Case 1
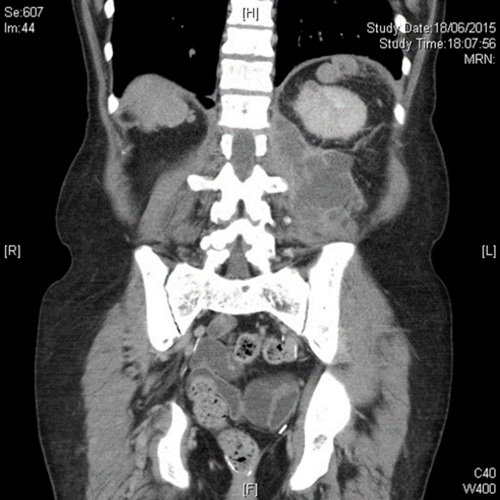
An 80-year-old woman presented with history of recurrent and recent cystitis, low grade pyrexia, abdominal and back pain, and pain on movement of the left hip which was observed to be flexed and externally rotated.
- What is the diagnosis from the CT image?
- What are the usual sources of this infection?
- What are the principles of management?
Case 2
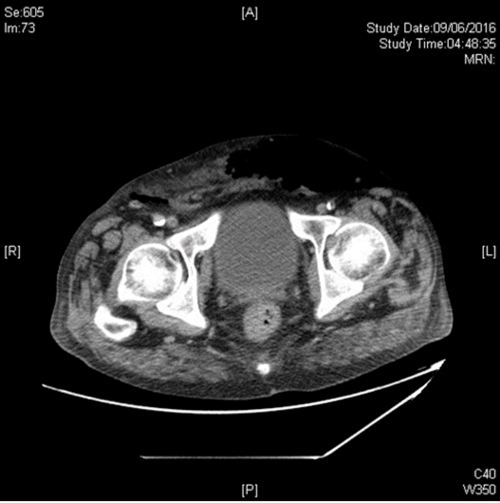
A 72-year-old diabetic man presented with acute confusion, tachycardia and pyrexia of 400C after reportedly having had a fall. He was found to be anuric and at the time of catheterisation he was found to have a swollen scrotum with erythema and crepitus extending up onto the perineum, anterior abdominal wall and loin. The posterior aspect of the scrotum was dark purple in colour. Emergency CT detected gas in the retroperitoneum and anterior abdominal wall.
- What is the diagnosis?
- What is the typical microbiology from this condition?
- What is the treatment of choice?
- What is the mortality from this condition?
Case 3
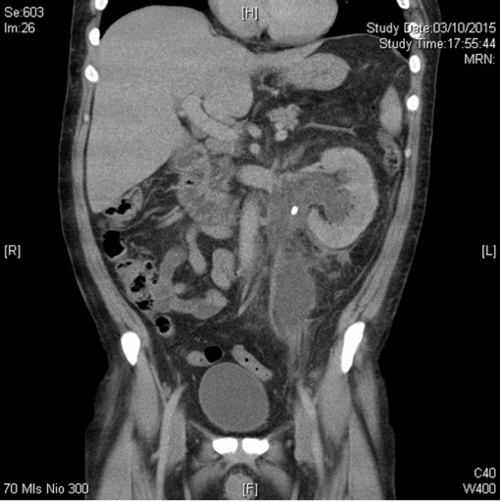
A 42-year-old woman presented with left loin pain radiating to the left iliac fossa, pyrexia and feeling generally unwell with spontaneous decompression of the pelvicalyceal system. Her inflammatory markers (WBC, CRP) and serum creatine were raised and she looked unwell.
- What would be your approach to decompress this?
- Name two major complications associated with the percutaneous approach.
Retroperitoneal sepsis – answers
Case 1
-
Iliopsoas abscess. The classic triad of back pain, limp and fever may actually be present in only 30% of cases. Many patients have an insidious onset of non-specific symptoms and signs. The flexed and externally rotated hip is a consequence of irritation of the psoas muscle and referred pain from the nerve roots L2, L3 and L4 which supply the psoas muscle [1].
