Hôpital Général Idrissa Pouye (HOGIP), formerly Hôpital Général de Grand Yoff – HOGGY), in Dakar, Senegal, is one of the most well-regarded teaching hospitals in West Africa. It has over 300 beds, a urology team of six consultants and attracts trainees from a number of West African countries. It has established itself as the premier centre for reconstructive and endoscopic urology in West Africa.
After assisting in delivering the first laparoscopic workshop in 2017 with IVUmed [1], Zeeshan Aslam was approached by the local team to continue the training and a further workshop was organised in 2019. The objective that was set at the time was to establish a recurrent and structured workshop at HOGIP running every 6-12 months. Following these successful trips the team at HOGIP would start to perform laparoscopic varicocoele ligations independently.
Unfortunately, the COVID-19 pandemic interrupted the return of further workshops but after almost three years and with COVID-related uncertainty still looming, we were able to assemble a faculty and restart the mission. As an ST5, I was given the opportunity to join Zeeshan and Mazhar Sheikh as part of the faculty and help deliver another structured five-day laparoscopic workshop alongside Professor Lamine Niang. Importantly the workshop has now gained Royal College of Surgeons of Edinburgh (RCSEd) accreditation. This article follows on from the report by Matt Trail published in 2020 [2] and details our experiences from the latest workshop.
In the weeks leading up to the workshop a teleconference was set up to run a virtual multidisciplinary team (MDT) meeting to discuss and select the appropriate cases for the live operating days. The workshop was further facilitated by the generous donations from Medtronic and Applied Medical, which helped acquire most of the essential laparoscopic equipment necessary for safe operating.

The host and visiting faculty with the residents after the first half-day of lectures.
Following our arrival in Dakar in the early hours of Sunday morning, we met up with Prof Niang who kindly helped us explore the city. A very moving experience for me was visiting the historically significant Gorèe Island where we learned its harrowing history. After a busy sleep-deprived Sunday of exploration, we made final adjustments to the programme in the evening in preparation for the busy week ahead.

Exploring the city and cooling down with a refreshing drink.
The workshop experience
Day 1: Seminars and introduction to simulation
We were all made to feel very welcome in Dakar but especially so on reaching HOGIP. It was really pleasing to see how Zeeshan was greeted like family by the host team. After a quick tour of the urology department, we set up in the seminar room and were soon introduced to the residents.
The number of residents and fellows had almost doubled from the previous workshop to 26 with up to 13 different nationalities present, from North and West Africa including Togo, Guinea, Burkina Faso, Gabon, Central African Republic, Cameroon, Morocco, Algeria, Mauritania and Tunisia. Some of these countries don’t have any dedicated practising urologists e.g. Central African Republic.

An introductory talk by Jamie Krishnan.
In the first half of the day, we delivered a number of short lectures including laparoscopic access, laparoscopic nephrectomy and pyeloplasty. There was also an interesting progress report on the local team’s experience in performing laparoscopic varicocoele ligations, a skill that they have mastered during the pandemic. The finalised list of planned cases for the live operating days was then reviewed.
"The workshop was a resounding success and a testament to the hard work, dedication and skill of the host and visiting teams"
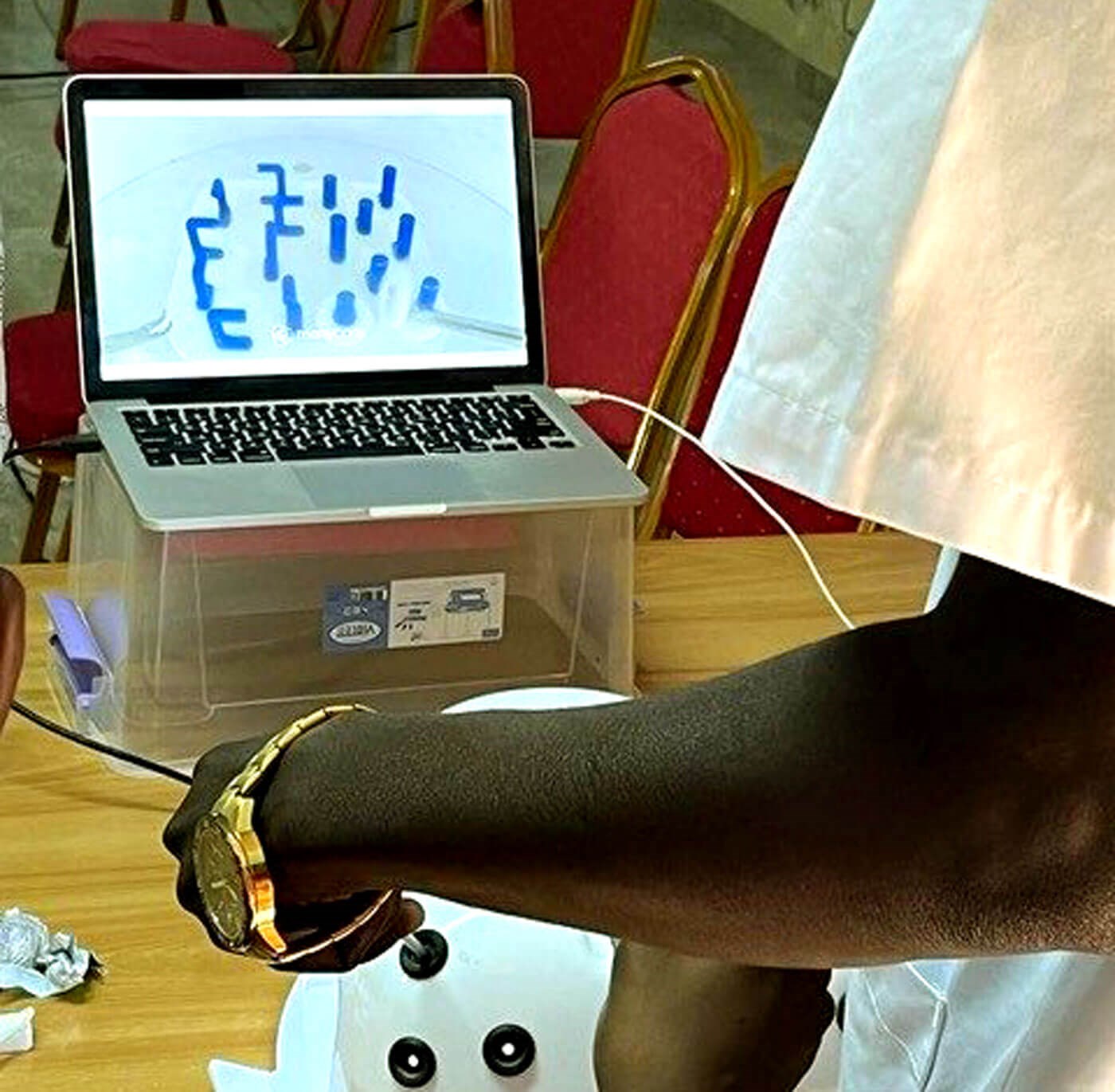
The afternoon was spent running a laparoscopic simulation workshop on a set of rather impressive box trainers and a ‘low-tech DIY’ box trainer made with a felt lined laundry box. Over the course of the week, the simulation exercises evolved from dry-lab to wet-lab based work using chicken and porcine tissue. For a number of trainees this was their first experience of laparoscopic surgery and simulation, so was an exciting exercise which was very well received as evidenced by the outstanding feedback that we were given. I was responsible for much of the simulation teaching over the course of the workshop and thoroughly enjoyed the near-peer teaching element of it.
Day 2-4: Parallel running of live surgery and simulation sessions
As the objective was to move to more advanced laparoscopic procedures, we planned to maximise the training opportunities. As a result, the lists were kept intentionally light with one major case listed per day – one radical nephrectomy and two simple nephrectomies followed by simpler procedures such as varicocoele and renal cyst decortication in the afternoon. This removed the time pressure on the surgeons and supervisors, minimised fatigue and made for an environment more conducive to learning.
The first case, a laparoscopic left radical nephrectomy was performed by Prof Niang under supervision of senior faculty. I was able to attend theatres intermittently, having set up and demonstrated a number of exercises in the sim lab earlier to the trainees. The excitement among the trainees was evident as half of them were present in theatre, while the other half were in the sim lab and there was palpable disappointment among those who did not get to perform the scrub nurse role.
A resident performing one of the simulation exercises.

