The NHS Nightingale Hospital London was launched in response to the COVID-19 pandemic. In mid-March 2020, the predicted scale of the pandemic was uncertain and there was concern that COVID-19 might overwhelm existing intensive care unit (ICU) capacity within weeks. This was an exceptional situation and demanded a fast-paced response.
Illustration by Madeleine Floyd.
Within two weeks, the ExCeL conference centre in east London was converted into a 500-bed ICU, designed to provide critical care to intubated and ventilated patients from overwhelmed local hospitals. In an unprecedented effort, over 2000 volunteers and staff were trained to work in pandemic conditions at the NHS Nightingale Education and Training Centre (from 30 March to 6 May, 38 days). The NHS Nightingale Hospital London remained open for 36 days at the height of the pandemic (from 3 April to 8 May), treating 54 critically unwell COVID-19 positive patients with 34 successful discharges and 20 deaths. The hospital currently remains on ‘stand-by’, ready to resume operations if needed.
The University College London Hospital (ULCH) urology department responded to a call from Health Education England (HEE) to join the NHS Nightingale Education and Training Centre faculty. The faculty included healthcare workers and educators from a wide range of backgrounds, specialties and geographic areas. The education centre was guided by the following principles: i) patient safety; ii) staff physical and psychological wellbeing; iii) effective communication between team-members; iv) evidence-informed practice [1].
Staff who volunteered to work at NHS Nightingale Hospital London would attend a comprehensive induction course at the Education and Training Centre (including local orientation, basic / advanced life support, personal protective equipment, simulation stations, communication skills, staff wellbeing, other clinical skills). Volunteer staff members came from a variety of different backgrounds, ranging from non-healthcare workers (e.g. airline employees) to healthcare professionals with varying levels of critical care experience. The induction course would be targeted to the self-reported experience of volunteer staff members, who were divided into groups (‘Green’ = critical care background; ‘Amber’ = non-critical care hospital staff; ‘Red’ = non-healthcare background).

Clinical Nurse Practitioner Mariya Dragova teaching management of difficult urethral catheterisation.
The faculty members were briefed on the evolving concept of the NHS Nightingale Hospital London and it was quickly apparent that this unique ‘field hospital’ environment would pose challenges to urological nursing and medical care. All patients would arrive to the facility with indwelling urethral catheters (IDC) in situ. Accidental IDC removal (with the balloon inflated) is estimated to occur in 2-5% of ICU patients (0.34 per 100 catheter days), causing urethral trauma which can make IDC reinsertion difficult [2]. Furthermore, patients would commonly be repositioned prone (‘proning’) to improve their oxygenation, thereby exposing patients to further risk of IDC dislodgement. There was no immediate plan for provision of operating theatre facilities or equipment (e.g. cystoscopy). There would be an on-site interventional radiology service, with the ability to insert ultrasound-guided suprapubic catheters (SPC) at the bedside if needed.
It was clear that easy troubleshooting of difficult IDC re-insertion would be essential for frontline staff on the ‘shop floor’, given that some patients would not be suitable for SPC (e.g. due to coagulopathy, prior abdominal surgery or high body mass index, BMI) and there would be no on-site operating theatre capacity. Thromboembolic disease requiring anticoagulation [3] and high BMI (>30) [4] appeared to be more common in COVID-19 positive ICU patients, making any potential SPC insertion less straightforward. Moreover, age and male gender are well-known risk factors for difficult urethral catheterisation and also proved to be risk factors for severe COVID-19 infection requiring ICU admission [4]. As the situation evolved, the UCLH urology department also volunteered to provide an on-call consultant urologist rota for clinical cover and to develop standard operating procedures (SOPs) (e.g. catheter care, catheterisation, paraphimosis, haematuria).
