See also Part 2 and Part 3.
Case 1
A 59-year-old man presented with right loin pain. His GP arranged for him to have an intravenous urogram (IVU) and subsequent CT urogram performed.


- What is the likely diagnosis? What are the classical features seen on imaging?
- What is the likely pathology?
- What treatment options are available to treat his kidney?
- What are the surgical principles for ureterolysis?
- What is the blood supply to the omentum?
Case 2
A 55 year-old female presented with persistent E.coli urinary tract infections (UTI). She underwent cystoscopy and the following lesion was identified.
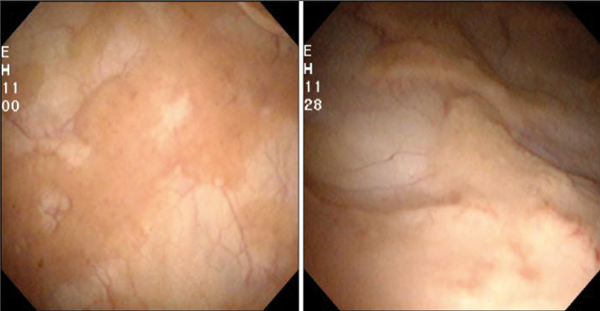
Figure 1.
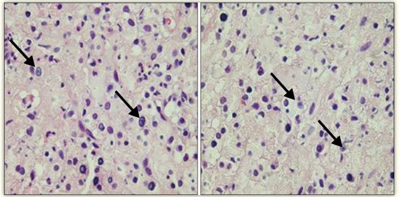
Figure 2.
(Images reproduced from Korean J Urogenit Tract Infect Inflamm 2013;8(2):125-8.
Copyright © 2013, Korean Association of Urogenital Tract Infection and Inflammation.)
- Describe the lesion seen on figure 1. What is the likely cause?
- How would you confirm the diagnosis?
- What pathognomonic histological feature is seen in figure 2?
- What parts of the urinary tract can be affected?
Case 3
NIH Classification of Prostatitis Syndromes
Category Definition
Type 1 A
Type 2 B
Type 3a C
Type 3b D
Type 4 E
- Define terms A, B, C, D and E?
- What specific groups of symptoms may patients complain of?
- What is the Mears Stamey 4 glass test?
- What is the NIH definition of prostatitis for the following patients based on the Mears-Stamey test:
A. VB1+2 negative, EPS positive for WBC and VB4 positive for WBC.
B. VB1+2 negative, EPS clear but VB4 positive for bacteria.
C. VB1 and VB2 positive for bacteria.
Answers
Case 1
-
Retroperitoneal fibrosis. Proximal hydronephroureterosis, tapering of the ureteric lumen and medial deviation of the ureter.
-
Idiopathic: Commonest (70%).
Inflammatory: Pancreatitis, perianeurysmal RPF, aortitis.
Drug induced: Hydralazine, beta blockers, methyldopa, haloperidol, phenacetin.
Malignant: Lymphoma, germ cell tumours, metastatic lymph node mass, sarcoma.
Iatrogenic: Radiotherapy.
Trauma.
-
Medical: Steroid treatment, +/- tamoxifen, azathioprine.
Surgical: Ureteric stent, nephrostomy tube, ureterolysis.
Alternative treatments include transureteroureterostomy, ileal interposition or autotransplantation.
-
Often bilateral treatment needed, despite unilateral disease. Ureteric stent insertion, start dissection from normal tissue to diseased tissue, avoid damage to ureteric adventitia, biopsy fibrotic mass, protect ureters with omental wrap.
-
Right and left gastro-epiploic arteries (via gastro-duodenal and splenic artery respectively, originating from the Coeliac axis, T12).
Case 2
-
Soft, raised, pale yellow plaques on the bladder mucosa. Malakoplakia – associated with defective macrophage function.
-
Resect the lesion for histology via TURBT.
-
Michaelis-Gutmann bodies. Represent remnants of phagosomes mineralised by iron and calcium deposition.
-
Commonly bladder, but it can affect the kidney, ureter and prostate.
Case 3
-
A: Acute bacterial prostatitis; B: chronic bacterial prostatitis; C: chronic pelvic pain syndrome – inflammatory; D: chronic pelvic pain syndrome – non-inflammatory; E: Asymptomatic.
-
‘UPOINT’ symptoms: Urinary; Psychosocial; Organ specific: bladder / prostate; Infection; Neurological; Tenderness of muscles; Sexual.
-
Specific set of urine samples taken at defined periods to aid in the diagnosis of prostatic syndromes. Urine samples sent for culture and WBC measurements, labelled VB1, VB2, EPS, VB3. VB1: 1st 10ml voided, VB2 is MSU, EPS represents expressed prostatic secretions (post DRE) and VB4 5-10ml post EPS urine sample.
-
A. Type IIIa B. Type II C. Type I (do not perform EPS in these patients).




