Case 1
A 28-year-old female, 19 weeks pregnant, presents with severe left loin pain. There is no past medical history of note. Blood tests show a white cell count of 14.1x109/L and creatinine of 56umol/L. An ultrasound scan (USS) reports left moderate hydronephrosis and right mild hydronephrosis.
- How common is hydronephrosis in pregnancy?
- What is the mechanism of hydronephrosis in pregnancy?
- What factors influence stone formation in pregnancy?
- How do stones present in pregnancy?
- What imaging options are available for this patient and what are the advantages / disadvantages of each?
- What is the radiation dose of a CT of kidney, ureter, bladder (KUB) and what dose of radiation is considered safe?
Case 2
A 19-year-old female who is 25 weeks pregnant presents unwell with severe right flank pain and fever. Urine dip shows blood, leucocytes and nitrites.
- What investigations should be performed?
- What management should be initiated?
- What classes of antibiotics are suitable for use in pregnancy?
- What types of analgesia are safe for use in pregnancy?
- How common is bacteriuria in pregnancy and how should this be managed?
- What are the options for draining an infected obstructed kidney in pregnancy? What are the main disadvantages of each of these?
- What are the indications for drainage?
Case 3
A 26-year-old attended for an elective ureteroscopy for a 9mm renal stone. She was found to be pregnant and her ureteroscopy was cancelled. She presents a few weeks later at nine weeks gestation with severe right flank pain. There are no features of sepsis.

1. What does this ultrasound of the right kidney show and what does this suggest?
2. What are the management options for this patient?
3. How often should a nephrostomy tube be changed in pregnant patients?
4. What are the potential complications of renal stones in pregnancy?
5. What are the principles of ‘ALARA’ with regards to radiation?
6. What measures can pregnant staff take to reduce radiation exposure from image intensifiers during stone procedures?
Kidney stones in pregnancy: answers
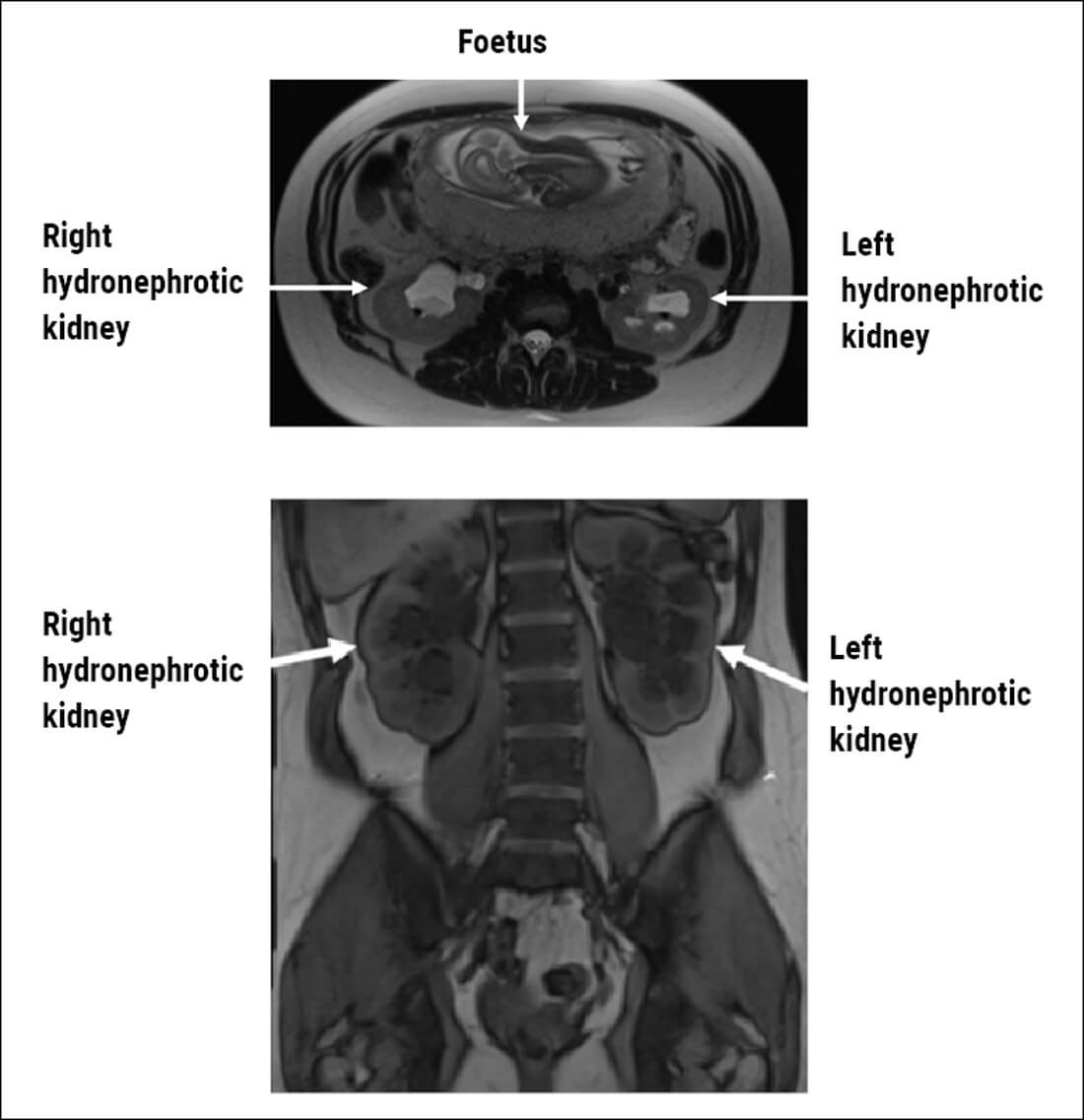
Figure 1: MRI scan in axial and coronal planes showing bilateral hydronephrosis in pregnancy.
Case 1
- Physiological hydronephrosis is present in more than 80% of pregnant women. By the third trimester, it is present on the right in 90% and on the left in 67% of women.
