Whilst the relatively random process of 12 core transrectal ultrasound guided (TRUS) prostate biopsy remains by far the most widely employed approach to prostate cancer diagnosis in the UK, its flaws as a standalone diagnostic strategy are increasingly apparent. TRUS-biopsy is an outlier in the diagnosis of cancer, with its lack of localisation by visual or imaging cues, the 12 core unguided deployment of needles has led to considerable errors in the pathway for diagnosing men with a suspicion of prostate cancer.
The ever criticised over-diagnosis of insignificant cancers along with their subsequent unnecessary treatment, the missed diagnosis of important cancers and the risk of 2-4% infection (some of which is life-threatening) all combine to make our current approach untenable.
Diagnostic performance will be considered at length below, but even in an article principally concerned with imaging, infection must at least be addressed. In an age where even the soberest of minds are making catastrophic predictions about antibiotic resistance and 300 million premature deaths by 2050 [1], a technique that is frequently repeated and relies on prophylaxis against numerous and often resistant bowel organisms merits careful consideration of strategies to replace it.
The use of multi-parametric MRI (mpMRI) for tumour identification and localisation has been growing for almost two decades but convincing level one evidence has been sparse, in no small part due to the heterogeneity of techniques, outcomes and reference standards. PROMIS [2] was conceived and delivered to fill this evidential void. In this article we discuss the findings of PROMIS within the context of the key evidence to date and the diagnostic improvements these should herald.
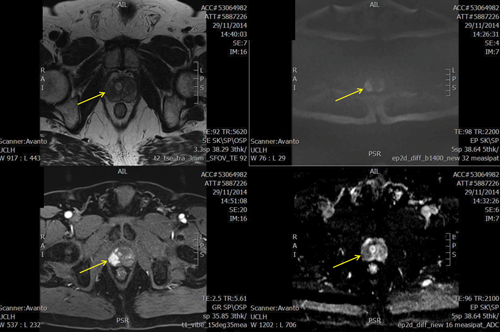
Multiparametric PROMIS MRI showing right peripheral abnormality (arrowed) scoring 5/5. TPM biopsy showed Gl 4+3. Sequences from top left T2, b-1400 diffusion weighted imaging, dynamic contrast enhanced and apparent diffusion coefficient map.
Key evidence to date
Much of this evidence has been synthesised in two recent systematic reviews [3,4] reporting sensitivities with a range of 58-96%, negative predictive values (NPVs) of 63-98% and specificities of 23-87%. The relatively wide spread for each test statistic may be explained by the inconsistencies in protocols, equipment and reporting standards between these single centre studies as well as the absence of blinding and the use of retrospective analysis.
PROMIS is notable in selecting transperineal template mapping biopsy (TPM) as the reference standard, as opposed to 12 core transrectal biopsy or whole mount pathology from radical prostatectomy, which prior publications have often favoured. Systematic biopsy of the entire prostate at 5mm intervals, though too large a burden for patients, urology and pathology departments to be employed as a routine test, produces a sampling density far greater than TRUS biopsy. Clearly whole mount pathology, with sufficiently judicious histological review, provides a detailed picture of the distribution of tumour within the gland. The disadvantage to previous trials employing this however, is that only patients with positive index tests who choose to have surgery would undergo the reference standard test, and thus no accurate calculation of test statistics can take place as proportions of both true and false negatives remain unknown.
The comparison of benign and malignant areas within the same gland is proposed in some studies [5] as a solution to this problem. Although appealing, this approach relies on the unproven and indeed unlikely assumption that benign tissue in a malignant gland occurs with the same relative frequency as do benign glands in the population, as well as it having similar morphological characteristics. Essentially, the proportions of benign and malignant tissue (as well as the distribution of cancer by grade) within the glands studied become a proxy for population disease prevalence, with a resultant skewing effect on test characteristics calculated. Both these effects stem from the selection or incorporation bias created by using whole mount specimens as a reference standard.
