Introduction
The efficient use of operating theatres is important to ensure optimum cost-benefit for the hospital and to clear waiting lists. The key elements in the efficient use of operating theatres are: effective management and good communication, trained staff, appropriate facilities, equipment, and operational layout [1]. Whilst operating rooms are simultaneously the largest cost centre and greatest source of revenue for most hospitals, studies estimate that between 10 and 40% of booked elective operations may be cancelled before surgery [2,3].
Analysis of the causes for cancellation consistently find sub-optimal utilisation of theatre time as a problem along with patients being unfit and cancellation by patients themselves [4]. In line with this, an Audit Commission report on operating theatres published in 2002 involving 70 NHS Trusts in the UK showed that on average only 73% of the planned operating hours are actually utilised [5].
“Turn-around time can be improved by having dedicated holding bays to receive preoperative patients and sufficient theatre recovery space postoperatively.”
Urological procedures make up a significant proportion of the 4.2 million surgical operations carried out each year in the UK. The specialty’s high turnover and increasing caseload, particularly in the area of endourology, make the subject of theatre utilisation and efficiency relevant in this current financial climate. The Productive Operating Theatre (TPOT) is a theatre improvement programme designed by the UK National Health Service and has been shown to improve efficiency such as start / overrun and times in urology theatres [6]. In this study, we undertook an audit in a large tertiary referral centre to record patterns of theatre usage in urology theatres and identify areas for improvement.
Materials and methods