- There is increased smooth muscle relaxation and reduced peristalsis in the ureter secondary to progesterone. In later stages of pregnancy, there is direct compression of the ureter from the enlarged gravid uterus. There is commonly dextro-rotation of the uterus leading to more compressive effects on the right than the left. The left ureter is also protected to a degree by the sigmoid colon and its mesentery. Hydronephrosis usually resolves by six weeks post-partum.
- Lithogenic factors include increase in renal plasma flow and glomerular filtration rate leading to increased urinary excretion of calcium, uric acid, sodium and oxalate. Also, there is reduced tubular reabsorption of calcium due to suppression of parathyroid hormone. Hydronephrosis leads to urinary stasis which increases the risk of stone formation. However, there is an increase in urinary excretion of inhibitors of stone formation including citrate, magnesium and glycoprotein nephrocalcin. Urine alkalinity during pregnancy also inhibits stone formation. Therefore, the overall risk of stone formation is similar to non-pregnant patients.
- Flank pain, visible or non-visible haematuria, urinary tract infection or found incidentally during scanning.
- Ultrasound is the best first-line option as it is widely available and does not involve radiation. However, it has low sensitivity for renal and ureteric calculi. An additional option is MRI (Figure 1). MRI is expensive, and less readily available. MRI has increased accuracy when compared with US. MRI can show hydronephrosis and occasionally filling defects. There are no known risks from US or MRI during any trimester, but the use of contrast agents such as Gadolinium should be avoided. Ionising radiation should in general be avoided if possible. With the evolution of ultra-low dose CT, there is an option for diagnostic certainty with very little risk of radiation dosing to the foetus, but this is typically reserved for patients in whom surgical interventions are being planned as CT will lead to fewer negative ureteroscopies, and therefore reduce the anaesthetic risk to mother and foetus.
- Mean dose 8mGy, compared with XR KUB which is 1.4mGY. Teratogenesis risk is very low with radiation doses below 50mGy but doses below 10mGY still carry a carcinogenic risk to embryo. Ultra-low dose CT can give effective radiation doses as low as 0.8mSv, but will need input from radiologists in each centre as protocols differ.
Case 2
- Urine microscopy and culture, blood cultures, blood tests including full blood count (FBC), urea and electrolytes (UE), C-reactive protein (CRP), calcium, lactate / blood gas analysis, imaging with USS in first instance.
- Sepsis 6 – cultures, lactate, urine output monitoring, oxygen, antibiotics, fluids. The obstetric team should be informed and involved in care.
