
Bladder washouts are a treatment usually employed by the urology team, more often in an inpatient setting, and commonly indicated for haematuria with clot retention and catheter bypassing [1,2]. Bladder washout is a cornerstone of treatment in urology wards, yet often the skill is expected of junior urology doctors and nurses who learn the technique on the job.
The transition in skillset is more marked when rotating junior doctors change from one job to another and are called upon to undertake washouts out of hours with little experience of the specialty. This demands rapid training for the incoming doctors and nurses. An anonymised survey of 45 clinical staff members on our ward, revealed poor rates of confidence with bladder washouts (44%), and only 11% of the cohort reported having had formal teaching in the procedure. This has led to an ongoing quality improvement project with development of formalised modular training. In this article we describe our method of performing bladder washouts which trainee staff may find helpful.
Equipment
Prior to doing a bladder washout the practitioner should ensure that the required equipment is at hand, as listed below (we use this list for our teaching sessions [3]):
- Personal protective equipment (PPE)
- Bottle of sterile normal saline 0.9% (1L)
- Sterile jug
- 60ml bladder-tip syringe
- Kidney dish
- Collecting vessel
- Sterile gloves
- Incontinence pads
- Spigot
- Antiseptic wipe / wet wipes
- Bladder scanner (optional)
- A chaperone / assistant

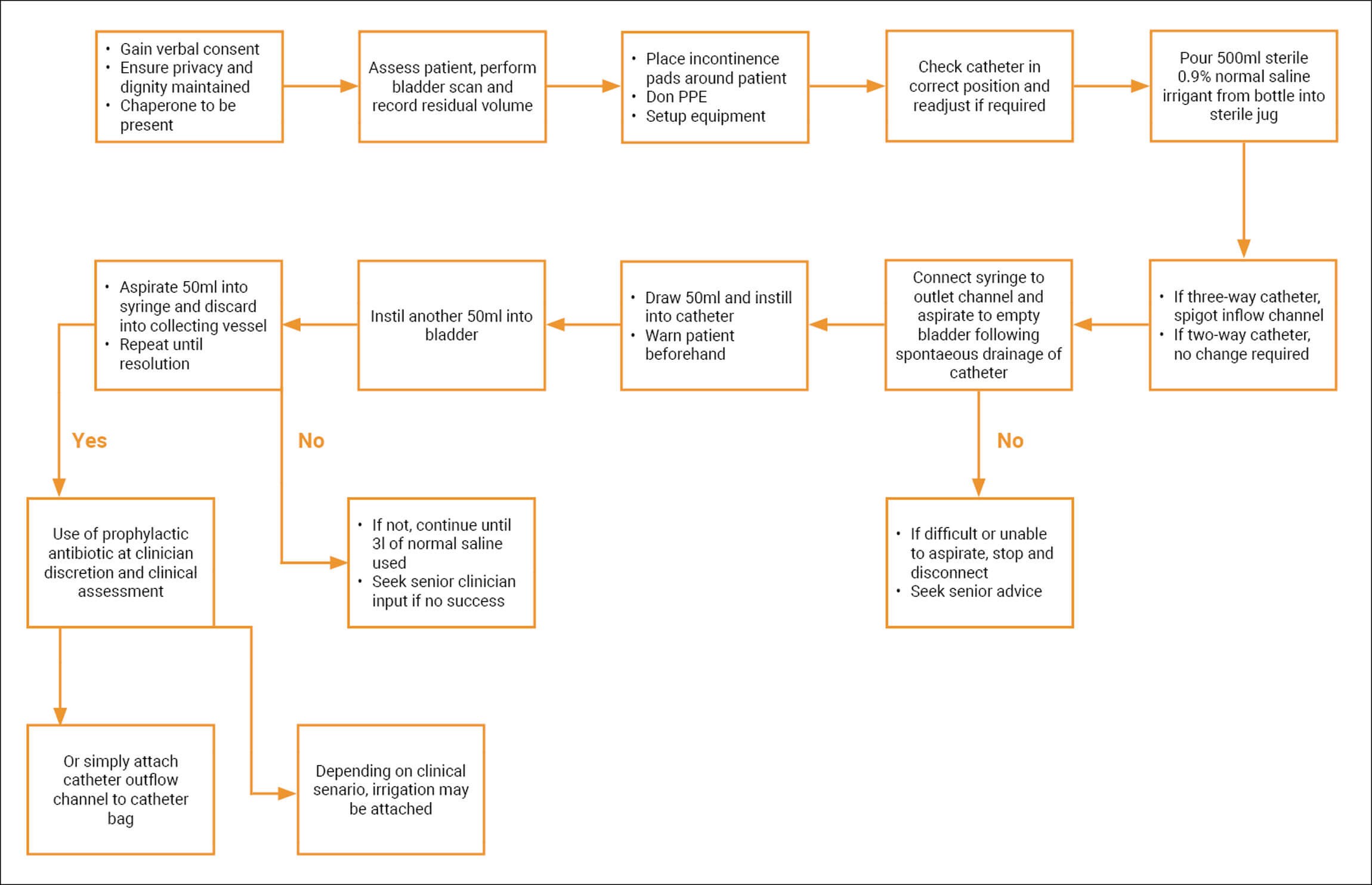
Key steps
The steps described below for performing a bladder washout have been approved and implemented at our department:
- Gain verbal consent.
