Case 1
A 65-year-old woman presents with an 18-month history of “recurrent urinary tract infections” (rUTI). She is otherwise fit and well with no underlying medical problems and no lower urinary tract symptoms.
- What is the definition of a UTI and what is the meaning of ‘recurrent’ UTI?
- What risk factors are commonly associated with rUTI in post-menopausal women?
- A urine dipstick is often the first port of call in diagnosing a UTI. What findings on a urine dipstick suggest infection and how reliable are they?
- What non antibiotic alternatives can be used to prevent rUTI?
Case 2
A 51-year-old woman presents with increased daytime frequency, urgency and urgency incontinence. She has no significant past medical history and has previously had two children via normal vaginal delivery. She does not report any stress urinary incontinence and wears two pads per day.
- Having trialled conservative measures her symptoms are still bothersome and she is prescribed 5mg solifenacin by her GP. What are the common side-effects and contra-indications to anti-cholinergic use?
- If anti-cholinergic therapy is ineffective (or contra-indicated) which other medication can be trialled?
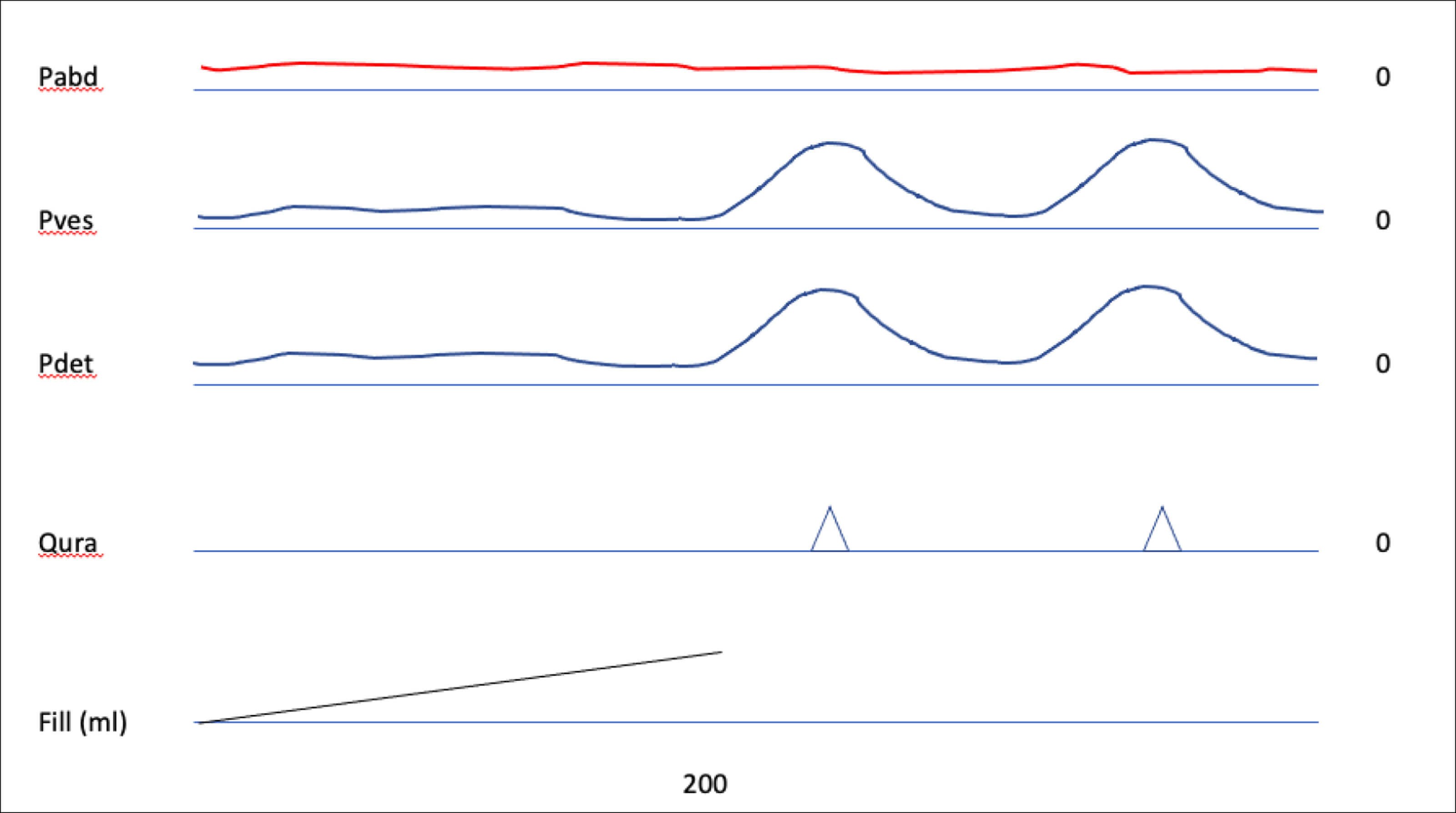
- What does the below urodynamics trace show and what surgical options are available to manage this?
