Educational theories: how familiar are we with these theories and their application in our training? As a Simulation Fellow I have been involved in teaching specific procedural skills and running full immersion simulation sessions. This experience has exposed me to various teaching styles and has heightened my interest in clinical education where I have come across several educational theories.
Analysing the various theories has been intellectually stimulating but more interestingly it has encouraged me to question which of these theories I currently use or which I should adopt and why. How will understanding these theories impact both my teaching and my learning? Learning is a continuous process but with the introduction of the European Working Time Directive (EWTD) the time spent in training has become more limited. This has led to concerns regarding quality of training in surgery [1]. It is therefore hugely important to optimise training in this limited timeframe, especially when learning technical procedures.
In order to try to improve this learning, this article will examine two educational theories, Vygotsky’s constructive theory with learning within the zone of proximal development (ZPD) and Kolb’s theory of experiential learning, which I find particularly applicable to my experience of teaching simulation-based procedural skills.
Focus of educational theories: teaching or learning
What are educational theories aimed at – teaching or learning? Traditionally education focuses more on teaching than on learning [2]. The emphasis on teaching becomes so great that the purpose of it, which is for the student to learn, is somewhat lost. Hence, an attempt to understand educational theories and how their application impacts learning is a step towards re-establishing the focus of education on learning and how to best deliver this.
Oscar Wilde said “education is an admirable thing, but it is well to remember from time to time that nothing that is worth learning can be taught” [3]. This baffles me though – if it cannot be taught than how can it be learnt? Perhaps we learn by means other than traditional teaching, which are not that obvious? We should consider the learning process in relation to educational theories.
Learning within the ZPD
Learners play the principal role in the learning process in a constructivist theory [4] and hold the key to exploring and manipulating the learning environment [5]. To examine the constructivist theory, I will briefly illustrate the stages of learning within Lev Vygotsky’s ZPD [6,7] (Figure 1) and attempt to relate my experience to these stages.
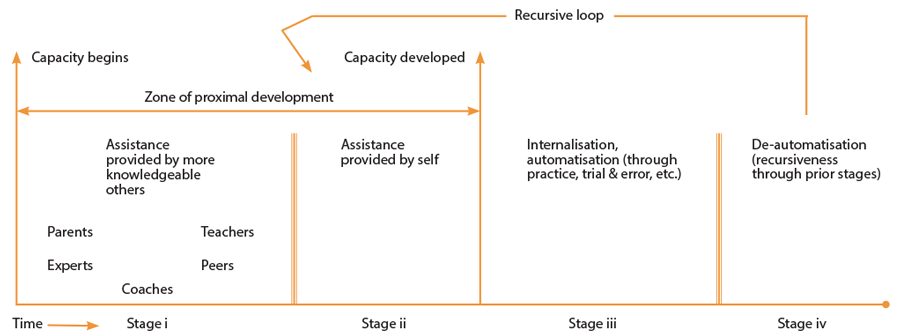
Figure 1: Modified version of Tharp & Gallimore’s Four-Stage Model of ZPD.
In order to relate this education theory to a practical medical education situation I will describe a simulated procedural skill session. I have recently been involved in teaching medical students how to perform rigid cystoscopy using pelvic trainer models and rigid cystoscopes. At the start the students had a vague awareness of the procedure and, following a very quick demonstration, were instructed to perform the procedure from assembly to endoscopy. What initially looked simple proved more challenging when the students attempted it. This was reflected by the support needed in most steps of the task. Clearly this fits in with the ‘other-assisted’ stage (Stage I) of learning within ZPD.
After some didactic teaching with a more detailed and slower demonstration of the task the learners were given time to practise. At first they sought support from the demonstrators but with more practice and application of the technical manoeuvres they soon became more relaxed and comfortable. Perhaps a valuable interactive social learning environment had been established; students attempted to overcome any difficulties themselves initially, sought help of peers next, and thereafter occasionally asked for expert advice when they felt it necessary. This, I believe, is when they transitioned to stage II within ZPD – ‘self-regulated’ learning where they identified where they needed more practice, and whether they needed help and from whom, until they felt confident. The pace of learning seemed much faster at this stage and appeared to be directly proportional to the degree of interaction.