- Penicillins and cefalosporins are safe. Antibiotics that should be avoided include aminoglycosides due to risk of auditory or vestibular nerve damage, trimethoprim because it is teratogenic (folate antagonist) and quinolones due to risk of arthropathy.
- Paracetamol is safe throughout pregnancy, and used IV is particularly effective for fever as well as ureteric colic symptoms. Non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided if possible, particularly in third trimester due to premature closure of patent ductus arteriosus in foetus. There is a risk of teratogenesis with codeine which should be avoided in the first trimester. Morphine can be used in low doses and short courses, although with caution in the late third trimester due to a risk of foetal opiate dependence.
- Asymptomatic bacteriuria is present in 4-7%. Of those, 20-40% develop pyelonephritis, usually in the third trimester, therefore where possible asymptomatic bacteriuria in pregnancy should be treated.
- Options – retrograde ureteric stent or percutaneous nephrostomy tube. Disadvantages: Retrograde ureteric stent – general anaesthetic, failed access into ureteric orifice, stent symptoms, need for fluoroscopy, tortuous anatomy in later pregnancy, extrinsic compression leading to stent failure. Percutaneous nephrostomy – bleeding risk, damage to kidney / visceral injury, external tube at risk of dislodging / blocking, pain at site. Both carry a risk of encrustation and bacterial colonisation and will need changing every six to eight weeks at least. If a stent is used in early pregnancy, the risk of repeat general anaesthetics needs to be considered.
- Obstruction in solitary kidney, bilateral obstruction, active infection, deteriorating renal function, signs of pre-eclampsia / preterm labour, severe pain refractory to analgesia.
Case 3
- Moderate hydronephrosis suggestive of stone migrating to the ureter. Physiological hydronephrosis of this extent is unusual in early pregnancy.
- Analgesia and conservative management if able to manage pain, with option to perform ureteroscopy in second trimester (reduced risk after 12 weeks). Nephrostomy / stent until second trimester then undergo a ureteroscopy. Nephrostomy / stent until end of pregnancy with repeated changes then ureteroscopy. Extracorporeal shock wave lithotripsy is contraindicated in pregnancy. Further imaging will be required to confirm presence of ureteric stone prior to ureteroscopy as stones may pass spontaneously in 50-80% of patients.
- Every six to eight weeks due to the risk of encrustation in stone formers, or more often if encrusting.
- Pre-term labour, miscarriage, sepsis, pre-eclampsia, low birth weight. Women of childbearing age who have kidney stones should be counselled about risks and should consider treatment to achieve stone-free status prior to pregnancy.
- ‘As low as reasonably achievable.’ Using the minimum amount of radiation necessary to achieve an overall benefit. It involves where possible shielding the foetus with protective materials, maximising distance from source of radiation and reducing time of exposure to radiation.
- Personal choice to avoid any procedure involving radiation. Otherwise, double lead gown (skirt and top preferable). However, this can be heavy. They can also stand further away from C-arm if possible. A personal radiation dosimeter should be worn to measure the cumulative dose. It is also important to follow the ALARA principles at all times, and take steps to minimise scattered radiation in the operating theatre as above.
Further reading
1. Somani BK, Dellis A, Liatsikos E, Skolarikos A. Review on diagnosis and management of urolithiasis in pregnancy: an ESUT practical guide for urologists. World J Urol 2017;35(11):1637-49.
2. Demir M, Yagmur İ, Pelit ES, et al. Urolithiasis and its treatment in pregnant women: 10-year clinical experience from a single centre. Cureus 2021;13(3):e13752.
3. Meher S, Gibbons N, DasGupta R. Renal stones in pregnancy. Obstet Med 2014;7(3):103-10.
4. Masselli G, Weston M, Spencer J. The role of imaging in the diagnosis and management of renal stone disease in pregnancy. Clinical Radiology 2015;70(12):1462-71.
5. Thakur AP, Sharma V, Ramasamy V, et al. Management of ureteric stone in pregnancy: a review. Afr J Urol 2020;26:60.
6. Talwar HS, Panwar VK, Ghorai RP, Mittal A. Catastrophic complications of urolithiasis in pregnancy. BMJ Case Reports CP 2021;14:e241597.