Another resident performing an exercise on a second box-trainer.

Prof Niang and Dr NDoye about to start a laparoscopic nephrectomy.
With Prof Niang and his team’s commitment to laparoscopy in the last two years, and successfully having performed some of the surgical steps for major procedures in the past, the rate at which they progressed and were able to perform much of the nephrectomy was impressive and inspiring. Both Dr Ndoye and Prof Niang took turns and were each primary surgeon. All three major cases were performed by the host team under supervision with no adverse events. The handling of the renal hilum was particularly meticulous and very encouraging to see. It truly was heartening to see how the structured mentorship was paying dividends. This was also true of the trainees who recorded notable improvements in their scores for their simulation exercises over the course of the week.
Day 5: Debrief and target setting
After a busy and tiring week, the workshop was a resounding success and a testament to the hard work, dedication and skill of the host and visiting teams.
The trainees expressed an interest in regular simulation-based workshops and the local faculty at HOGIP are well placed to provide this with the box trainers and equipment available. With greater experience among the consultant body now, we feel this is more likely to take off.
In addition to the primary mission, we also had the opportunity to meet the national Transplant Board and inform them of the success of the workshop. The Panel were deliberating setting up the nation’s first transplant centre at HOGIP and Prof Niang’s team pitched the ambitious aim of ultimately performing laparoscopic retrievals, as many of the transplants in Sub-Saharan Africa are live donor transplants.
Conclusion
There was a great sense of satisfaction and confidence by the end of the week. Having performed major laparoscopic procedures, the fear of the unknown had been faced and the host team now firmly believe that they can safely learn and perform these major procedures with some ongoing training. We, as faculty, completely agreed with that. The goal of developing laparoscopic urology in West Africa seems a step closer.
For me, this was a fantastic opportunity as a trainee to visit, and be involved in, a healthcare system in a low income country. It was an excellent chance to develop teaching, communication and surgical skills.
This was undoubtedly the best professional experience of my life, and my only regret was missing out on performing an open transvesical prostatectomy due to ill health on the final day. But this has now given me a reason to return to this wonderful country, which I would have done in any case.
I found exchanging clinical experiences with fellow trainees in HOGIP to be eye-opening and educational. While appreciative of the training I have received and the fortunate position I find myself in as a trainee in the UK with the relative abundance of resources we have here, I can’t help but be impressed and inspired by the consultants and trainees I met and their vast array of technical and non-technical skills.
The team at HOGIP are highly motivated, inspirational and ambitious and soon will be ready to develop and deliver their own laparoscopic urology service.
Acknowledgements
I would like to thank The Scottish Urology Society for supporting me on this endeavour.
References
1. Aslam Z. Is laparoscopic urological training in Sub-Saharan Africa a goal worth pursuing? Observations from my experience with IVUmed in Senegal. Urology News 2019;23(6):16-19.
2. Trail M, Thwaini A, Niang L, Aslam Z. Delivering a laparoscopic urology workshop in West Africa: our initial experience in Senegal. Urology News 2020;24(6):14-17.








