally agreed that a 55% cure rate is possible with intensive pelvic floor muscle exercises maintained for a six-month period [13].
Consider a patient with stress urinary incontinence who leaked a little with every cough or sneeze, and on rising from the sofa. Her pelvic floor muscles were graded as normal (ICS scale) / four (Oxford Scale) but the fast contraction lacked power and the squeeze was felt more in the superficial pelvic floor muscles. Initial retraining involved correcting the pelvic floor muscle technique with palpation, cueing the muscles with the instruction “draw upwards and forwards from the back passage towards the front bone” [16]. Subsequently, the ‘knack’ was taught to improve urethral closure which counteracts the rise in abdominal pressure that occurs on rising to standing from sitting. If a real time ultrasound machine is available, the urethral movement can be demonstrated to the patient, and the correct muscle action may be taught and seen.
Several studies show that in the longer term the initial symptomatic improvement is not maintained over longer time periods [14,15]. There is a need for further studies to assess the benefit of ongoing pelvic floor muscle training and to determine the optimal length of time for intervention and at what point and by whom. The physiotherapist is in an excellent position to help make the connections for the patient between symptoms and clinical findings. Using patient-friendly terminology, good visual aids and highlighting short-term improvements gained is likely to improve adherence to the management programme.
Patients can be very quick to condemn their own bodies – “I’ve got no pelvic floor muscles left”, “it’s all open down there” – and the men often have no concept of having a pelvic floor at all. It can be hugely reassuring for the patient following a detailed assessment to hear that there are indeed muscles, and that much of their anatomy is very normal. Explaining the concept of pelvic floor muscle exercises in terms of re-education, and retraining for function can be empowering.
Many women defer seeking help for stress urinary incontinence, either thinking that it is normal after childbirth or due to embarrassment. They may self manage with fluid control, pads and reduced activity. They may also try to use their pelvic floor muscles ‘to keep things tight’. Long periods of holding muscles tight can leave them stiff and unresponsive and unable to release. These women may report symptoms of dyspareunia, where they feel that their partner is ‘hitting something’ or they may have post coital discomfort. Careful vaginal examination can demonstrate to the patient that the muscles are held tight and short, creating a muscular hurdle during penetrative intercourse. Learning to relax the pelvic floor muscles allows more comfortable penetration.
Current guidelines for the management of urinary incontinence recommend a course of intensive supervised pelvic floor muscle exercises. Table 3 below summarises some of the recommendations from published guidelines, reviews and patient information sources [2,3,13,17,18].
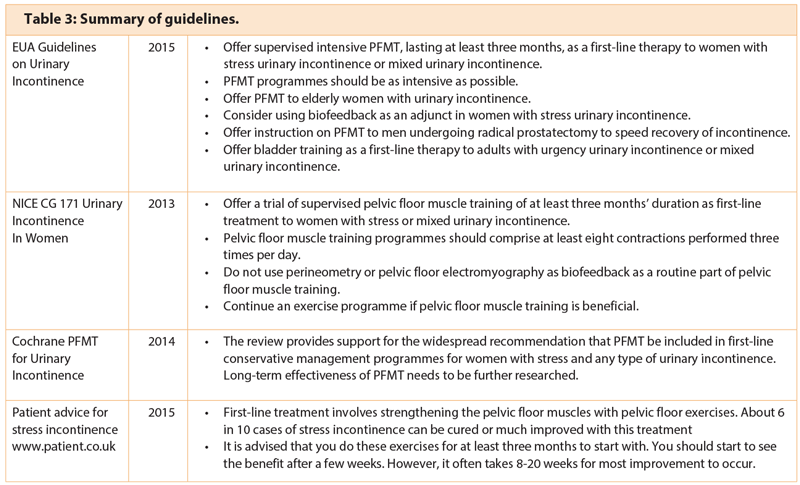
Further recent recommendations suggest that specialist physiotherapy as part of a multidisciplinary team should be included in the early management of chronic prostatitis / pelvic pain syndrome [2].
