Urethral diverticula are an uncommon finding on imaging. They are focal outpouchings of the urethra into the periurethral / urethrovaginal space, occurring more frequently in females (up to 6% of women) [1]. These diverticula are becoming more prevalent in clinical practice, in part due to developments and advances in imaging techniques leading to improved sensitivity and specificity.
As female urethral diverticula becomes more prevalent in clinical practice, radiologists and clinicians should be familiar with imaging features and optimal techniques. We present a review of common diagnostic techniques and imaging recommendations.
Aetiology and pathology
They are most prevalent between the third and sixth decades, and are multiple in up to one third of female patients. It is thought that the acquired diverticula result from a rupture / dilatation of an infected or obstructed periurethral gland [1-4]. The diverticula may also form after disruption of the periurethral fascia during surgery (such as obstetric, vaginal or urtheral surgery) [2,3]. Congenital urethral diverticula have also been reported although it should be noted that these are extremely rare [2]. Despite many diverticula being asymptomatic and discovered incidentally these phenomena can cause symptoms such as recurrent urinary tract infections, pain and incontinence [1,2].
Symptoms often arise due to chronic inflammation which can lead to complications such as stones (10% of patients [4]) or more serious sequelae such as intra diverticular neoplasia [1]. Adenocarcinoma is the most frequently diagnosed tumour in female urethral diverticula; as the diverticula can be of quite inconspicuous presentation, a neoplastic diagnosis can often be delayed [1,3]. The most common clinical presentation are the three D’s; Dysuria, Postvoid Dribbling and Dyspareunia [3]. Classic findings on examination are a tender cystic lesion in the anterior vaginal wall in half of patients with urethral diverticulum [3].
Urethral diverticula can occur as single or multiple entities [3]. They can be wide or narrow necked, unilocular or multicompartmental [3]. So called ‘saddle diverticula surround the urethra. The diverticula are usually located on the posterolaterally wall (at the three to nine o’clock position) [1,2,3] within the middle third of the urethra [2]. Potential differential diagnoses to consider are: Gartner duct cyst, Müllerian duct cyst, epithelial inclusion cyst and urethral tumour.
Fluoroscopic imaging
Voiding cystourethrography was traditionally used to investigate urethral diverticula due to its high sensitivity and specificity. The bladder is catheterised with a 14-French Foley catheter and filled with contrast agent [2,4]. Anteroposterior and oblique images are obtained during filling as well as during and after voiding [2]. It has the advantage of being technically easy and relatively simple to perform. Unfortunately, fluoroscopy is rather insensitive for those diverticula with obstructed orifices. It also involves ionising radiation and requires catheterisation, which can be uncomfortable for the patient. It can only provide intraluminal information.
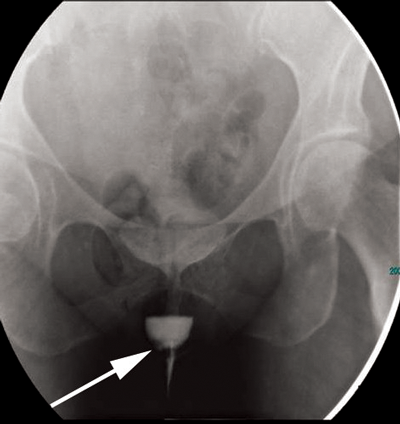
Figure 1a: Erect image taken from a voiding cystourethrogram
showing a urethral diverticulum with a filling defect (arrow).

