The physician associate (PA) is a new role in the NHS which has expanded across medical and surgical specialties to include urology. In the USA, it has long been an established field of practice where physician assistants work autonomously within defined levels of supervision. In the USA, the term ‘physician assistant’ is used whereas in the UK they are called ‘physician associates’.
Two definitions of the physician associate / assistant are as follows: The first definition is provided by the Yale School of Medicine:
“Physician assistants or physician associates (PAs) typically obtain medical histories, perform examinations and procedures, order treatments, diagnose diseases, prescribe medications, order and interpret diagnostic tests, refer patients to specialists as required and first or second assist in surgery”.
The second definition is provided by the Department of Health, Curriculum and Competence Framework (2006):
“A new healthcare professional who, while not a doctor, works to the medical model with the attitudes, skills and knowledge base to deliver holistic care and treatment within the general medical / general practice team under defined levels of supervision”.
History of the physician associate
Providing healthcare has been a challenge for many centuries. Before the physician assistant role was first established in the 1960s, non-physicians have been used in many countries across the world. The most notable use of non-physicians was in Russia where a lack of co-ordinated medical care was commonplace. ‘Feldshers’ (a term coined by the Germans) were used as field surgeons and were first introduced into the Russian army in the 17th century. These non-physicians were mainly trained in battlefield medicine and still exist today. They continue to practise in former East Soviet bloc countries, such as Ukraine, undergoing a three-year course (two years non clinical, one year clinical).
During World War II, Dr Eugene Stead from the USA developed a fast-track three-year medical curriculum for medical students. Following the war and into the 1960s, he modified this and made his intentions clear to develop a physician assistants programme using former military corpsmen. In 1965 the first physician assistant educational programme was inaugurated at Duke University. They took on four former military corpsmen. As interest grew, physician assistant programmes were established at many medical institutions. To date, the American Registry of Physician Assistants (ARPA) regulates training and quality assures the programmes.
Currently in the USA, the programme is 26 months and divided into didactic, clinical and research elements. The first year is mainly classroom-based with problem based learning (PBL); this self-directed learning approach makes up most of the learning in the first year. Intertwined with the classroom-based learning is the GP placement which is offered one day a week. Here the student can demonstrate their knowledge and practise their history taking and examination skills. The final year is predominantly clinical, giving the student exposure to all the main clinical specialities. This enables the student to apply the knowledge gained from the first year and start developing management plans for patients. To date, there are around 170 physician assistant programmes and over 100,000 physician assistants working across the country.
In the UK, in 2003 the Department of Health led a taskforce and recruited 33 pilot American physician assistants. Initially based within primary care in the Midlands, these pilot physician assistants established the United Kingdom Association of Physician Associates in 2005. The Association was developed in order to promote the role and the development of the profession. In 2005, the first physician associate programme was set up in the University of Hertfordshire and enlisted seven students. As interest grew, further institutions developed their own programmes and currently St George’s University (London), Wolverhampton, Birmingham, Plymouth, Worcester and Aberdeen all conduct programmes. It has been agreed that by 2016, four further universities (Anglia Ruskin, Leeds, Reading and Sheffield Hallam) will deliver training in physician associate programmes.
Currently physician associates maintain a voluntary register. All physician associates who work within the UK are required to join the register and employers make registration a mandatory condition of appointing a physician associate.
USA physician assistants
At present in the USA there are around 4000 physician assistants working in urology, they are autonomous in their field and have gained a wealth of experience; some are performing TRUS biopsies, urodynamics, flexible and rigid cystoscopy, and ureteric stent removals independently. Due to the ever increasing number of physician assistants in urology the Urology Association of Physician Assistants (UAPA) was developed in 2011. The organisation was set up to advance and promote the profession.
One-year residency programmes for physician assistants in urology have also been developed across the USA. These programmes touch on clinical, research and educational aspects of urology. The first six months are spent rotating around the subspecialties areas of urology (BPH, lower urinary tract symptoms, stone and mineral metabolism, urologic oncology, reconstructive urology, etc). The second six months provide dedicated operating time in addition to first assistant training. This covers a wide variety of robotic urological procedures.
Why hire a physician associate?
A physician associate is a permanent member of the medical team and, whilst not a doctor, is educated in a similar manner and to follow a similar approach. PAs have been trained to be experts in the evaluation and management of common diseases and to recognise life-threatening medical conditions. They work within the medical team to make sure that patient safety is protected; if the PA realises that the patient illness is beyond the scope of their training, they will transfer the care of that patient to their supervising doctor.
All PAs hold at least a bachelor’s degree, usually in a life science or healthcare related area and most PA programmes require a 2:1 honour degree for entry into a postgraduate diploma course / master’s course.
Physician associates are employed on a permanent basis either in primary or secondary care. PAs have not been practising in the UK for many years but in the USA the role itself is well established as previously mentioned. PAs in the USA hold their post, on average, for approximately five to six years [1]. This length of time spent in a speciality can be seen as invaluable as the individual will learn new skills and provide patients with a highly specialised continuity of care. PAs also develop long-standing relations with the MDT such as nurses, pharmacists, social workers and physiotherapists.