The end of this stage I felt overlapped the stage III ‘internalisation of learning / automatisation’ when they were able to perform the task without assistance. In retrospect is it possible in simulation to establish to what extent learning has been internalised and if further assistance will be required? This is a procedure that will eventually be performed on a patient rather than a simulated model. To what degree will these skills be transferred from simulation to patient? How much support will be needed at the initial stages of skills transfer and thereafter?
These questions cannot be answered until skills transfer has taken place and may indeed vary from person to person. Although at some point performance may be consistent and reliable we cannot forget that every patient, their problems and anatomy may vary. From personal experience, in new or complicated cases, even seniors and consultants may need assistance and advice from experienced peers. As mentioned previously, learning is a continuous process and occurs at every stage of our practice. Then, how can we define when learning has actually been internalised or achieved? In the simulated environment learning is achieved when the learning objectives are met and assessed.
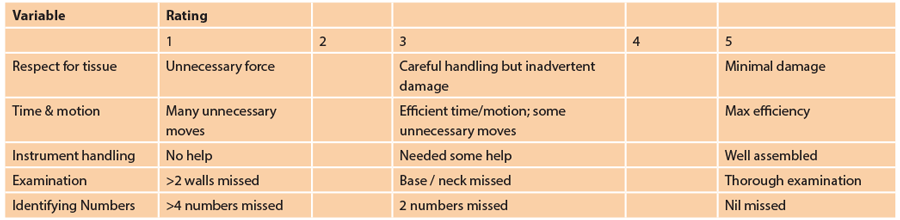
After the practice sessions, our learners were assessed on their performance using an adjusted global rating score (Appendix 1). Although all did well in the practice sessions, many struggled with the assembly of equipment which caused a staggered start. This seemed to have an impact in the endoscopic manoeuvres for some candidates. Perhaps the unexpected difficulty at the start of assessment caused undue stress and led learners to return to earlier ZPD. This relates to the ‘de-automisation’ stage (Stage IV) of learning with ZPD.
What I find fascinating is that most learners chose to practise the procedure itself and put less importance on learning the parts of the equipment and assembly. They chose what to learn in the self-regulated phase but re-enforced learning or where to improve when they struggled during assessment. In my opinion this suggests that assessment for feedback should be scaffolded much earlier, perhaps at the self-regulated phase. This will allow candidates to reflect and redirect their attention to improve their learning outcome.
“An attempt to understand educational theories and how their application impacts learning is a step towards re-establishing the focus of education on learning and how to best deliver this.”
That is what I believe will build a stronger social interaction for appropriately focused cognitive development. Although much of the stages of development lie congruent to Vygotsky’s constructivist theory there exists some areas that may not relate as visibly. Nonetheless, I believe that we cannot overlook the significance of the role of learners in the learning process and that reflective feedback lies at the heart of simulation-based learning. Teachers facilitate this learning pathway and attain some learning themselves in the process be it from reinforcement or from reflecting on others’ difficulties and actions.
Procedure-based simulation: experiential learning
To some extent contrary to the stages of learning in Vygotsky’s ZPD, Kolb & Kolb clarify that indeed learning is a continuous process (Figure 2) and involves the interaction of social and personal knowledge adapted appropriately to the environment [8]. Our example describes experiential learning with some integrated didactic teaching. As Albert Einstein said “the only source of knowledge is experience” [9] and through simulated cystoscopy the opportunity for experience, learning and above all social interaction to allow the learning has been created in a safe environment.