Figure 1b: Supine image showing urethral diverticulum.
Figure 1 shows a well defined rounded area filled with contrast that remains after bladder emptying. Note the small filling defect on the right side of the diverticulum (arrow), in keeping with a tumour. Double-balloon urethrography can also be used, despite having a greater sensitivity than voiding cystourethrography [2] it is more technically difficult. More recently, cross-sectional imaging has become more popular due to the greater need to delineate the diverticula and investigate malignant transformation [4].
CT imaging
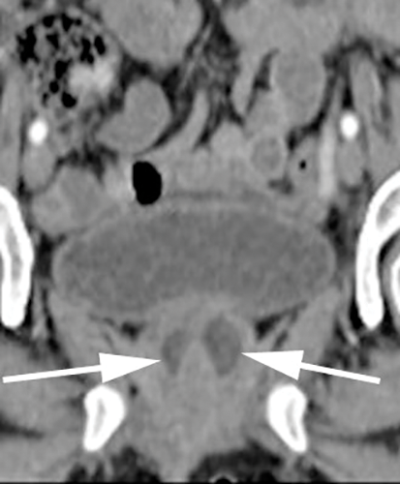
With CT imaging, diverticula appear as hypointense periurethral cystic lesions, with wall thickening and enhancement [2]. They are usually identified at the level of the pubic symphysis (Figure 2). Using voiding CT urethrography, the diverticula may opacify upon post voiding imaging [2]. To a limited extent CT can characterise urethral abnormalities [2]. It can also identify associated complicating urethral calculi and gas within the diverticula and allows for regional staging of any urethral neoplasms [2]. The disadvantage of CT is the use of ionising radiation and it is rather insensitive for small diverticula [4]. Figure 2 demonstrates a urethral diverticulum on CT imaging. Note the low attenuation, thick walled cystic density structure around the urethra measuring 2.7 x 2.0cm.
Figure 2a: Axial CT.
Figure 2b: Coronal CT showing urethral diverticulum (arrows).
MR imaging
MR imaging has high sensitivity and specificity for urethral diverticula. MR is more sensitive than fluoroscopy and does not involve any ionising radiation. It is ideal for detecting narrow-neck diverticula and has the added benefit of being able to detect other abnormalities in adjacent structures that could be causing symptoms [2]. MRI with a torso phased array coil can help to depict particularly small diverticula [2,3]. However this does have the disadvantages of increased cost, reduced access and long image acquisition times.

Figure 3a: Axial T1 fat sat pre gad – the urethral diverticulum cannot be seen.
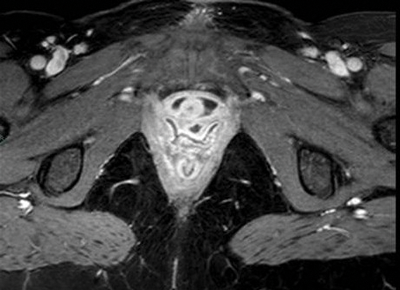
Figure 3b: Axial T1 fat sat post gad showing low signal diverticulum
but no enhancement to suggest a tumour.

Figure 3c: Axial T2 fat sat shows debris within the divertiuclum.
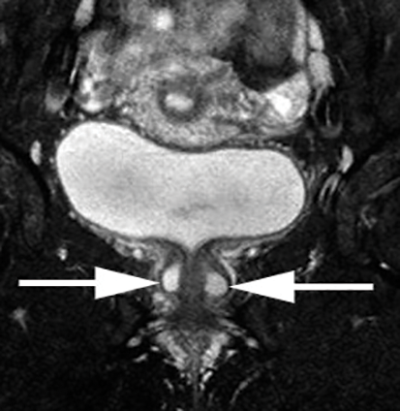
Figure 3d: Coronal T2 SPIR. Images show the saddle diverticulum encasing the urethra.
Uretheral diverticula are usually characterised as a hyperintense periurethral cystic lesion on T2 weighted imaging (Figure 3). They are hypointense on T1 weighted sequences. The diverticula neck may or may not be visualised. The addition of a gadolinium-based contrast agent can help in differentiating diagnoses. Irregular enhancement or mass-like components within a diverticulum may suggest infection or malignancy [2]. Once identified, radiologists should report the size and number of urethral diverticula, as well as the presence of any complications. The position of the diverticular neck if visible should also be commented upon to aid possible surgical intervention [2].
Suggested MR imaging protocol [2,4]
- T1 weighted sequences pre and post administration of IV gadolinium based contrast material.
- Axial, coronal and sagittal fat-saturated fast spin T2 weighted sequences.
These are best performed with pelvic phased-array coils. Endovaginal or endorectal coils provide greater higher resolution details and help to appreciate the orientation of the diverticula orifice [2], however these are not routinely used due to patient discomfort [2,3,4].
Conclusion
Thorough knowledge of the available imaging modalities used to investigate urethral diverticula is important for radiologists in order to provide the best imaging technique for this increasingly prevalent condition. MR imaging is the recommended imaging modality of choice but urethral diverticula can also be seen on screening. The advantage of MR is its ability to delineate the diverticulum, provide details of associated complications and avoidance of ionising radiation. The addition of gadolinium-based contrast is also recommended to aid in the detection of inflammation, infection and potential malignant transformation.
References
1. Prasad SR, Menias CO, Narra VR, et al. Cross-sectional imaging of the female urethra: technique and results. Radiographics 2005;25:749-61.
2. Chou CP, Levenson RB, Elsayes K, et al. Imaging of female urethral diverticulum: an update. Radiographics 2008;28:1917-30.
3. Kawashima A, Sandler CM, Wasserman NF, et al. Imaging of urethral disease: a pictorial review. Radiographics 2004;24:S195-S216.
4. www.radiopaedia.org/
articles/urethral-diverticulum