Introduction
Testicular microlithiasis (TML) was originally described in 1970 in a healthy four-year-old boy [1] and the first paper regarding microlithiasis as an entity seen on ultrasound was published in 1987 [2]. Testicular microlithiasis is seen on ultrasound as small, non-shadowing hyperechoic foci of calcification ranging in size from 1 to 3mm. The widely accepted definition is where five or more foci of microcalcifications are seen in a field of view. Microlithiasis may cluster within the testis, or be seen throughout the visualised testicular tissue on ultrasound.
The European Society of Urogenital Radiology (ESUR) established a Scrotal Imaging Working Group in 2012 and the committee has written guidelines regarding follow-up of patients with testicular microlithiasis [3], which were recently published. This article aims to describe the most salient points of the guidelines.
Testicular ultrasound Ultrasound is generally the first imaging modality used in assessment of the testis. It does not involve ionising radiation, is relatively cheap, and quick to perform and can give a patient an immediate answer, often in the form of reassurance as the majority of palpable lesions are found to be benign. A high frequency, linear probe is used and images of high resolution should be obtained.
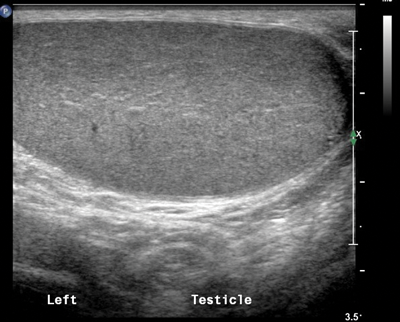
Figure 1: Longitudinal section through the left testis showing uniform echogenicity.
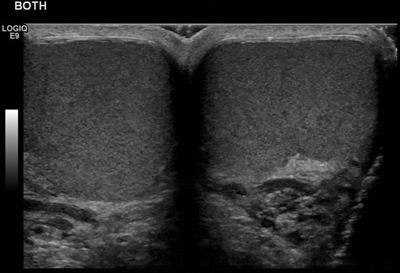
Figure 2: Transverse section through the midline showing both testes are of the same echogenicity.
When performing testicular ultrasound, each testis should be examined individually to assess echogenicity and any focal lesion should be thoroughly examined to ascertain whether it appears benign or aggressive. The testis should be of uniform echogenicity as shown in Figure 1. Colour Doppler should be applied to ensure both testes have adequate vascularity. Any focal lesion should be assessed with colour Doppler to ascertain if a lesion is hypo- or hypervascular.
Both testes should be compared in the transverse plane, as the testes should be of a similar size and echogenicity (Figure 2) and direct comparison between the two testes is advised as part of routine ultrasound.
The epididymis should be assessed on each side and then the operator should scan the scrotum by angling the probe both laterally and medially to assess for the presence of a varicocele.
Representative images of normal testicular and epididymis architecture should be taken as well as images of any focal lesion. Although ultrasound is operator dependent and a dynamic investigation, relevant images should be saved so clinicians can view them and, where necessary, used for comparative purposes in the future.
Testicular microlithiasis
Testicular microlithiasis is a condition of unknown aetiology where calcium deposits form in the lumina of seminiferous tubules or arise from the tubular basement membrane components. The microliths are asymptomatic, do not cause pain, and are so small that they are impalpable.
Testicular microlithiasis is most commonly diagnosed by ultrasound, as the microliths are clearly identified as hyperechoic foci which do not demonstrate posterior acoustic shadowing, less than 3mm in size. Different definitions exist about the diagnosis of microlithiasis, but the most universally accepted definition is that five of more microliths are seen per field of view on ultrasound (Figure 3). When testicular microlithiasis is widespread and seen throughout the testis, it is described as a ‘snow-storm’ appearance [4].

Figure 3: Longitudinal section of the right testis showing microlithiasis,
with more than five microliths seen in the field of view.
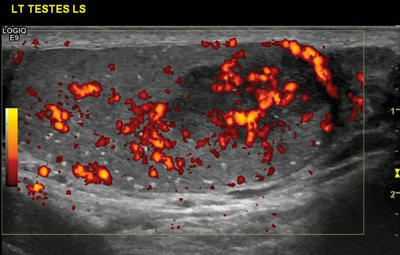
Figure 4: Same patient as Figure 3 showing a tumour in a patient
with bilateral microlithiasis. In this case, follow-up US is advised.
Although MRI is increasingly used in imaging of the testes, microliths are not clearly visible on this imaging modality as calcification, even when large in size.
With recent advances, ultrasound machines are able to produce higher resolution images, making testicular microlithiasis more clearly visible. Earlier literature reported that the incidence of microlithiasis on scrotal ultrasounds is approximately 0.6% and is usually an incidental finding [5].
Previously, there was evidence that suggested that testicular microlithiasis increased a patient’s risk of developing a germ cell tumour and annual ultrasound surveillance had been recommended. A study performed by Cast et al. on 4819 patients suggested that microlithiasis is strongly associated with germ cell tumours [6] but other studies have failed to confirm this association, which therefore suggests that the condition is benign [7].