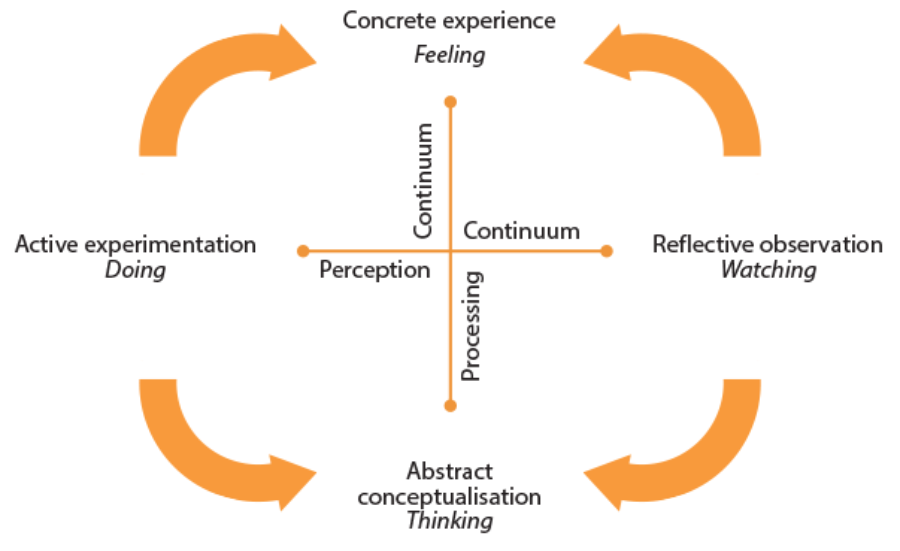
Figure 2: Modified version of Kolb’s experiential learning cycle.
If we recall from earlier, every patient, their problem and anatomy may differ. Reflecting even on this alone it seems that Kolb’s theory is tailored for the session and the challenges I have described. The cyclic pathway of learning (Figure 2) described by Kolb [10] provides flexibility and should allow for comfortable learning. A rigid education system deprives the learners of the opportunity to arouse interest and gain experience. Each of us learns differently and at a different pace. This model allows us to enter the cycle at different points based on our experience and comfort or convenience.
To expand on this, in our cystoscopy session some candidates entered the cycle at ‘active experimentation’ stage mimicking what had been briefly demonstrated and improving on the skills upon further demonstration and practice. At the other end of this spectrum some candidates could not undertake the procedure at all until formal demonstration was delivered along with some didactic teaching. Clearly, this group found it more effective to enter at the ‘reflective observation’ stage. In brief, the learners found their own entry point into this cycle with a common aim of learning how to perform rigid cystoscopy.
If it is possible to enter at any phase of this cycle then how would one enter at ‘abstract conceptualisation’? Is it possible in this day and age to learn a technical skill by logically analysing ideas and situations? Does this not place under scrutiny our ethics of treating patients by doing so? ‘See one, do one, teach one’ is a model that has come under scrutiny in the last decade [11] and even this model suggests that at least one should be seen before trying it out. The more I consider starting the learning process at ‘abstract conceptualisation’ the more convinced I am that this phase may not comply with the patient safety aspect that our learning as doctors is meant to provide; except perhaps if it were for research or novel purposes but only after ethical approval.
“A rigid education system deprives the learners of the opportunity to arouse interest and gain experience.”
We must not forget that it is often easier to learn than to re-learn what we have learnt wrong. As Dewey’s educational philosophy points out, experiences may promote or inhibit learning: “The belief that all genuine education comes about through experience does not mean that all experiences are genuinely educative….for some experiences are miss-educative” [12]. I agree with this statement which to my mind appears to be a predicament of the outcome of education if Kolb’s cycle is entered at ‘abstract conceptualisation’ (in relation to the specific cystoscopy session in question as opposed to a generalised educational session).
Regarding ‘concrete experience’, to an extent this overlaps ‘active experimentation’ in my particular session. Either way, I would like to think one of these phases accounts for the true experience when cystoscopy is attempted on patients. For true learning development to occur the procedure will have to eventually be carried out on a patient. However,I do not feel it is safe to encourage this as an entry point but rather a development phase, where learners will learn to deal with the challenges they come across either through observing, experimenting or seeking help.