Recent evidence from the POPPY trial has shown that pelvic floor muscle exercises are effective for improvement of pelvic organ prolapse. This large, multicentre, randomised controlled trial (RCT) used a pragmatic intensive pelvic floor muscle training programme delivered by experienced physiotherapists. The study group received five physiotherapy appointments over a 16-week period with a vaginal examination at each appointment to adjust the PFM exercises. Longer term outcomes are yet to be fully reported [1].
Conservative management of pelvic floor disorders will include a supervised patient-specific pelvic floor muscle exercise programme reviewed at regular intervals and lifestyle advice about weight loss, constipation, fluids, lifting and suitable activity. The pelvic floor muscle assessment for a patient with pelvic organ prolapse will identify what type of prolapse and whether the pelvic floor muscle contraction is effective in reducing the prolapse and urogenital closure. Helping the patient to understand that the lack of vaginal support can explain the bladder or bowel symptoms – particularly incomplete emptying – may be a key factor in compliance with pelvic floor muscle exercises.
Conclusion
This article gives a snapshot of what a specialist physiotherapist working in the area of pelvic floor dysfunction does. More information about the range of clinical work covered by members of POGP is available at pogp.csp.org.uk. Most physiotherapists are very happy to come and talk to doctors and other health professionals about what they do. Sharing information about the roles of other health professionals can only benefit the patient pathway, improve compliance and lessen confusion.
Acknowledgement:
Figure is courtesy of Maeve Whelan.
References
1. Hagen S, Stark D, Glazener C, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. The Lancet 2014;383:796-806.
2. NICE Clinical Guideline 171:Urinary Incontinence in Women. 2013.
3. European Urology Association Guidelines on Urinary Incontinence. 2015.
4. NICE Medicines Optimisation Overview. 2015.
5. Dumoulin C, Frawley H, McClurg D; ICS Round table Committee. Adherence of Physical Therapy of the Pelvic Floor. 2012. Accessed from www.ics.org
6. CSP. Information Paper PD 092: Pelvic Floor Examination CSP expectations. 2012.
7. Dietz HP, Wong V, Shek KL. A simplified method for determining hiatal biometry. ANZJOG 2011;51:540-3.
8. Ferrera CHJ, et al. Inter-rater reliability study of the modified oxford grading scale and the peritron manometer. Physiotherapy 2011;97(2):132-8.
9. Frawley HC, et al. Reliability of pelvic floor muscle strength assessment using different test positions and tools. Neurourology and Urodynamics 2006;25(3):236-42.
10. Laycock J, Jerwoord D. Pelvic floor muscle assessment: The PERFECT scheme. Physiotherapy 2001;87(12):631-42.
11. Messelink B, et al. The standardization of terminology of pelvic floor muscle function and dysfunction. Report from the pelvic floor clinical assessment group of the International Continence Society. 2005.
12. Miller JM, Ashton-Miller JA, Delancey J. A pelvic floor muscle precontraction can reduce cough-related urine loss in selected women with SUI. J Am Geriatr Soc 1998;46:870-4.
13. Dumoulin C, Hay-Smith EJC, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014;5.
14. Agur W, Steggles P, Waterfield M, Freeman R. The long-term effectiveness of antenatal pelvic floor muscle training: eight-year follow up of a randomised controlled trial. BJOG 2008;115:985-90.
15. Glazener CM, MacArthur C, Hagen S, et al.; ProLong Study Group. Twelve-year follow-up of conservative management of postnatal urinary and faecal incontinence and prolapse outcomes: randomised controlled trial. BJOG 2014;121(1):112-20.
16. Crotty K. Investigation of optimal cues to instruction for pelvic floor muscle contraction: a pilot study using 2D ultrasound imaging in pre-menopausal, nulliparous, continent women. Neurourology and Urodynamics 2011;30:1625-31.
17. http://patient.info/health/stress-incontinence
Accessed 21 July 2015.
18. Rees J, Abrahams M, Doble A, Cooper A, and the Prostatitis Expert Reference Group (PERG). Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU International 2015; [Epub ahead of print].
Declaration of competing interests: None declared.