Trial design
The PROMIS trial was a multicentre, prospective paired cohort study evaluating the role of multiparametric MRI in men with a clinical suspicion of prostate cancer [6]. It represents level 1b evidence and reporting conforms to the STARD consensus [7]. The trial recruited 576 men from those who had not previously undergone prostate biopsy and had a raised prostate specific antigen (PSA) that was less than 15ng/ml. All participating men underwent 1.5 Tesla mp-MRI (T1W, T2W, diffusion including high b-value and ADC, dynamic gadolinium contrast) followed by a combined biopsy procedure, under general anaesthetic, incorporating standard 12 core transrectal biopsy and transperineal template mapping biopsy (the reference standard). MRI scan protocol, as well as reporting procedure, was standardised across sites with centralised training conducted. All MRI scanners and scans generated underwent independent quality control. All prostate areas were scored on a five-point Likert scale with one representing a very low and five a high likelihood of malignancy. A score of three or greater was regarded as suspicious for the purpose of the primary outcome.
The primary outcome was the detection of clinically significant disease, defined as the presence of any primary Gleason pattern four disease or a maximum cancer core length of 6mm or greater. Reporting of index and reference tests was conducted in a blinded fashion both to urologists and patients. Pathologists were also blinded and the TRUS-biopsy and TPM biopsy were reported by two separate pathologists.
Primary results
Cancer detection by the transperineal template mapping biopsy was 408/576 or 71% (95% CI 67-75) of which 40% (36-44) were clinically significant by the primary definition. The sensitivity of mpMRI for detecting these cancers was 93% (88-96) and negative predictive value 89% (83-94). By comparison, systematic TRUS biopsy demonstrated a lesser diagnostic performance with 48% sensitivity and 74% negative predictive value. MpMRI had poorer specificity and positive predictive value than TRUS-biopsy which simply indicated that a suspicious mpMRI still required a biopsy. One hundred and nineteen significant prostate cancers were missed by TRUS biopsy, the majority of which (99/119) were Gleason 3+4. Conversely 17 men had a negative MRI but significant prostate cancer detected at TPM, all of which was Gleason 3+4 disease.
Limitations
Some limitations in the trial design, though often obligate, have been rightly pointed out. The diagnostic potential of TRUS biopsy may have been limited by it taking place after transperineal mapping biopsy in all cases in PROMIS. The alternative, a randomisation of order with half of men undergoing extensive transperineal biopsy of a prostate already contaminated by rectal pathogens, was considered ethically unacceptable. Equally, the decision to set an upper prostate volume limit for the trial favoured TRUS over MRI as with decreasing sampling density one would expect TRUS to perform increasingly poorly against the volume independence of MRI. This criterion also likely reduced the number of men with no significant cancers and a high PSA due to benign enlargement.
Questions may also be reasonably directed at the choice of definition for clinically significant disease in the primary outcome and it seems true that imaging is better able to detect higher grade cancers. Two answers may be raised here. First, the definition chosen has its basis in evidence with a 0.5ml tumour volume representing the significant cut off [8] and computer modelling having shown a 6mm biopsy core to be equivalent to this size of tumour [9].
Second, analysis at differing levels of significance was conducted and the diagnostic performance of mpMRI was consistent, with sensitivity / specificity of 88% / 45% for the presence of any Gleason 7 disease and 87% / 47% for UCL significance definition 2 – grade of Gl 3+4 or and maximum cancer core length (MCCL) of at least 4mm.
The future
There is clear evidence from PROMIS and elsewhere that mpMRI should be carried out prior to first biopsy. If one accepts this premise the mind must next turn to the details of its employment. Variables abound here including quality control of mpMRI conduct and reporting, capacity, MRI sequences as well as magnet strength, biopsy route, means of targeting, and the role of zonal or mapping biopsy [10].
The authors’ institutions currently favour an MRI guided transperineal strategy, with cognitive targeting of abnormalities under local anaesthetic and the option of sedation. Zonal or mapping biopsies are not employed as standard which brings benefits to operating time and costs generally, as well as pathological burden and complication rates. In equivocal cases where imaging may be contraindicated or unclear, or where diagnostic doubt remains for some other reason template mapping biopsies provide a second tier of investigation.
Targeted only biopsies have been shown to have a diagnostic performance close to that of template mapping [11,12] and can be successfully performed under local anaesthesia and optional sedation [13], with the accompanying advantages to patient and hospital.
“The case for continuing to diagnose prostate cancer with morbid and inaccurate unguided TRUS biopsy is untenable in the light of these results.”
A significant impediment to the expansion both of pre-biopsy MRI as well as transperineal prostate biopsy in the UK and abroad has been cost. mpMRI generally costs £300-400 in the UK and can be many times that in other systems of healthcare provision, for example in the US.
