See also Part 1 and Part 3.
Case 1
A 43-year-old lady presented to the urologist with a history of pain during bladder filling and associated frequency / urgency. She underwent standard microbiological and radiological investigations that are normal. She proceeded to a cystoscopy + bladder distension to investigate her pain.
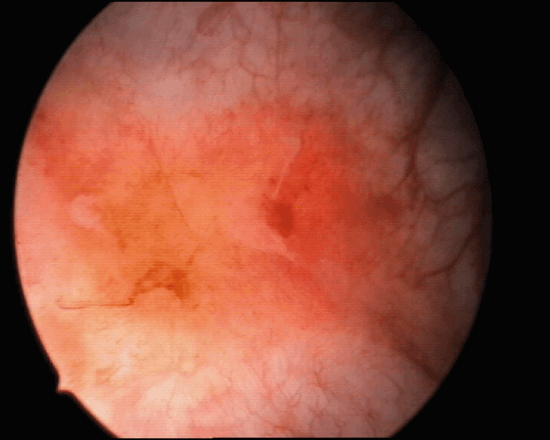
Figure 1.
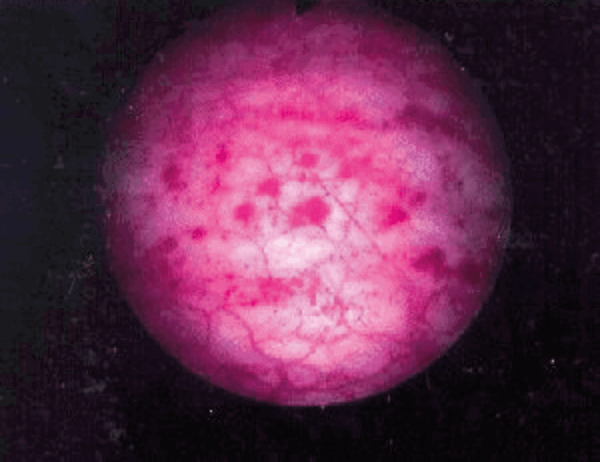
Figure 2.
- What are the appearances seen in Figure 1 and 2? What is the likely diagnosis at this stage?
- List other conditions that must be excluded before a diagnosis can be established.
- How can this disease be classified?
- What are the potential pathophysiological mechanisms for this disease?
- List potential treatment options available to manage this condition.
Case 2
An 82-year-old diabetic man with a long-term catheter presented to the Emergency Department with rigors and non-specific abdominal pain. He had an elevated white cell count (WCC) and C-reactive protein (CRP). An abdominal and pelvic CT scan was arranged. Selected CT images are shown below:
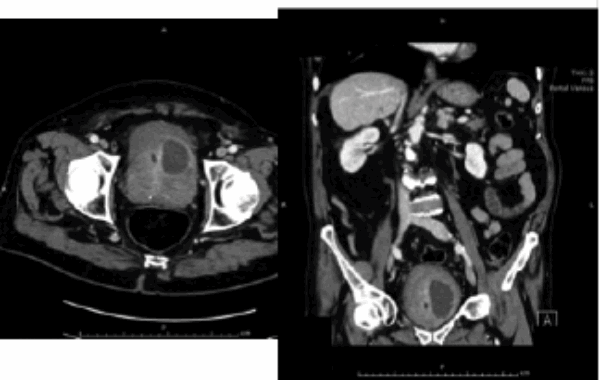
- Describe the CT findings. What is the diagnosis?
- What is the pathophysiology of this condition?
- What are the risk factors?
- What is the most likely causative organism?
- How can it be drained?