- What is the efficacy of intravesical botulinum toxin injections and what risks should be included on the consent form?
Female and functional: answers
Case 1
- A UTI is the inflammatory response of the urothelium to micro-organism invasion (most commonly bacteria). Recurrent infections can be defined as ≥ two in six months or ≥ three in one year. These may further be sub-divided into persistent (infection with the same organism) or re-infection (different organism).
- Risk factors in young and pre-menopausal women are typically related to sexual intercourse and include the use of spermicide or a new sexual partner, with other risk factors including a mother with a history of UTIs, infections during childhood and blood group antigen secretory status.
In post-menopausal and elderly women recurrent infections are typically attributed to poor bladder emptying and atrophic vaginitis. Further commonly cited risk factors include history of UTI before menopause, urinary incontinence, cystocele, blood group antigen secretory status, urine catheterisation and functional status deterioration in elderly, institutionalised women [1]. - Leucocytes and nitrites suggest infection. Leucocytes (pyuria) have a sensitivity of 75-95% but low specificity. Alternatively, nitrites have high specificity but low sensitivity. In essence if a patient has a nitrite positive dip, they are likely to have an infection, but false negatives are common.
- Topical oestrogen is thought to promote vaginal lactobacilli and reduce colonisation by uropathogens such as E.coli. Application has been shown to be superior to placebo and hence vaginal oestrogen replacement is strongly recommended by the European Association of Urology (EAU) [1,2]. D-mannose is a monosaccharide which binds to the type 1 pili of E.coli preventing bacterial adhesion to the bladder wall.
D-mannose has been shown to be similar in efficacy to prophylactic antibiotics, but further data is required [2]. Patients are required to purchase D-mannose at their own expense.
Methanamine hippurate (Hiprex™) is hydrolysed in urine to form formaldehyde, which is bacteriostatic. It works best in an acidic environment and may therefore be given with additional vitamin C. The recent ALTAR study confirmed non inferiority to antibiotic prophylaxis and Hiprex may reduce the rate of antibiotic resistance in suitable patients [1,3].
Other non-antibiotic options include immunoactive prophylaxis and intra-vesical installations (such as iAluRil®).
Case 2
- Solifenacin is a competitive muscarinic receptor antagonist, it is largely selective for the functionally important M3 receptor. Common side-effects include dry mouth, constipation and blurred vision. Antimuscarinics should be avoided in those with acute angle closure glaucoma, myasthenia gravis, a significant post void residual volume and gastrointestinal pathology such as ulcerative colitis and intestinal atony. An association with dementia has been reported and therefore it should be used with caution in the elderly or at-risk patients who may also be considered for alternatives such as trospium which does not cross the blood brain barrier [4].
- The B3 agonist mirabegron can be used. Contraindications include severe uncontrolled hypertension.
- Idiopathic detrusor overactivity and detrusor overactivity incontinence. Surgical management includes intravesical botulinum toxin A (Botox®) injections or sacral neuromodulation (SNM). In extreme cases clam augmentation cystoplasty or urinary diversion may be performed.
- The efficacy is approximately 50-75% and patients should be warned they will need repeat injections, on average, every 6-12 months. Commonly occurring after-effects include dysuria and mild haematuria. Less common side-effects include infection, the need to perform self-catheterisation (which should be taught to all patients prior to the procedure), an allergic reaction, flu-like symptoms and transitory lower limb weakness.
References
1. EAU Guidelines on Urological Infections. Presented at the EAU Annual Congress Amsterdam, The Netherlands 2022.
2. Sihra N, Goodman A, Zakri R, et al. Nonantibiotic prevention and management of recurrent urinary tract infection. Nat Rev Urol 2018;15(12):750-76.
3. Harding C, Mossop H, Homer T, et al. Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women: multicentre, open label, randomised, non-inferiority trial. BMJ 2022;376:e068229.
4. Gray SL, Anderson ML, Dublin S, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med 2015;175(3):401-7.