- CHARITY FOCUS -
Focusing on all of disease characteristics, societal factors, and better communication gives us real potential to fix a disparity that has persisted for too long.
When it comes to health inequity, the numbers are stark. Black men face 2 times the risk of a prostate cancer diagnosis [1] and 2.5 times the risk of dying [2], compared to their white counterparts.
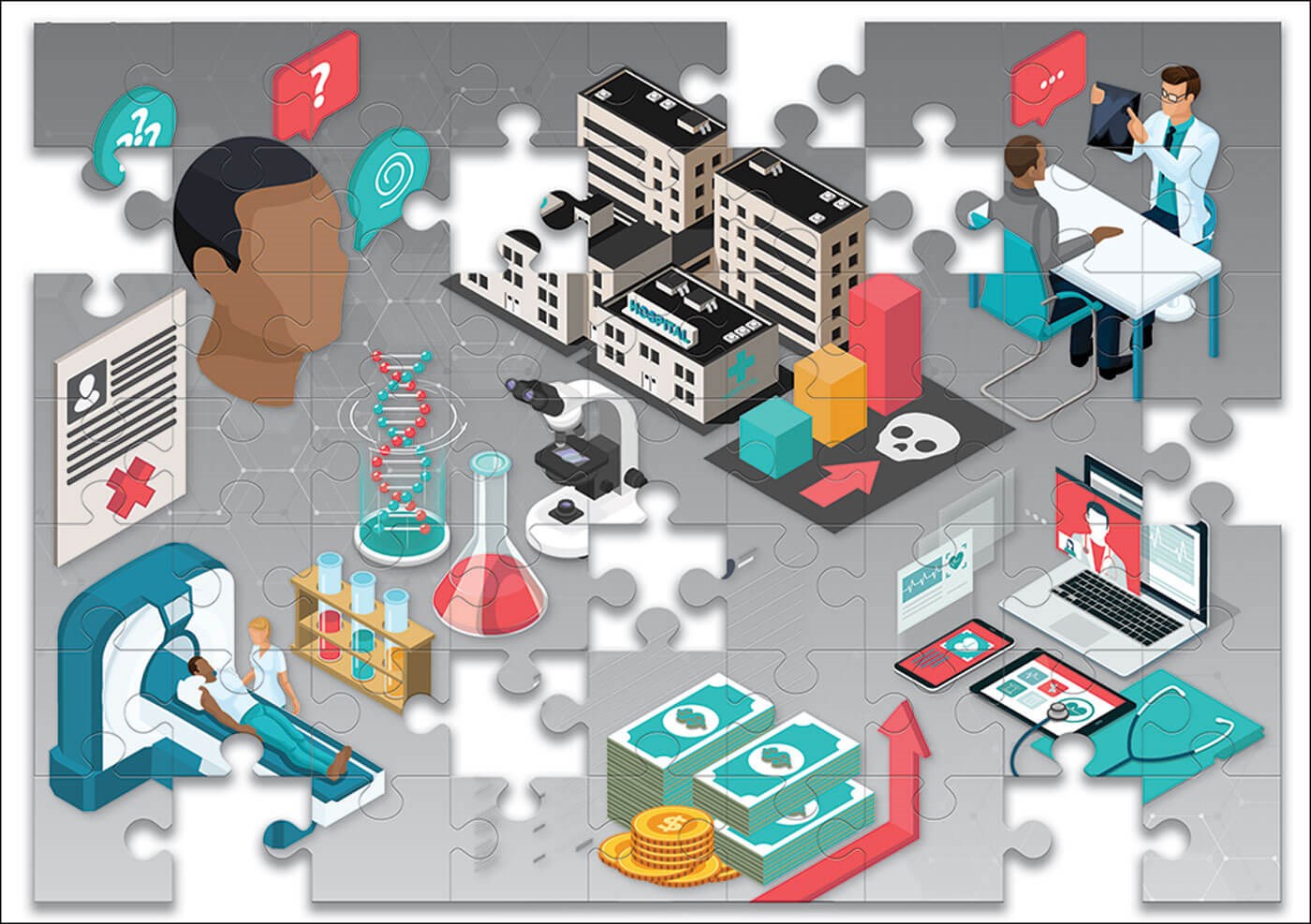
The incomplete jigsaw
Finding solutions to these inequities is like trying to make a recipe with only half the ingredients.
There are huge gaps in our knowledge – from the known unknowns, such as the lack of data from Black people in large Genome-wide association studies (GWAS) [3] and clinical trials [4]; the little-known knowns, such as how cancer is experienced differently by different communities [5], and how this affects their information and support needs, to the unknown unknowns, experiences not captured because people are missing from the data, or because the right questions haven’t yet been asked.
The biology piece
There are indications that biology has some part in Black men’s greater risks. Immigrant communities usually acquire the cancer risk of their new home countries within two generations [6], but this is not true for men of African origin, suggesting an ancestral component. Various key genetic and molecular changes, such as LSAMP deletion [7] (associated with rapid progression), mutations of the key prostate cancer lynchpin, the androgen receptor [8], and deletion of tumour suppressor PTEN [9], differ between ethnic groups.