The study was undertaken at Freeman Hospital, Newcastle Upon Tyne, UK over a 12-month period (1 June 2011 to 1 June 2012). At our unit, during this period, there were two dedicated urology theatres and a specialist endourology theatre running from 0800 to 1730 five days a week for elective surgery. Theatre session data was obtained from the local audit department and by consulting the COSMOS theatre software. This software captures the time patients are sent for, time spent in the anaesthetic room, operative and turn-around time. Data analysis was undertaken using spreadsheet software (Microsoft Excel). Specific note was made for delay in lists starting and when theatres over-ran.
Results
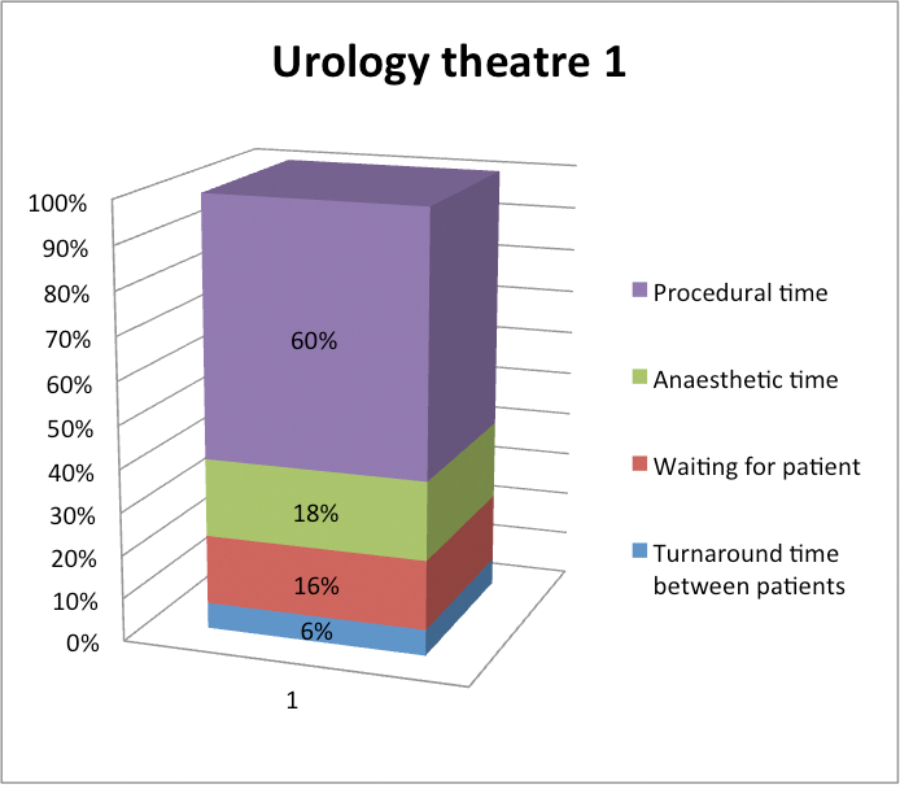
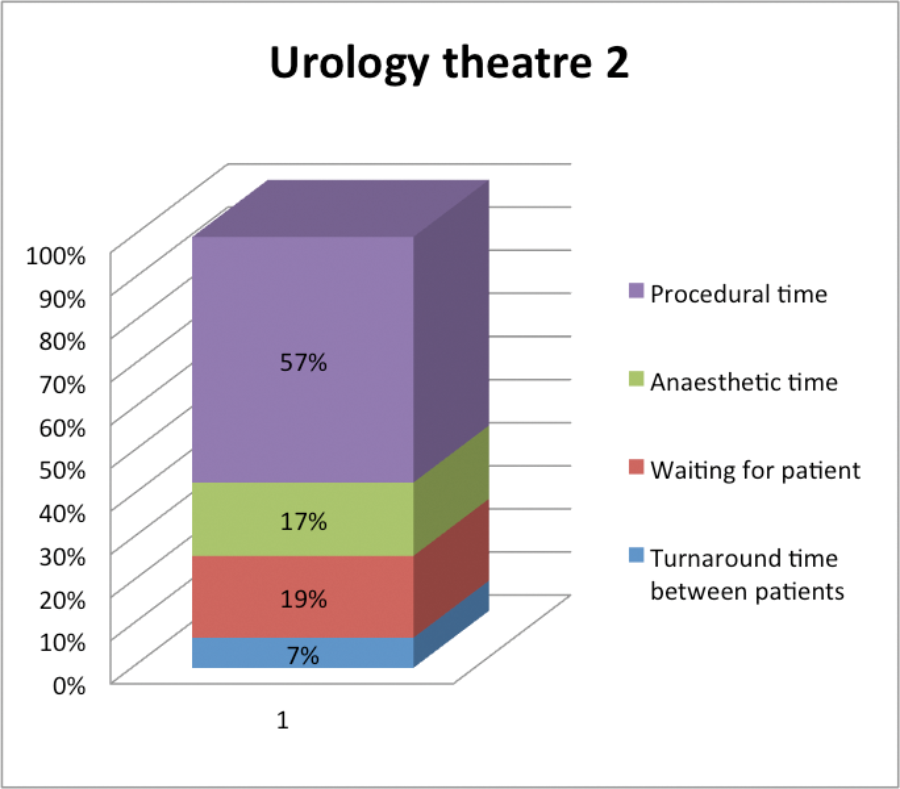
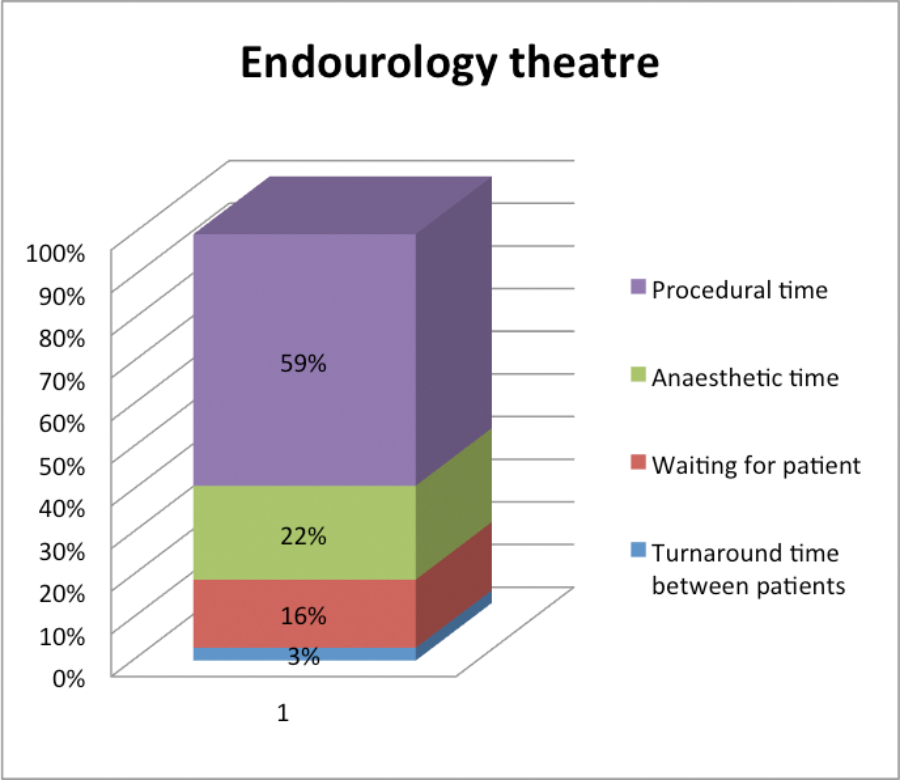
In the 12-month period, on average in all urology theatres and across 3347 cases, only 63% of the session time was spent performing surgery. Fourteen percent of time was spent in the anaesthetic room, with the remaining 23% spent between cases (turning around theatre and waiting for patients). Overall, 12% of theatre sessions had a delay in starting and there were overruns in 20%. Specifically looking at the endourology theatres, 59% of the time was spent performing surgery with 22% in the anaesthetic room and 19% between cases.
Discussion
Our study confirms that there are significant inefficiencies in theatre utilisation during elective operating lists, and about a quarter of time is wasted between operations. Considerable operating theatre time is wasted while patients are transferred to and from the operating theatre resulting in both anaesthetists and surgeons having to wait between patients in a high proportion of cases. Inefficient theatre time utilisation is in fact a problem worldwide, with several studies having been carried out in North America and Australia [7]. A number of measures have been discussed to improve efficiency. Pre-admission anaesthetic assessment clinics have been shown to reduce the number of theatre cancellations and reduce delay in theatres whilst patients wait for tests on the day of surgery [8]. Patients should be sent for early enough to avoid the anaesthetist having to wait to be able to start the anaesthetic [9]. In addition, on the anaesthetic side, overlapping reversal with induction of the next case has been shown to improve theatre efficiency by reducing turnover time and increasing operating room occupancy but this often requires two anaesthetists to achieve [10]. Turn-around time can be improved by having dedicated holding bays to receive preoperative patients and sufficient theatre recovery space postoperatively.