-
The known origins of secondary spread of infection to the iliac or psoas muscles may be broadly categorised into: a) Gastrointestinal (e.g. Crohn’s disease, diverticulitis, appendicitis, colorectal carcinoma); b) Genitourinary (e.g. urinary tract infections including pyelonephritis, instrumentation); c) Musculoskeletal infection (e.g. vertebral osteomyelitis, septic arthritis, infective sacroilitis); d) Others (endocarditis, trauma, femoral artery catheterisation, etc. Tuberculous infection has been implicated from both haematogenous spread and spread from adjacent TB focus, either skeletal, gastrointestinal or genitourinary).
-
First-line treatment is broad spectrum antibiotics that cover S. aureus (the most commonly isolated organism on cultures from aspirates). Surgical draining is the traditional treatment of choice with some authors describing quicker recovery after, although percutaneous drainage under imaging guidance is a good alternative. The latter may not be effective when small or multiple / multiloculated abscesses occur, or if access if difficult. A co-existing intra-abdominal disease requiring surgical intervention, such as complex Crohn’s disease or diverticulitis, may also determine which option is chosen. Small abscesses may be successfully treated with antibiotics alone [1].
Case 2
-
Fournier gangrene, a potentially life-threatening form of necrotising fasciitis involving the male genitalia. It was originally reported by Baurienne in 1764 and by Fournier in 1883 [2].
-
Wound cultures often yield mixed growth with a combination of aerobic (e.g. E. coli, klebsiella, enterococci) and anaerobic organisms (bacteroides, clostridium, microaerophilic streptococci).
-
Prompt diagnosis is critical because of the rapidity with which the condition progresses. Immediate debridement is essential, with extension excision of all infected tissue until normal fascial planes are found. This may extend up into the abdomen or into the perineum, as in this case. Orchidectomy is almost never necessary because the testis have their own blood supply and do not usually get involved by the infective process. If the urethra is suspected to be involved a suprapubic catheter should be inserted. This should be combined with aggressive resuscitation and broad spectrum antibiotic cover in advance of the surgical debridement [2].
-
The mortality rate averages approximately 20% [2].
Case 3
-
The drainage of acute renal obstruction, especially when suspected to be associated with infection, is a urological emergency. Obstruction can be drained by either retrograde ureteric stent (RUS) insertion or percutaneous nephrostomy (PCN). Current guidelines do not provide specific recommendations on the choice between these options [3,4]. This particular patient had a retrograde stent inserted followed by a percutaneous drain in the retroperitoneal collection with broad spectrum antibiotic cover.
-
Quality improvement guidelines for percutaneous nephrostomy recommend a major complication rate of <4% which is achievable [5] although most series report combined major and minor complication rates of approximately 10% [4]; these include severe bleeding, renal loss and septic shock. Reference 5 provides a usefully detailed overview on the subject.
References
1. Shields D, Robinson P, Crowley TP. Iliopsoas abscess - A review and update on the literature. International Journal of Surgery 2012;10:466-9.
2. Schaeffer AJ, et al. Infections of the Urinary Tract. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA (Eds). Campbell-Walsh Urology, 11th edition, Philadelphia, USA; Elsevier; 2016;237-303.
3. Lynch MF, Anson KM, Patel U. Current opinion amongst radiologists and urologists in the UK on percutaneous nephrostomy and ureteric stent insertion for acute renal obstruction: results of a postal survey. BJU International 2006;98(6):1143-4.
4. Türk C (Chair). EAU Guidelines on Urolithiasis. http://uroweb.org/wp-content/uploads/EAU-Guidelines-Urolithiasis-2016.pdf. Accessed 26 July 2016.
5. Dagli M, Ramchandani P. Percutaneous nephrostomy: technical aspects and indications. Semin Intervent Radiol 2011;28:424-37.