No formal guidelines existed regarding the need and frequency of ultrasound follow-up in patients found to have microlithiasis and different departments adopted local policies.
ESUR Scrotal Imaging Working Group
The ESUR Scrotal Imaging Working Group was asked to review the current evidence in order to formulate guidelines for radiologists and urologists regarding the need for ultrasound surveillance if microlithiasis is detected. The committee consisted of experts from both Europe and America who wrote the guidelines following extensive literature review as well as discussions, both at face-to-face meetings and via email. All members of the subcommittee agreed on the guidelines prior to publication.
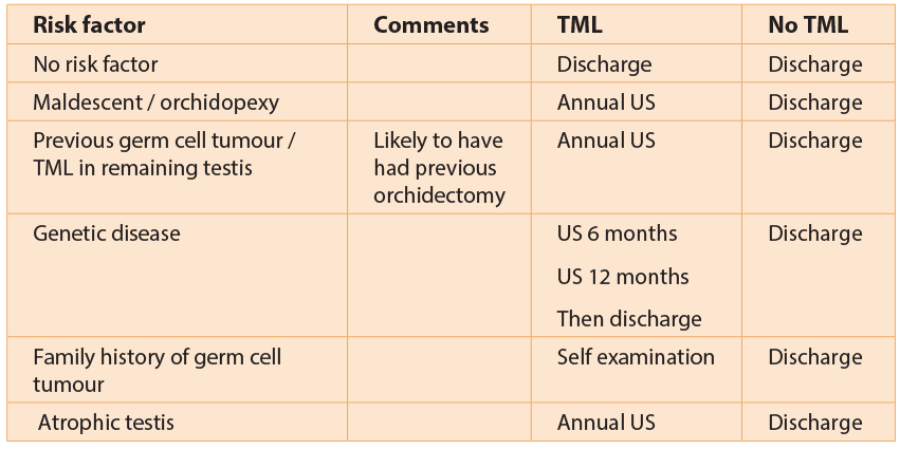
ESUR Scrotal Imaging Working Group Guidelines state that annual ultrasound should only be performed in patients who have an independent risk factor for developing a germ cell tumour.
Risk factors for germ cell tumours
Known risk factors for germ cell tumours include history of a previous germ cell tumour in the contralateral testis, history of maldescended testis or orchidopexy, a history of a germ cell tumour in a first degree relative, atrophic testis and Klinefelter’s syndrome.
In patients with risk factors for germ cell tumour who are found to have testicular microlithiasis on ultrasound, the ESUR Scrotal Imaging Working Group guidelines state that ultrasound should be performed annually until the patient reaches the age of 55 years, after which the risk of developing a germ cell tumour decreases.
In patients with no risk factors, regular self-examination is advised and if the patient develops a palpable mass, ultrasound should then be performed. In patients with no risk factors for germ cell tumour who are found to have microlithiasis, routine ultrasound surveillance is not recommended, as the risk for developing a tumour remains very small.
If a focal lesion is seen in either testis, then referral to a specialist centre for further investigation is advised. This may include tumour markers, further imaging with repeat ultrasound or MRI, or orchidectomy depending on the clinical and ultrasound findings.
The following table has been designed by the ESUR Scrotal Working Group to aid follow-up advice given to patients.
Conclusion
Annual ultrasound in patients found to have microlithiasis is only recommended if there is an independent risk factor for the patient developing a germ cell tumour. In other cases, self-examination is advised and if a palpable lesion develops, ultrasound should then be performed.
References
1. Priebe CJ Jr, Garret R. Testicular calcification in a 4-year-old boy. Pediatrics 1970;46:785-6.
2. Doherty FL, Mullins TL, Sant GR, et al. Testicular microlithiasis: a unique sonographic appearance. J Ultrasound Med 1987;6:389-92.
3. Richenberg J, Belfield J, Ramchandani P, et al. Testicular microlithiasis imaging and follow-up: guidelines of the ESUR scrotal imaging subcommittee. Eur Radiol 2015;25(2):323-30.
4. Roberts IS, Loughran CF. Case report: the ultrasound appearances of testicular microlithiasis ‘snow-storm’ testis: a case complicated by testicular seminoma. Clin Radiol 1993;47(L1):65-7.
5. Bennett HF, Middleton WD, Bullock AD, Teefey SA. Testicular Microlithiasis: US Follow-up. Radiology 2001;218:359-63.
6. Cast JE, Nelson WM, Early AS, et al. Testicular Microlithiasis. Prevalence and Tumour Tisk in a Population Referred for Scrotal Sonography. AJR 2000;175(6):1703-6.
7. Richenberg J, Brejt N. Testicular microlithiasis: is there a need for surveillance in the absence of other risk factors? Eur Radiol 2012;22(11):2540-6.