“It was quickly apparent that this unique ‘field hospital’ environment would pose challenges to urological nursing and medical care”
The urology aim from an educational perspective was to prevent and manage complications of urethral catheterisation, including accidental IDC removal, catheterisation-associated urethral injury (CAUI) and catheter-associated urinary tract infection (CAUTI). Implementation of education programmes has been shown to reduce CAUI and CAUTI [5-7]. We also sought to equip frontline qualified non-urology staff with a safe algorithm for difficult IDC re-insertion, adapted from the UCLH Male Catheterisation Guideline. After inadvertent IDC removal at the NHS Nightingale Hospital London, the algorithm recommends that an experienced clinician should make a single attempt at reinsertion with a 16Fr Foley catheter, followed by a further attempt with the Urethral Catheterisation Device (UCD®) (Urethrotech). The on-call urology consultant should be contacted if these two attempts at catheter reinsertion are unsuccessful. The UCD® incorporates an integrated hydrophilic nitinol guidewire into its design, making the safe and effective Seldinger technique easily accessible and available to non-urology frontline staff [8-10].
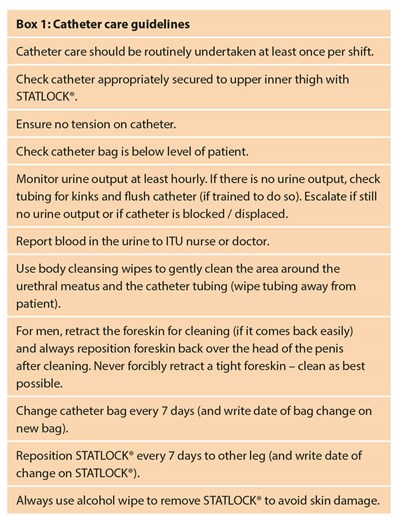
We developed educational resources for use at the NHS Nightingale Education and Training Centre. These included lesson plans (for ‘catheter care’ and ‘difficult urethral catheterisation’), short instructional training videos (accessible by hyperlink or QR code - see Figure 1) and laminated resource cards (Box 1: Catheter Care Guidelines and Box 2: Correct Male Urethral Catheterisation Technique).
Figure 1: Short instructional videos
• Catheter care: http://vimeo.com/405419828/bd4375f187

• Difficult urethral catheterisation with the Urethral Catheterisation Device (UCD®): https://vimeo.com/405474594/bafffd2e0b

The education centre made all lesson plans available to all volunteers on the ‘Induction app’ (accessible on smart phones). Volunteers were encouraged to review lesson plans and instructional videos ahead of their induction day, so that they could maximise their learning experience. Videos could be viewed from specific QR codes enabling them to be embedded into documents including SOPs.
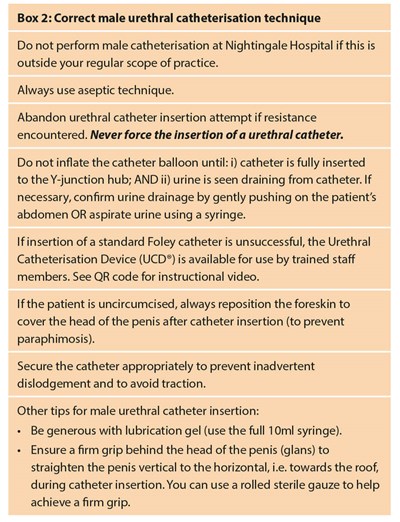
The UCLH urology faculty (including clinical nurse practitioners, urology trainees and urologists) delivered brief catheter education sessions (20 minutes) to small groups (up to eight students per group), who rotated between different ‘clinical skills’ stations relevant for that group. We tailored the education sessions to volunteer self-reported experience. For volunteers from non-healthcare backgrounds, often with no practical catheter experience, we focused on ‘catheter care’ (Box 1), which included instruction on appropriate catheter fixation using the STATLOCK® device (to prevent IDC dislodgement), awareness and management of the catheter bag during ‘proning’, urine output monitoring, troubleshooting catheter blockage, foreskin care, catheter hygiene and advice on when to escalate concerns. For volunteers whose scope of practice included catheterisation, we provided a brief training intervention to refresh and standardise best practice in standard urethral catheterisation (Box 2) to avoid complications of CAUI, CAUTI and paraphimosis. We made all volunteers aware of the algorithm for difficult IDC re-insertion, and we instructed selected experienced volunteers on the use of the UCD®.

Urology Fellow Nicola Jeffery teaching catheter care.
