Case 1
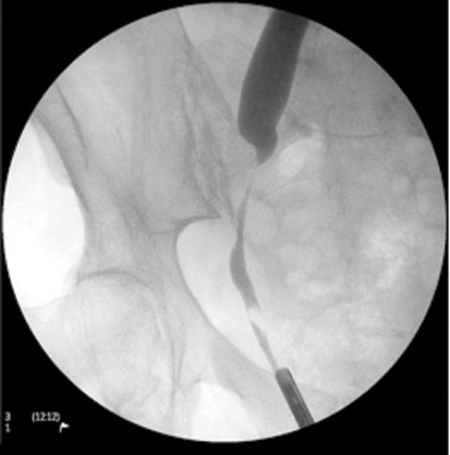
- What is this investigation? What are the findings of this investigation?
- What are the causes for this?
- What are the treatment options?
Case 2

Image 1.

Image 2.
- What do these X-Ray KUB films show?
- What are the complications of ureteric stents?
- How can stent pain be minimised?
Case 3
Image 1.

Image 2.
- What do the X- Ray KUB images show?
- What is this metallic device made of, and how does it work?
- What are the advantages of this device over a standard ureteric stent?
- What are the complications associated with this device?
Ureteric strictures – answers
Case 1
-
Retrograde ureterogram. A narrowing of the right ureter at the pelvic brim with proximal ureteric dilatation. An air bubble can also be seen within the lower ureter.
-
Latrogenic (instrumentation, pelvic surgery, radiotherapy), post impacted stone, extrinsic compression (malignancy, collection, lymph nodes, etc), retroperitoneal fibrosis, transitional cell tumours and trauma.
-
Endoscopic: ureteric stents (temporary or permanent with plastic or metallic stents), ureteric dilatation and ureteric incision. Reconstruction: depends on site and length of stricture. Options include ureteroureterostomy, transureteroureterostomy, re-implantation +/– psoas hitch and Boari flap. Nephrectomy: for a non-functioning kidney.
Case 2
-
Image 1: Ureteric stent with stone formation in the bladder, mid ureter and renal pelvis. A left upper calyceal renal calculus.
Image 2: Bilateral ureteric stents, right ureteric stent deviation secondary to retroperitoneal lymphadenopathy and part of an inferior vena cava (IVC) filter in-situ. This patient has metastatic testicular cancer with bulky retroperitoneal lymphadenopathy and deep vein thrombosis (DVT).
-
Stent pain (80%), encrustation, migration, fracture, occlusion and stone formation. Bladder storage and reflux symptoms, dysuria, haematuria and infection. Impairment of sexual and quality of life.
-
Avoid stents if possible and minimise duration. Analgesia, alpha-blockers or combined treatments (alpha-blockers / anti-cholinergics) are effective [1,2].
Case 3
-
Image 1: Memokath in left mid-ureter plus left nephrostomy.
Image 2: Memokath migration into bladder.
-
The Memokath is a thermo-expandable nickel-titanium alloy stent. It retains its normal shape at room temperature to allow placement in the ureter and expands when warmed to aid deployment.
-
Lower incidence of migration and occlusion, reduced tumour ingrowth, reduced bladder / renal irritation symptoms, long-term cost-effectiveness and low risk of encrustation.
-
Encrustation, migration, occlusion (debris, stone, matrix or tumour).
References
1. Lamb AD, Vowler SL Johnston R, et al. Meta-analysis showing the beneficial effect ofα- blockers on ureteric stent discomfort. BJUI 2011;108(11):1894-902.
2. Lim KT, Kim YT, Lee TY, Park SY. Effects of tamsulosin, solifenacin, and combination therapy for the treatment of ureteral stent related discomfort. Korean J Urol 2011;52(7):485-8.