- Ensure privacy and dignity are maintained. Offer a chaperone.
- Assess the patient and if a bladder scanner is available, perform and note the post void bladder scan residual volume.
- If the patient attends with new-onset clot retention, ensure washout is done as soon as possible following three-way catheter insertion.
- Place incontinence pads underneath patient and in the working environment to contain any spillage.
- Don the appropriate PPE and ensure hand hygiene.
- Ensure equipment setup on field and next to dominant hand.
- Before proceeding; ensure that the catheter is in the correct position and readjust if needed. Let catheter drain bladder to completion freely.
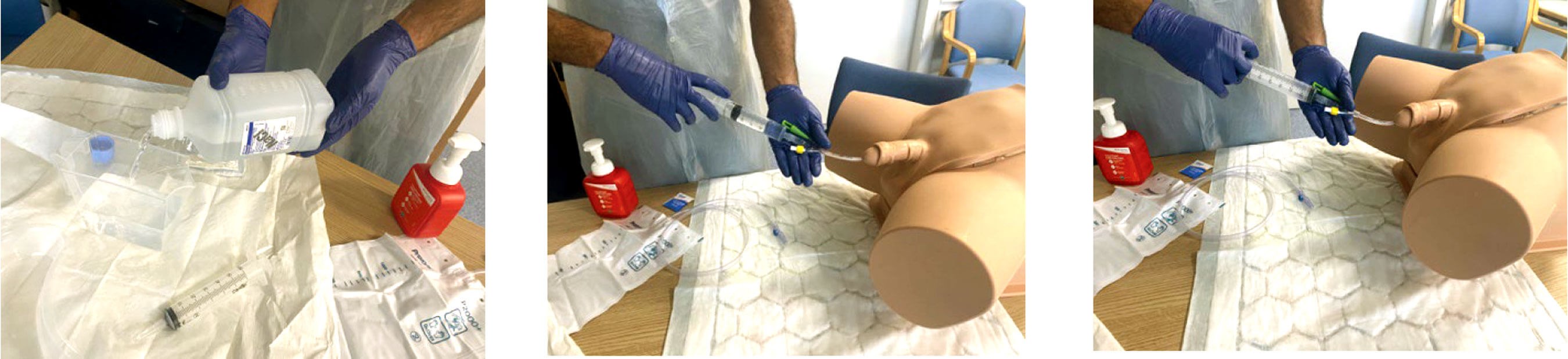
- Pour 500ml of sterile saline irrigant from the bottle into the sterile jug.
- If the patient is on irrigation with three-way catheter, stop the irrigation. Disconnect the line, and place spigot into the third (inlet) channel. If patient has a two-way catheter, disconnect catheter bag from the catheter, when you are about to start the bladder washout.
- Once catheter position in the bladder is confirmed, connect the bladder tip syringe to the catheter outlet channel and gently aspirate to empty the bladder. If difficult or unable to aspirate, stop and review as recommended in the troubleshooting section below.
- Draw up 50ml of normal saline irrigant into the bladder tip syringe, connect to catheter outlet channel and instil gently all 50ml inside. Please warn the patient of discomfort before doing so.
