We present the case of an 83-year-old female who underwent right radical nephrectomy for renal cell carcinoma (RCC). Despite negative surgical margins, the patient presented with a skull metastasis six years post radical nephrectomy. This case highlights the importance of vigilant follow-up and consideration of metastatic disease in patients with a history of renal cell carcinoma.
RCC accounts for approximately 2–3% of all adult malignancies and is known for its potential to metastasise to distant organs [1]. While radical nephrectomy remains the standard treatment for localised RCC, the management of metastatic disease poses significant challenges, particularly when metastasis occurs in uncommon sites such as the skull. Metastasis to the skull occurs in approximately 1–2% of RCC cases and presents unique diagnostic and therapeutic dilemmas [2].

Figure 1: Initial CT of patient.

Figure 2: 2.7cm abnormal, heterogeneous mass seen anteriorly in the upper pole of right kidney, highly suspicious of RCC. This was not seen previously.

Figure 3: CT CAP, status post right radical nephrectomy. Left simple lower pole renal cyst.
Case report
An 83-year-old woman was referred to our urology multidisciplinary team (MDT) for an enlarging scalp lesion for three to four months, otherwise not causing any neurological symptoms. Her background consisted of left upper lobectomy pT2aN1 and adjuvant chemotherapy (2016), right radical nephrectomy for a centrally located 2.4cm grade 2 clear cell RCC, International Society of Urologic Pathologists (ISUP) Grade 2, pT1a, clear surgical margins, Leibovich 0 (November 2019), right upper lobectomy for adenocarcinoma pT2b N0 M0 (March 2021), hypertension, cerebral vascular accident (CVA), and chronic kidney disease (CKD) stage 3. Between 2011 and 2018 she was also treated for right renal tract stones with percutaneous nephrostomy (PCN) and antegrade JJ stent. She was on antihypertensives, a statin and clopidogrel. A long-time smoker, she lived alone, mobilised with a Zimmer frame, was assessed as patient performance status (PS) stage 3, and was clinically frail.
Blood work reported estimated glomerular filtration rate (eGFR) of 26, creatinine 161, and normal liver functions tests (LFTs). The CT at initial presentation with renal cancer and the recent contrast CT chest, abdomen and pelvis are shown in Figures 1–3. MRI of the skull reported a 3.3x2.3cm soft tissue heterogeneous lesion involving the parietal bone and invading the dura (Figure 4). Ultrasound-guided scalp biopsy showed infiltration of fibrous tissue by sheets of epithelioid tumour cells with abundant clear cytoplasm and intervening prominent blood vessels. The tumour cells expressed RCC, CD10 and PAX 8. They did not express CK7, CK20, TTF-1, Gata3 and WT-1. The conclusion was metastatic RCC.
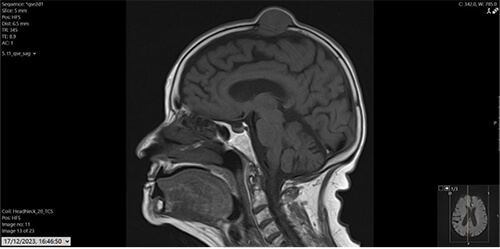
Figure 4: A soft tissue lesion with heterogeneous signal intensity is seen in the parietal bone measuring 3.3x2.3cm in size which shows dural invasion. Both CP angles are normal.
The neuro-oncology MDT determined that the lesion was centred in the bone in the proximity of the superior sagittal sinus but not in contact with the brain but is keeping with metastasis. The management plan was for the local oncology team to review her for consideration for radiotherapy, and that she would not be suitable for neurosurgical intervention.
Discussion
Skull metastasis from renal cancer is uncommon, occurring in less than 1% of cases. The interval between nephrectomy and presentation of skull metastasis varies widely, ranging from months to several years. The pathogenesis of RCC metastasis involves hematogenous spread, with bone being one of the favoured sites due to its rich vascularity.
About 50 different sites are described as potential metastatic locations for renal tumours, including skull metastasis which is a rare location [3]. RCC exhibits a pronounced inclination to spread, with 25% of patients showing distant metastasis at initial presentation, while an additional 50% experience metastasis during subsequent follow-up [4,5]. There are head and neck metastases from RCC in up to 8–15% of cases [4,6].