Once again, this educational model can be applied to the teaching of rigid cystoscopy in simulated models but there may be a need for limiting the entry point within the learning cycle. In a different teaching experience,educational theories and their application would have to be varied with the situation.
Feedback: a tool for development of learning
So far we have only briefly brought up the term feedback. What is intriguing is its role in progressive development of learning. If we recall the assessment of medical students attending the cystoscopy session, many candidates struggled with assembly of equipment as they paid less importance to this. It was only at assessment that they reflected upon the significance of this aspect and its impact on the rest of the procedure. This was the student achievement from the assessment which has been used for feedback purposes. The scores of the assessment were used for a separate analysis and were not revealed to the students. Only reflection on the aspects observed were discussed regarding which they were briefed at the start of the day. Evidently, if feedback had been omitted there would have been an undetected gap in skill acquisition and in the bigger scheme a potential risk to patient safety in the future.
Christopher Watling once stated, “The problem in medicine is not a lack of human capacity for meaningful teacher–learner relationships, but, rather, a cultural failure to recognise the importance of such relationships and to create opportunities to nurture them” [13]. As the clinical educator, I learnt that I probably should have incorporated the feedback earlier in the practice session to direct the students’ learning according to development needs and to preserve their confidence.
Current status of simulation in urology teaching
I have only demonstrated an example of a specific simulation skill and selective educational theories. However, urology is at the forefront of minimally invasive surgery with a wide array of surgical and diagnostic modalities requiring varied skill sets. Numerous simulators are available to teach both technical and non-technical skills with evidence suggesting simulation-based training helps to bypass the early stages of the learning curve and many of its associated challenges. Hence, this is being increasingly utilised as a training tool with a recent proposal to incorporate it into the current urology training curriculum.
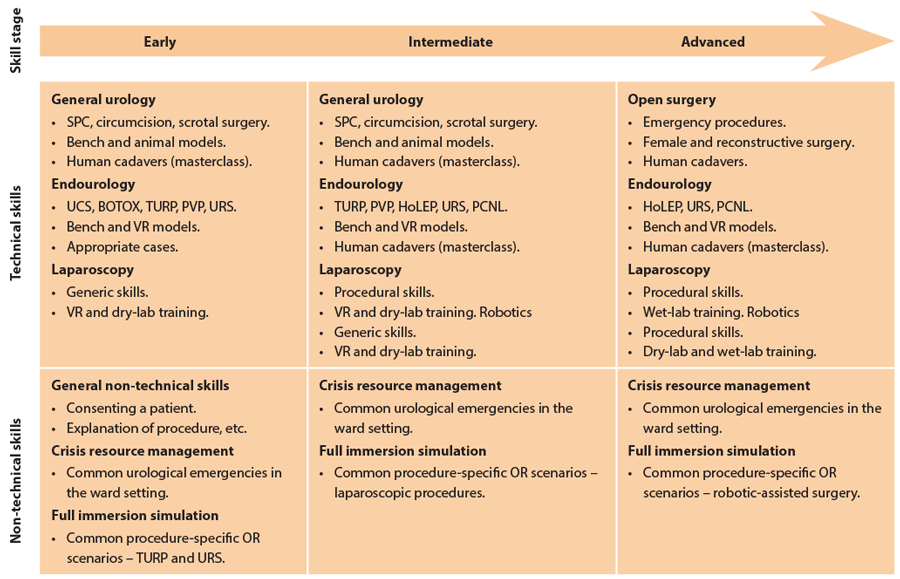
Figure 3: Recently recommended urology simulation training pathway by Abdullatif Aydin,
Nicholas Raison, Muhammad Shamim Khan, Prokar Dasgupta and Kamran Ahmed.
The suggested generic and additional proficiency-based simulation curriculum for urology training to enhance operating-room experience has been recently outlined in Nature Reviews Urology as demonstrated in Figure 3. With increased utilisation of these valuable educational adjuncts there is an increasing need to understand the effective integration of educational theories in order to optimise the outcome of both teaching and learning and to create a safe learning environment in true terms.
