Introduction
The identification of specific risk factors associated with erectile dysfunction (ED) allows patients with mild or moderate ED to undergo a series of lifestyle changes, which may provide enough improvement in the erectile function to avoid pharmacotherapies. Cessation of smoking, weight loss and regular exercise are associated with an improvement in erectile function, as well as improving endothelial function. Bicycle riding for more than three hours per week is also a risk factor possibly due to compression of the pudendal nerve and arteries.
Treatment options for ED
Psychosexual counselling
Patients diagnosed with purely psychogenic ED should have a programme of psychosexual counselling incorporated in the management plan. This does not stop them from undergoing treatment with pharmacological agents. Invariably most patients will have a combination of psychogenic as well as organic factors and therefore psychosexual counselling should be offered to all patients undergoing treatment for ED.
Most psychological approaches use the following:
- Cognitive behavioural therapy (CBT)
- Behavioural model using techniques of sensate focusing
- Couple counselling
- Group therapy.
Generally between 8 and 20 treatment sessions where negative experiences and underlying conflicts related to sexual behaviour are explored, are required. Several phases are then introduced which are aimed at reducing the pressure and inhibition related to performance and then gradually developed until successful coitus is achieved.
Over the counter and herbal remedies
Although a number of herbal remedies have been used in parts of Asia and Africa as well as in some regions of Europe and North America, there are only three herbal remedies which have published data from studies in humans – Panax ginseng, Butea superba and Yohimbine.
Pharmacological treatments for ED
Pharmacotherapies include oral agents, intracavernosal injection (papaverine, phentolamine, prostaglandin E1, VIP) and transurethral vasoactive agents (prostaglandin E1). Although a number of newer phosphodiesterase type 5 (PDE-5) inhibitors are available globally, sildenafil (ViagraTM), vardenafil (LevitraTM) and tadalafil (CialisTM) are the commonest prescribed PDE-5 inhibitors in the UK. Tadalafil at the once daily dose of 5mg is also the only PDE-5 inhibitor currently licensed for the treatment of ED and lower urinary tract symptoms / benign prostatic hyperplasia (LUTS / BPH).
“Invariably most patients will have a combination of psychogenic as well as organic factors and therefore psychosexual counselling should be offered to all patients undergoing treatment for ED.”
Food intake causes no delay or reduction in tadalafil absorption, whereas it is known to reduce and delay absorption of sildenafil. The mean half-lives (t1/2) of sildenafil and vardenafil are three to four hours, whereas that of tadalafil is approximately 17.5 hours. Results from clinical trials suggest that all three currently available PDE-5 inhibitors are effective in a wide range of patient groups. Treatment with vardenafil at a dose of 20mg produced an improvement in the ability to achieve an erection in 80% of ED patients. In a study using sildenafil (100mg dose) 84% of ED patients were successfully treated. Treatment with tadalafil 20mg produced an improvement in the ability to achieve an erection in 81% of ED patients. The most common side-effects seen with sildenafil include headache, flushing, dyspepsia, and rhinitis. The adverse effects with tadalafil and vardenafil are similar to sildenafil, however tadalafil is associated with a higher incidence of back pain (4-9%) and myalgia.
Table 1: Oral agents for the treatment of male erectile dysfunction.
Oral Treatments: Sildenafil citrate (ViagraTM)
Dose: 50-100mg
Oral Treatments: Tadalafil (CialisTM)
Dose: 5mg daily or 10-20mg on demand
Oral Treatments: Vardenafil hydrochloride (LevitraTM)
Dose: 10-20mg
The synthetic PGE1 analogue alprostadil can be administered as a second-line therapy in patients who fail to respond to PDE-5 inhibitors or have a specific contraindication to treatment with oral agents. PGE1 mediates corpus cavernosum smooth muscle relaxation by increasing the intracellular concentrations of the second messenger cAMP. Alprostadil is either used as an intracavernosal injection (dose 2.5-20μg, 80% response rate) or intraurethral instillation of a small pellet in the form of MUSE® (dose 250–1,000μg, 65% response rate).
Testosterone replacement therapy
Although androgens are known to be involved in both the central and peripheral pathways mediating penile erection, the role of testosterone replacement is still uncertain in men with late onset hypogonadism. Testosterone is required for NOS expression in the corpus cavernosum and also for the maintenance of the neural pathway. Although controversial, testosterone supplementation has been reported as a therapeutic option in patients with erectile dysfunction who are non-responders to PDE-5 inhibitors and have been diagnosed with a low serum testosterone level. However, testosterone replacement as a first-line treatment option for erectile dysfunction in men with late onset hypogonadism or those with normal serum testosterone levels is not recommended.