By mooting mpMRI as a triage test the PROMIS findings put forward the first of several potential strategies to offset the costs of a diagnostic pathway in prostate cancer driven by imaging and transperineal biopsy. A quarter of the men in the trial might have avoided prostate biopsy, based on the primary analysis, had the results of their MRI been taken into account.
High quality health economic studies on this question are awaited but a newer diagnostic pathway offers other potential efficiencies. Further savings might potentially come from the lower need for repeat biopsies as well as the lower rate of complications and their associated healthcare costs. Treatment expenditure could be reduced due to fewer clinically insignificant cancers being detected. A pathway that includes targeted transperineal biopsy allows for the use of local anaesthetic only and finally the use of new, less expensive imaging technologies such as multiparametric ultrasound may also have a role to play.
Conclusion
The PROMIS trial represents level 1b evidence on the use of mpMRI in prostate cancer diagnosis and is the largest registered trial to date in the population at risk. The diagnostic performance of mpMRI was shown to be improved over that of standard TRUS biopsy with approximately double the sensitivity for clinically significant prostate cancer. Modelling based on the PROMIS results shows that a quarter of the trial participants might have safely avoided prostate biopsy had their MRI result been used for triage.
The adoption of a diagnostic pathway in prostate cancer based on MRI heralds the chance of improved disease detection from fewer prostate biopsies causing a much lower rate of complications. The case for continuing to diagnose prostate cancer with morbid and inaccurate unguided TRUS biopsy is untenable in the light of these results.
References
1. O’Neill J (Chair). Antimicrobial resistance: tackling a crisis for the health and wealth of nations. December 2014. Commissioned by HM Government and the Wellcome Trust.
2. Ahmed HU, El-Shater Bosaily A, Brown L, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 2017 [Epub ahead of print].
3. de Rooij M, Hamoen EH, Futterer JJ, et al. Accuracy of multiparametric MRI for prostate cancer detection: a meta-analysis. AJR Am J Roentgenol 2014;202:343-51.
4. Fütterer JJ, Briganti A, De Visschere P, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol 2015;68(6):1045-53.
5. Chamie K, Sonn GA, Finley DS, et al. The role of magnetic resonance imaging in delineating clinically significant prostate cancer. Urology 2014;83:369–75.
6. El-Shater Bosaily A, Parker C, Brown LC, et al. PROMIS – prostate MR imaging study: a paired validating cohort study evaluating the role of multi-parametric MRI in men with a clinical suspicion of prostate cancer. Contemporary Clinical Trials 2015;42:26-40.
7. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Clin Chem 2015;61:1446-52.
8. Wolters T, Roobol MJ, van Leeuwen PJ, et al. A critical analysis of the tumor volume threshold for clinically insignificant prostate cancer using a data set of a randomized screening trial. J Urol 2011;185:121–5.
9. Ahmed HU, Hu Y, Carter T, et al. Characterizing clinically significant prostate cancer using template prostate mapping biopsy. J Urol 2011;186(2):458–64.
10. Ahmed HU. The PROMIS of MRI. BJU Int 2016;118(1):7.
11. Kasivisvanathan V, et al. Transperineal magnetic resonance image targeted prostate biopsy versus transperineal template prostate biopsy in the detection of clinically significant prostate cancer. The Journal of Urology 2012;189:860–6.
12. Grey A, Hartington T, Allen C, et al. Transperineal MRI visually-targeted prostate biopsies compared to template mapping biopsy in 534 men requiring further risk stratification. J Urol 2016;195(4):e697–e698.
13. Bass EJ, Donaldson IA, Freeman A, et al. Transperineal targeted biopsy – results from a local anaesthetic service. Journal of Clinical Urology 2016;b:9-77.
TAKE HOME MESSAGE
-
MRI shows double the sensitivity for significant prostate cancer of traditional TRUS biopsy.
-
Used as a triage test MRI allows some men to safely avoid biopsy.
-
Targeted prostate biopsy may offer advantages in cost and morbidity over mapping biopsy, with a similar diagnostic performance.
Declaration of competing interests: Hashim Ahmed has received fees for speaker events, funds for attendance at conferences and proctor fees for training in HIFU from Sonacare Inc. He is also a paid proctor for Galil Medical / BTG. Sophiris, Trod Medical and Sonacare Inc provide funds for clinical trials to the institution.