Prostate Cancer Research is funding research investigating how microRNA changes affecting androgen signalling differ between populations, and so could identify Black men at increased risk. Another funded project is developing an epigenetics-based test tailored for Black men (www.prostate-cancer-research.org.uk/project/genetic-test-for-prostate-cancer-in-black-men), which could beat the accuracy of the currently used prostate specific antigen (PSA) test. Further projects interrogate the role of ancestry and of ethnic differences in immunity in cancer risk, and a new potential therapy. Taking these lines of enquiry brings us closer to closing the gap for this community.
The society piece
Society contributes to health inequalities in several complex and overlapping ways. While we have the power to make individual choices, those choices are constrained by the world around us. If we get sick, we won’t all have the same experiences in accessing healthcare and receiving support. Our research has revealed that non-white patients perceive less empathy from their healthcare providers, and Black men are more likely to be offered less aggressive treatment, despite being more likely to have more aggressive tumours [10]. These are not things which an individual can solve: they need interventions on a wider scale.
We fund work to dissect the barriers Black men face in both receiving early diagnosis (www.prostate-cancer-research.org.uk/project/tackling-barriers-to-early-diagnosis) and in staying on cancer treatment, co-designing solutions with, by and for members of the community. We are also funding work investigating how neighbourhoods contribute to healthcare disparities (www.prostate-cancer-research.org.uk/project/reducing-barriers-to-screening-in-black-men-with-prostate-cancer), and what policymakers need to consider when they design our streets and our healthcare systems.
The communication piece
There’s little point in developing new treatments if they can’t be accessed. Low health literacy, which affects about half the population [11], has enormous human and economic costs, being linked to increased hospital stays [12], reduced treatment adherence [13] and increased mortality [14]. Less effective communication with healthcare professionals also means that the needs of a significant number of people are not being captured, which places even greater strain on the system.
Infopool: Prostate Cancer Research’s ground-breaking new platform.
We at Prostate Cancer Research have developed a ground-breaking platform, the infopool (www.theinfopool.co.uk). The infopool provides clear, easy-to-understand information on testing, treatment, side-effects and clinical trials in a mixture of formats, including animated and non-animated videos, pictures, infographics and illustrations. Crucially, it centres real people talking about the impact of decisions they have made, including what it’s like to live with the effects of different treatments. We believe integrating filterable stories from people who look and sound like those watching and reading them, is a revolutionary way of educating and empowering the hardly reached groups: Black men and people with low health literacy.
Fitting it all together
When trying to tackle deeply embedded inequities, it’s important to unlearn, relearn, and be proactive. Being mildly proactive doesn’t work. It took a targeted funding call to really start tackling this disparity through research. We had to do some unlearning about how to present healthcare information, as the way it has been done before has not been working for everyone, and that is why we developed the infopool. It is possible to have an impact against long-standing problems, but new, joined-up approaches must be taken.
For further information visit www.prostate-cancer-research.org.uk
References
1. Lloyd T, Hounsome L, Mehay A, et al. Lifetime risk of being diagnosed with, or dying from, prostate cancer by major ethnic group in England 2008–2010. BMC Med 2015;13:171.
2. DeSantis CE, Siegel RL, Sauer AG, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA Cancer J Clin 2016;66(4):290-308.
3. Peprah E, Xu H, Tekola-Ayele F, Royal CD. Genome-wide association studies in Africans and African Americans: expanding the framework of the genomics of human traits and disease. Public Health Genomics 2015;18(1):40-51.
4. Wissing MD, Kluetz PG, Ning YM, et al. Under-representation of racial minorities in prostate cancer studies submitted to the US Food and Drug Administration to support potential marketing approval, 1993-2013. Cancer 2014;120(19):3025-32.
5. Alexis O, Worsley A. An integrative review exploring black men of African and Caribbean backgrounds, their fears of prostate cancer and their attitudes towards screening. Health Education Research 2018;33(2):155-66.
6. Hemminki K, Försti A, Khyatti M, et al. Cancer in immigrants as a pointer to the causes of cancer. European Journal of Public Health 2014;24(1):64-71.
7. Petrovics G, Li H, Stümpel T, et al. A novel genomic alteration of LSAMP associates with aggressive prostate cancer in African American men. EBioMedicine 2015;2(12):1957-64.
8. Tan SH, Petrovics G, Srivastava S. Prostate Cancer Genomics: Recent Advances and the Prevailing Underrepresentation from Racial and Ethnic Minorities. Int J Mol Sci 2018;19(4):1255.
9. Khani F, Mosquera JM, Park K, et al. Evidence for molecular differences in prostate cancer between African American and Caucasian men. Clin Cancer Res 2014;20(18):4925-34.
10. Rude T, Walter D, Ciprut S, et al. Interaction between race and prostate cancer treatment benefit in the Veterans Health Administration. Cancer 2021;127(21):3985-90.
11. Health literacy - NHS digital service manual
https://service-manual.nhs.uk/
[Last accessed 29 March 2023].
12. Baker DW, Parker RM, Williams MV, Clark WS. Health Literacy and the Risk of Hospital Admission. Journal of General Internal Medicine 1998;13(12):791-8.
13. Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patient’s knowledge of their chronic disease: A study of patients with hypertension and diabetes. Arch Intern Med 1998;158:166-72.
14. Baker DW, Wolf MS, Feinglass J, et al. Health literacy and mortality among elderly persons. Arch Intern Med 2007;167(14):1503-9.









