Case 1
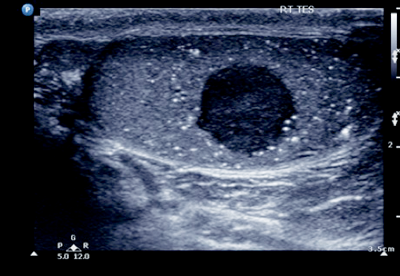
- What does the ultrasound show?
- What further imaging does this patient require?
- Which tumour markers should be checked?
- What is the half-life of these markers?
- What does an elevation in these markers mean?
Case 2
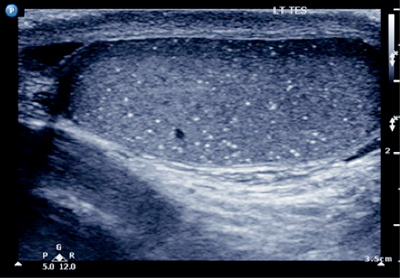
- What is this pathology?
- How is this pathology defined?
- When is this pathology a risk factor for testicular cancer?
- If they have a risk factor and microlithiasis, what is the preferred treatment option?
Case 3
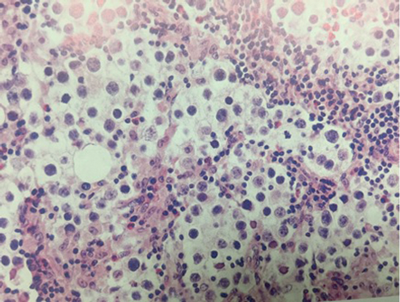
- What does this testicular histological specimen show?
- What are the prognostic factors for occult metastatic disease in seminoma?
- How are the different prognostic groups for metastatic seminoma defined?
- What are the treatment options for stage 1 seminoma?
Testicular cancer – answers
Case 1
-
Right-sided testicular mass with associated microlithiasis.
-
Staging CT chest / abdomen and pelvis.
-
α-Fetoprotein (ALP), β-human chorionic gonadotrophin (HCG), lactic dehydrogenase (LDH).
-
α-FP is 5-7 days, β-HCG is 24-36 hours.
-
α-FP: implies yolk sac element, non-seminomas germ cell tumours (NSGCT) (50-70% elevated), NOT elevated in seminoma. Differential: alcohol abuse, viral hepatitis, hepatotoxic drugs. β-HCG: implies syncytiotrophoblastic elements, choriocarcinoma, NSGCT (40-60% elevated), seminoma (up to 30%). LDH: less specific marker, its concentration is proportional to tumour volume.
Case 2
-
Microlithiasis.
-
Five or more echogenic foci per high powered view, in either or both testes.
-
Contralateral testis cancer, small testicle (<12mls), infertility, cryptorchidism or atrophic testis.
-
Testicular biopsy.
Case 3
-
Testicular seminoma: characteristically shows a combination of large neoplastic cells with clear cytoplasm and lymphocyte-rich stroma. Some tumours have fibrosis due to a histiocytic granulomatous response.
-
Tumour size >4cm, invasion of the rete testis.
-
Good prognosis: no non-pulmonary visceral metastasis, normal αFP, any β-HCG/LDH. Intermittent prognosis: non-pulmonary visceral metastasis, normal αFP, any β-HCG/LDH.
-
Surveillance or one course adjuvant carboplatin-based chemotherapy (single-dose carboplatin is less toxic and as effective as adjuvant radiotherapy).