Renal tumours commonly manifest with bone metastases, yet instances of metastases in the skull are rare. In a review of 1668 RCC patients by Forbes [7], only five cases exhibited skull metastasis. This occurrence typically presents as a swelling on the skull. In certain instances, if the metastasis exerts pressure on the brain, it may manifest with symptoms of intracranial hypertension or focal neurological deficits, particularly if located near critical cerebral areas [8].
The established protocol for managing metastatic RCC involves surgically removing the tumour in the skull and performing a radical nephrectomy [9]. It has been observed that metastatic deposits can sometimes vanish after removing the primary tumour [10], indicating complete spontaneous regression of pulmonary and bone metastases likely triggered by immunological responses [11]. However, it is important to note that this phenomenon hasn't been definitively confirmed for head and neck metastases from RCC [9].
The presence of metastatic RCC initially indicates an extensively spread disease, typically resulting in a median survival of one year [12]. Additionally, the simultaneous detection of solitary metastasis along with the primary tumour is regarded as an unfavourable characteristic [13].
Nevertheless, in this specific subgroup of patients, aggressive surgical intervention can yield optimal palliative outcomes and may even lead to long-term survival in certain instances [14]. Targeted therapies, such as tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors, have shown efficacy in controlling metastatic RCC; however, their role specifically in skull metastasis is not well-defined.
Conclusion
While occurrences of metastases in the head and neck region are rare, it's important to consider them when assessing any atypical subcutaneous mass in this area. Given the unpredictable timing and clinical characteristics of metastases, a thorough evaluation of any unusual lesion is warranted, regardless of the patient's cancer history. Even unconventional sites like the calvaria should prompt consideration of RCC. Managing metastatic RCC poses challenges, as determining the most effective treatment regimen to achieve long-lasting responses without significant toxicity remains undefined.
References
1. Gupta K, Miller JD, Li JZ, et al. Russell MW, Charbonneau C. Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): a literature review. Cancer Treat Rev 2008;34(3):193–205.
2. Nieder C, Marienhagen K, Astner ST, et al. Prognostic scores in brain metastases from renal cell carcinoma. BMC Cancer 2009;9:106.
3. Wahner-Roedler DL, Sebo TJ. Renal cell carcinoma: diagnosis based on metastatic manifestations. Mayo Clin Proc 1997;72:935–41.
4. Ogunyemi O, Rojas A, Hematpour K, et al. Metastasis of genitourinary tumors to the head and neck region. Eur Arch Otorhinolaryngol 2010;267:273–9.
5. Schwab B, Lee W. Bilateral renal cell carcinoma metastasis in the oral cavity. Am J Otolaryngol 2012;33:154–5.
6. Ishak AI, Pauzi SH, Masir N, Goh B. Multiple metastatic deposits in the head and neck region from a renal cell carcinoma. Malay J Med Sci 2010;17:71–4.
7. Forbes GS, McLeod RA, Hattery RR. Radiographic manifestations of bone metastases from renal carcinoma. Am J Roentgenol 1977;129:61–6.
8. Koutnouyan HA, Rumore GJ, Kahn JM. Skull metastasis from renal cell carcinoma: case report and literature review. Ann Otol Rhinol Laryngol 1998;107(7):598–602.
9. Yeh HC, Yang SF, Ke HL, et al. Renal cell carcinoma presenting with skull metastasis: a case report and literature review. Kaohsiung J Med Sci 2007;23:475–9.
10. Hrouda D, Muir GH, Dalgleish AG. The role of immunotherapy for urological tumours. Br J Urol 1997;30:7–16.
11. Simo R, Sykes AJ, Hargreaves SP. Metastatic renal cell carcinoma to the nose and paranasal sinuses. Head Neck 2000;22:722–7.
12. Fyfe G, Fisher RI, Rosenberg SA. Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J Clin Oncol 1995;13(3):688–96.
13. O’Dea MJ, Zincke H, Utz DC. The treatment of renal cell carcinoma with solitary metastasis. J Urol 1978;120(5):540–2.
14. Navarro F, Vicente J, Villanueva MJ. Metastatic renal cell carcinoma to the head and neck area. Tumors 2000;86:88–90.