Limitations / drawbacks
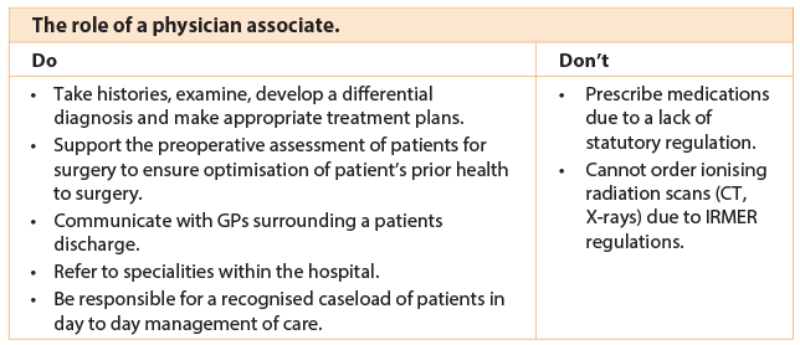
PAs in the UK are currently not allowed to prescribe medication which was similar to the early days in the USA. PAs have an extensive knowledge of pharmacology as they have to sit a pharmacology exam within their training. It is only due to the lack of statutory regulation that they are currently unable to prescribe. Close working with supervising physicians and arrangements within the team allow for flexible working practice.
As well as prescribing PAs are unable to order ionising radiation. The Ionising Radiation (Medical Exposure) Regulations Act (IRMER) was amended in 2006 and states that only registered healthcare professionals are able to order ionising radiation.
Accreditation
Unlike any other clinical profession there is a clear described national curriculum framework which was constructed by the Department of Health committee. This committee was made up of the Royal College of General Practitioners, the Royal College of Physicians, junior doctors, employers and patients. Once the PA has passed their two-year postgraduate course they have to maintain their continuing professional development in addition to passing their national assessment every six years. It is mandatory to pass this assessment to stay on the managed voluntary register.
The future of physician associates in the UK
The United Kingdom Association of Physician Associates was dissolved in May 2015 to become the Faculty of Physician Associates at the Royal College of Physicians (RCP). This is the first time in the Royal College’s 500-year history that a non-doctor has entered into the faculty. This new organisation will take over managing the voluntary registry as a well as accrediting future PA programmes.
As stated earlier the physician associate profession is a voluntary registered profession, which means that at present the profession cannot prescribe. This has been an issue since the early days of the profession and the frustration has been highlighted on more than one occasion by different journal articles [2,3]. These articles highlight the benefits and pitfalls of the physician associate. There are a few reasons why the profession is not regulated at present; one is partly due to the number of physician associates that are currently working in the National Health Service. At present there are around 240 working across the UK in primary and secondary care. The cost of implementing regulation for such a small number would be deemed not cost-effective. The recent government manifesto highlights the need for seven day working across primary/secondary care. This is being achieved with the recruitment of more physician associates. This will happen in two-fold:
- By increasing the amount of university programmes running a physician associate course.
- Setting up a programme called the National Physician Associate Expansion Programme (NPAEP).
The NPAEP is a transformational programme run by the NHS, the main aim of which is to recruit a large number of physician associates / physician assistants from the USA and deploy them across four regions of the UK. The intention is that recruiting the US-trained physician assistants on a two-year temporary contract will help build up the workforce in the UK and then UK PAs will eventually replace the US-trained PAs.
The future of physician associates in urology
At present there are two urology physician associates working in the UK*. Both are currently employed by St George’s Hospital in London. As physician associates are trained to the medical model they can provide an extension to the medical workforce.
Urology is a varied speciality which encompasses both elements of medicine and surgery. Physician associates can help deliver a safe, efficient and effective service. As cancer diagnostic service waiting times continue to decrease it is important that safety and efficiency standards are adhered to under these increasing time pressures. Physician associates can help with this pathway as they can gain the skills to run pre-assessment clinics / haematuria clinics and assist in theatre with emergency and routine cases. By being able to provide this increased scope of skills, valuable training time is created for junior doctors on the ward.
It is important to create awareness throughout the UK so that more PAs are employed in the field of urology. In doing this the profession can develop a specialist professional body just as the USA have developed theirs. In this way PAs, working alongside other medical professionals, can help to shape their career and develop a specialist training curriculum (dependent of course upon PA regulation and registration).
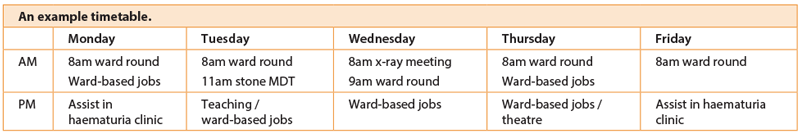
An example timetable
The table above provides an example of a physician associate’s timetable in St George’s. At present there is a blank canvas as to what a physician associate could achieve and every opportunity for development of the PA role in urology should be explored.
Feedback on the PA role in urology
“Acts as an aid to bridge the gap and enhance communication within members of the multi-disciplinary team.”
Ward Sister, St George’s Hospital
“Available on the ward and know the patients very well therefore able to answer queries effectively and appropriately. PAs add a valuable input towards the team.”
Pharmacist, St George’s Hospital
*At time of going press (Nov/Dec 2015) this could be three, however we are unclear if this person has been appointed.
References
1. Graeff EC, Wallace L, Stewart G, Leafman JS. Job satisfaction levels of physician assistant faculty in the USA. The Journal of Physician Assistant Education 2014;25(2):15-18.
2. Williams LE, Ritsema TS. Satisfication of doctors with the role of physician associates. Clinical Medicine 2014;2(2):113-16. Accessed from
http://static1.squarespace.com/static/
544f552de4b0645de79fbe01/t/
54b54238e4b0362b2df60f3c/
1421165112507/
Doctor_satisfaction_with_PA’s%281%29.pdf
9 August 2015.
3. Drennan V, Halter M, Brearley S, et al. Investigating the contribution of physician assistants to primary care in England: a mixed-methods study. Health Serv Deliv Res 2014;2(16).
Declaration of competing interests: None declared.