Educational resources and teaching methods were iteratively developed incorporating both feedback from volunteers, as well as clinical feedback from the NHS Nightingale Hospital London. For example, it soon became apparent that there were no sluice areas within the hospital, and so educational materials were updated to reflect this. Volunteers were instructed on waste management using absorbent crystals (Vernacare) and patient hygiene using body cleansing wipes. There was a shift towards case-based teaching, because this was favoured by volunteers. For the ‘Red’ groups, catheter care was combined with patient hygiene, fluid balance / documentation, faecal catheters and chest drains to form a ‘Fluids IN / Fluids OUT’ clinical skill station with case-based teaching.
In conclusion, the NHS Nightingale Hospital London and its Education and Training Centre was developed rapidly to meet the urgent needs of the COVID-19 pandemic and exemplified the volunteer spirit and dedication that supported London through this exceptional crisis. Through our involvement in this endeavour, we have shown that a short training intervention can be feasibly delivered on a large scale to healthcare workers to refresh best practice in urinary catheter care and urethral catheterisation skills. We demonstrated how it was possible to use simple video resources as pre-learning, to augment face-to-face sessions, be available to clinical staff and incorporate knowledge acquisition into SOPs. We believe that catheter education (tailored to job role) should be included in the induction programme for all NHS hospitals and should form part of the ongoing mandatory training requirement for all relevant staff members (similar to ‘Fire training’ and ‘Advanced Life Support’). Such education initiatives aim to reduce the incidence of preventable IDC complications, such as CAUI and CAUTI. At UCLH, we regularly run an ‘Advanced Male Urethral Catheterisation Course’, which we will seek to expand in the future.
References
1. NHS Nightingale Educators Resources. Health Education England. Accessible from:
https://www.hee.nhs.uk/our-work/
nhs-nightingale-educators-resources.
[Accessed 21 June 2020].
2. Lorente L, Huidobro MS, Martin MM, et al. Accidental catheter removal in critically ill patients: a prospective and observational study. Crit Care 2004;8:R229-33.
3. Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020;191:9-14.
4. Mahase E. Covid-19: most patients require mechanical ventilation in first 24 hours of critical care. BMJ 2020;368:m1201.
5. Loveday HP, Wilson JA, Pratt RJ, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86(Suppl 1):S1-70.
6. Kashefi C, Messer K, Barden R, et al. Incidence and prevention of iatrogenic urethral injuries. J Urol 2008;179(6):2254-7.
7. Sullivan JF, Forde JC, Thomas AZ, Creagh TA. Avoidable iatrogenic complications of male urethral catheterisation and inadequate intern training: a 4-year follow-up post implementation of an intern training programme. Surgeon 2015;13(1):15-8.
8. Bugeja S, Mistry K, Yim IHW, et al. A new Urethral Catheterisation Device (UCD) to manage difficult urethral catheterisation. World J Urol 2019;37(4):595-600.
9. Fluckiger S, John H. A new urethral catheterisation device for safe urethral catheterisation in difficult cases. J Clin Urol 2019;12(83).
10. Dragova M, Bamfo A, Holmes K, et al. Managing difficult catheterisation in nurse-led catheterisation services: Does guidewire-assisted urethral catheterisation make a difference? Int J Urol Nurs 2020;1-7.
Declaration of competing interests: Daniela Andrich has developed a Foley-catheter innovation to solve difficult catheterisation and brought to market the Urethral Catheterisation Device (UCD®) by setting up a Urethrotech Ltd., a medical device company, in order to provide healthcare providers and patients with a safe catheterisation solution. DE Andrich is the founder of the non-profit organisation Advanced Urinary Catheterisation Academy Ltd., to provide healthcare professionals with accredited training programs for advanced.
Acknowledgements: Thank you to all the UCLH urology volunteers: Sian Allen, Daniela Andrich, Hilary Baker, Tom Collins, Eoin Dineen, Mariya Dragova, Charlie Dunford, Helena Gresty, John Hines, Sabareen Huq, Nicola Jeffery, Wai Gin Lee, Angelica Lomiteng, Conor Mosli-Lynch, Clement Orczyk, Mahreen Pakzad, Pippa Sangster, Greg Shaw, Daron Smith, Anthony Ta, Mary Vincencio, Shafi Wardak and Dan Wood.