Case 3

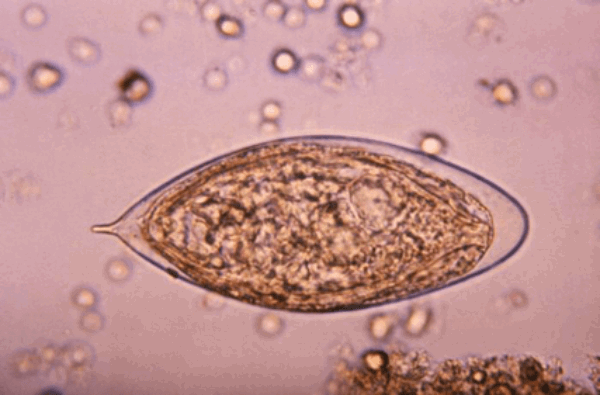
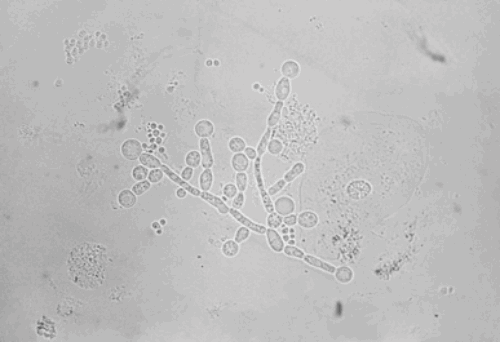
Above are some selected infective microorganisms seen in urological practice.
- Name the organism based on the images shown?
- What are the normal host defence mechanisms to prevent urinary tract infection (UTI)?
- How common is asymptomatic bacteriuria? When should it be treated?
- How do you manage a patient with asymptomatic candiduria?
- What are the common risk factors for candiduria?
Infections and Inflammation: part 2 – answers
Case 1
-
Figure 1: Hunner’s ulcer.
Figure 2: post distension glomerulations. Interstitial cystitis / bladder pain syndrome (BPS).
-
Cystitis: microbiological / chemical / radiation / drug (cyclophosphamide). Overactive bladder syndrome / detrusor overactivity.
Malignancy: urological / gynaecological / abdominal / pelvic.
Endometriosis / uterine fibroids.
-
BPS is classified on cystoscopic appearances by the ESSIC into normal (grade 0), glomerulations grade II-III (grade I denoted petechiae in at least two quadrants), and Hunner’s lesions. Cystoscopy findings combined with histological on biopsy enables a more detailed classification as per the ESSIC guidelines.
-
Mast cell release of histamine, defective GAG layer of bladder with consequent abnormality of urothelial permeability, neurogenic mechanism, reflex sympathetic dystrophy of the bladder, autoimmune response and urinary toxins.
-
Behavioural: patient education, dietary modification (avoidance of triggers: citric fruit, tomatoes, vitamin C, coffee / tea, spicy food, alcohol, caffeine), stress reduction, pelvic floor rehabilitation through physiotherapy.
Medical: H2 antagonists, epithelial repair (pentosan polysulfate), inhibit neural activity (amitriptyline), nonsteroidal anti-inflammatory drugs / paracetamol.
Intra-vesical: dimethyl sulfoxide (DMSO), combined GAG replacement therapy, alkalinised lidocaine.
Surgery: resect Hunner’s lesions, bladder augmentation / diversion / cystectomy.
Other options: BTX-A with hydrodistension, oral cyclosporine A
Case 2
-
There is a peripherally enhancing collection in the left anterosuperior aspect of the prostate. Diagnosis: left sided prostatic abscess.
-
Infected urine reflex into the prostate, haematogenous spread (commonly Staph aureus), direct spread (transrectal ultrasound guided biopsy).
-
Diabetes, immunocompromised (steroids / HIV / chemotherapy), chronic bacterial prostatitis, long-term catheter.
-
E. coli (up to 80%), other enterobacteriaceae (Klebsiella, Enterobacter and Serratia species) (3-11%), Proteus species (5%), Pseudomonas aeruginosa (5%).
-
Transurethral drainage (selective transurethral resection of the prostate over abscess) or perineal aspiration and drainage under radiological guidance.
Case 3
-
Figure 1: E.coli (clue: rod shaped).
Figure 2: Schistosoma haematobium (clue: terminal spine).
Figure 3: Candida albicans (clue: spore forming).
-
Host defence: antegrade flow of urine, acidic urine, exfoliation of epithelial cells, lactobacillus of vagina, intact GAG layer, Tamm-Horsfall protein (uromodulin) - binds Type 1 pilli of E.coli.
-
Up to 5% of patients. Treat during pregnancy (4-7% incidence) as increased risk of pyelonephritis (20-40% will develop pyelonephritis).
-
No treatment is needed unless the patient is high-risk (neutropenia, low birth weight infant) or undergoing urological manipulation. Symptomatic patients must be treated.
-
Indwelling catheters and stents, elderly age, antibiotic use, neutropenia, underlying gastrointestinal tract abnormalities, previous surgery and diabetes.