Overall we have shown that the majority of non-operating time is spent in anaesthetics or turn-around. Nearly a quarter of time is spent between cases (non surgical / anaesthetic time). Streamlining the patient pathway and reducing turn-around time may significantly improve theatre throughput.
References
1. The Association of Anaesthetists of Great Britain and Ireland. Theatre efficiency – safety, quality of care and optimal use of resources. London, UK; 2013.
2. Denton B, Viapiano J, Vogl A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag Sci 2007;10:13–24.
3. Schofield WN, Rubin G, Piza M, et al. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust 2005;182:612–15.
4. Rai M, Pandit JJ. Day of surgery cancellations after nurse-led pre-assessment in an elective surgical centre: the first 2 years. Anaesthesia 2003;58:692–9.
5. Operating Theatres: Review of National Findings – Audit Commission. London, UK; 2003.
6. Ahmed K, Khan N, Anderson D, et al. Introducing the productive operating theatre programme in urology theatre suites. Urol Int 2013;90(4):417-21.
7. Franklin D, Traub RD. How to schedule elective surgical cases into specific operating rooms to maximize the efficiency of use of operating room time. Economics and Health Systems Research. Anesth Analg 2002;94:933–42.
8. Emanuel A, Macpherseon R. The anaesthetic pre-admission clinic is effective in minimising surgical cancellation rates. Anaesth Intensive Care 2013;41(1):90-4.
9. Sahaly P, Pinjanily A, Al-Shabibily N, et al. Why we are wasting time in the operating theatre? Int J Health Plann Mgmt 2009;24:225–32.
10. Sokolovic E, Biro P, Wyss P, et al. Impact of the reduction of anaesthesia turnover time on operating room efficiency. Eur J Anaesthesiol 2002;19:560–3.
Declaration of competing interests: None declared.