Figure 1: An example of a vacuum erection device.
Vacuum erection devices
These devices (Figure 1) are useful in patients with psychogenic or organic erectile dysfunction and can be used alone or in combination with other therapies. An external cylinder is used to create a negative pressure and the resulting penile tumescence is maintained by means of a constriction ring placed at the base of the penis. The reported patient satisfaction rate is 50–70%.
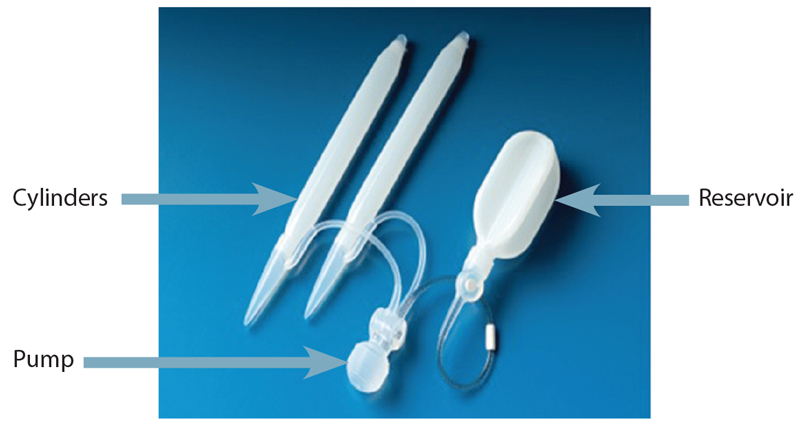
Figure 2: The recently launched Titan Touch 3-piece inflatable penile prosthesis. The new pump design allows the deflate button to be pressed once followed by instantaneous deflation of the cylinders. Image courtesy of Coloplast.
Penile prosthesis surgery
Patients with severe erectile dysfunction which is refractory to pharmacological treatment can be offered a penile prosthesis as an end-stage surgical solution. Two main subtypes of prosthesis are available: malleable (or semi-rigid) and inflatable. The malleable devices have the advantages of decreased mechanical breakdown, easier placement and lower cost. Inflatable devices are available as two-piece (Ambicor®, American Medical Systems) or three-piece devices (AMS 700CX® or Coloplast Titan®, Titan Zero Degree®, Titan Touch®). The two- and three-piece devices have a pump placed in the scrotum that controls the inflation and deflation of the device and therefore requires an element of patient dexterity. With the three-piece prosthesis a reservoir is placed in the retropubic space and the transmission of fluid to the cylinders from the reservoir is controlled by a lock out valve. Inflatable prostheses continue to undergo modifications with better tactile pumps and modifications to the reservoir to allow easier placement. The complications include infection rates of up to 2–3% and re-operation rates for mechanical failure of 15% by 10 years. The overall satisfaction rates have been reported as over 90% from both patients and partners.
Penile revascularisation surgery
Vascular causes of erectile dysfunction include arterial insufficiency of the internal iliac artery and its branches or veno-occlusive dysfunction. The high prevalence of internal pudendal artery stenoses among men with angiographically evident coronary artery disease has led to interventionalists performing balloon angioplasty or placement of stents in the internal iliac and internal pudendal arteries. Although erectile dysfunction secondary to traumatic injuries to the internal pudendal arteries is amenable to microsurgical revascularisation by anastomosing the inferior epigastric artery to the deep doral vein of the penis, the use of stenting and angioplasty provides another option for stenotic blood vessels. Recently, low intensity shock wave treatment has been used in small clinical trials to induce neovascularisation in the corpus cavernosum. Larger multicentre trials are awaited.
Future treatment options
Despite recent advances in the management of ED, there are still a significant number of ED patients who do not respond to currently available treatment modalities, especially those patients with diabetes or neurogenic injury following pelvic surgery, for whom new treatment alternatives are in great demand. As a result of this, there has been renewed interest in the possibility of gene therapy in the management of ED. Putative targets for gene therapy may include nitric oxide synthase, growth factors and voltage gated channels. However, there are safety concerns that have delayed the clinical translation of gene therapy to human patients. However, it is hoped that the long-term safety of both viral and non-viral gene therapy can be established in the near future before large-scale human studies are considered.
Part 1 of this topic is available here.