Conclusion
From my experience of teaching surgical procedural skills, I have begun to understand the different perspectives and depths of various educational theories. From my understanding of pedagogy it appears that adopting any one particular educational theory is exceedingly complex. With the increasing inclusion of simulation-based training as an educational adjunct there is an increasing need for understanding the principles of effective amalgamation of educational theories.
Although these theories help us explore what learning is about they interact like multiple facets of a fly’s compound eyes. Each facet of the eye sees a different perspective to give a multidimensional holoscopic view [15] thus suggesting that perhaps no one theory is superior to the other and consequently they have to be adapted to fit the teaching sessions. Undeniably this is in keeping with Kolb’s proposal of characteristic of experiential learning: “learning is a holistic approach of adaptation to the world and involves transaction between the person and the environment” [10].
As Sutkin suggests, “Excellent teaching, although multi-factorial, transcends ordinary teaching and is characterised by inspiring, supporting, actively involving and communicating with students” [16]. Hence, the learner is the core of the learning process and social interaction is the environment for it to prosper. Reflective feedback is a powerful tool that should be used appropriately to improve social interaction, aid proximal development and continued professional development.
References
1. ASGBI. The impact of EWD on delivery of surgical services, a consensus statement of the Association of Surgeons of Great Britain and Ireland. 2008. www.asgbi.org.uk
2. Ackoff R, Greenberg D. The objective of education is learning, not teaching; Turning education right side up: Putting education back on track. London, UK; Financial Times / Prentice Hall; 2008.
3. Wilde O.
www.quotesnsmile.com/quotes/
70-brilliant-oscar-wilde-quotes
4. Jonassen DH. Designing constructivist learning environments. In CM Reigeluth (Ed.), Instructional-design theories and models: A new paradigm of instructional theory Vol. II 1999:215-39.
5. Jonassen DH. Evaluating Constructivistic Learning. In Duffy TM, Jonassen DH (Eds.). Constructivism and the Technology of Instruction: A Conversation Hillsdale, USA; Lawrence Erlbaum; 1992:137-148.
6. Sanders D, Welk DS. Strategies to Scaffold Student Learning, applying Vygotsky’s Zone of Proximal Development. Nurse Educator 2005;30(5):203-7.
7. Tharp R, Gallimore R. Rousing minds to Life. Cambridge, UK; Cambridge University Press; 1988.
8. Kolb A, Kolb D. Learning Styles and Learning Spaces: Enhancing Experiential Learning in Higher Education. Academy of Management Learning & Education 2005;4(2):193-212.
9. Einstein A.
www.brainyquote.com/quotes/
quotes/a/alberteins148778.html
10. Kolb D. Experiential Learning: Experience as the Source of Learning and Development. 1984.
http://academic.regis.edu/ed205/kolb.pdf
11. Rodriguez-Paz JM, Kennedy M, Salas E, et al. Beyond “see one, do one, teach one”: toward a different training paradigm. The International Journal of Healthcare Improvement 2009;
http://qualitysafety.bmj.com/
content/18/1/63
12. Dewey J. Education and Experience New York, USA; Simon and Schuster; 1938;25-8.
13. Watling C, Driessen E, van der Vleuten CP, Lingard L. Learning culture and feedback: an international study of medical athletes and musicians. Medical Education 2014;48:721-3.
14. Aydin A, Raison N, Shamim Khan M, et al. Simulation-based training and assessment in urological surgery. Nature Reviews Urology 2016;13:503-19.
15. Aggoun A. 3D holoscopic imaging technology for real time volume processing and display. In: Mrak M, Grgic M, Kunt M (Eds.). High-Quality Visual Experience Germany; Springer; 2010:411-28.
16. Sutkin G, Wagner E, Harris I, Schiffer R. What makes a good clinical teacher in medicine? - A review of the literature. Academic Medicine 2008;83(5):452-66.
Declaration of competing interests: None declared.
Appendix 1: Adjusted Global Rating Scale for assessment of cystoscopic skills.