- Repeat the above step. The aim is to insert 100ml into the bladder if the bladder is empty. Ensure the bladder volume is under 200ml before attempting to instil any further fluid.
- Using the syringe to aspirate, withdraw the fluid aiming for 50ml into the syringe. Discard into the collecting vessel.
- Repeat Steps 12 -14, until you are satisfied that clear urine is draining and all clots have been extracted.
- If the urine is not clear or clots still persist, seek senior (registrar / consultant) advice.
- Use of prophylactic antibiotic will be at the discretion of the clinician and the clinical assessment, such as in a traumatic catheterisation.
- Ensure that the catheter bag is emptied regularly and not allowed to be full.
- Depending on clinical scenario (expected ongoing haematuria) attach irrigation immediately to inflow channel in a three-way catheter.
Troubleshooting
If concerned at any point, stop and seek senior advice. Ensure that the catheter is correctly placed in the bladder. This can be determined by techniques including free movement of catheter, ease of bladder washout and position of the catheter being inserted to the hilt in males. If in doubt seek senior advice.
Common difficult scenarios
I can instil irrigant but can’t aspirate anything on a washout
Either the catheter is blocked with a clot or the tip of the catheter is pushed against the bladder wall (mucosal suction).
Try putting another 50ml of saline in to dislodge a clot and to push the bladder wall away from the tip of the catheter. Do not allow the volume in the bladder to exceed 250ml. Pull the catheter back a little and rotate it to move it away from the bladder wall.
This may also help to dislodge any clot and prevent the tip of the catheter abutting on the bladder wall.
Deflate the catheter balloon, remove the catheter and carefully advance the catheter tip into the bladder, reinflate the balloon only when sure about catheter position. Standard inflation of three-way catheter balloon is to 20ml for this purpose.
I have washed out the bladder and the aspirated fluid is clear but when I attach the catheter bag, nothing is draining
The catheter may be blocked. Please check to ensure the catheter is correctly sited in the bladder, and that it is patent.
The bladder may be empty, insert another 50ml of saline and reconnect the catheter bag.
Try a further washout to confirm position.
The patient is finding the procedure very uncomfortable
This isn’t uncommon. Some patients will find the distension of the bladder uncomfortable. Ensure the catheter is correctly sited in the bladder. Ensure the bladder volume is under 250ml. Instil the irrigant very gently if there is pain on instilling fluid. Warn them before every instillation of irrigant fluid during washout. If the patient cannot tolerate it and the catheter is blocked, the catheter will need to be changed.
Extra caution needs to be taken, along with senior expertise, in postoperative patients including bladder outlet obstruction surgery (e.g. TURP / TURis, etc), transurethral resection of bladder tumour (TURBT), radical prostatectomy, as well as patients with a history of bladder injuries and neobladders.
Regular bladder washouts interrupt the closed drainage system and should only be undertaken if the risk of obstruction is greater than the risk of infection associated with interrupting the closed system.
In situations where the catheter needs to be maintained, especially once the patient is discharged home to the community, certain instillation solutions may be used to minimise catheter-associated infections or catheter blockages. There is inadequate high-level evidence to advocate the use of such instillations [4]. Before considering the use of any catheter maintenance solution, it is important to make an individual assessment of the patient, and identify the clinical indication for its use.
References
1. Evans A, Godfrey H. Bladder washouts in the management of long-term catheters. Br J Nurs 2000;9(14):900-6.
2. Getliffe KA. Bladder instillations and bladder washouts in the management of catheterized patients. J Adv Nurs 1996;23(3):548-54.
3. Geng V, Cobussen-Boekhorst H, Farrell J, et al. EAUN Evidence-based Guidelines for Best Practice in Urological Health Care: Catheterisation, Indwelling catheters in adults, Urethral and Suprapubic. 2012
https://nurses.uroweb.org/guideline
/catheterisation-indwelling-catheters
-in-adults-urethral-and-suprapubic/
[accessed 29 September 2022].
4. Shepherd A, McKay W, Hagen S. Washout policies in long-term Indwelling urinary catherisation in adults. Cochrane Incontinence Group. Cochrane Database Systematic Reviews 2017;3(3):CD004012.
Declaration of competing interests: None declared.










