Suprapubic catheters (SPCs) are in widespread usage in medical practice and this review will focus on the pre-assessment, indications, methods and complications that are associated with the insertion of an SPC. Although suprapubic catheter insertions may be done electively or acutely, the ability to gain access to the bladder in an emergency situation is a key surgical skill. In this short review we focus on the assessment, precautions and techniques for SPC insertion for a core surgical trainee in the acute setting.
History and examination
A comprehensive medical history should aim to elicit the reason for catheterisation. A catheter is sometimes not needed, such as when a patient has a residual volume but is not obstructed, is able to void, and opts to stay par for the course.
There are a number of reasons why a suprapubic route for bladder catheterisation may be necessary or preferrable in an emergency setting. If bladder drainage is required but urethral access cannot be achieved or should not be attempted, placement of a suprapubic catheter should be considered. Careful attention to the history provided by the patient and that in the medical records should reveal important information on previous catheterisation attempts, particularly a history of difficult or traumatic instrumentation. Any previous urological procedures that the patient has undergone should be noted prior to catheterisation. For example, inadvertent undermining of the bladder neck or clot retention after recent transurethral resection of the prostate (TURP), a history of urethral strictures, recent urethral surgery or suspected urethral trauma may presage difficult urethral catheterisation and may require consideration of an alternative to the standard urethral approach.
Assessment of suitability for catheterisation requires a thorough physical examination. Assessment of body habitus and confirmation of a clearly palpable bladder that is dull on percussion gives us a physical landmark to proceed with safe insertion of a suprapubic catheter. Presence of lower abdominal surgical scars, infection, and evidence of previous vascular surgery will alert the clinician to contraindications.
Examination of the external genitalia should aim to ascertain reasons why a urethral approach may be difficult or inappropriate, which may include meatal stenosis, known urethral stricture, or bleeding from the meatus after trauma. In case of pelvic fracture examination of the perineum, abdomen and urethral meatus will highlight possible urethral trauma.
Indications and contraindications
Insertion of a suprapubic catheter can be undertaken either in the elective setting or as an emergency procedure. There are a number of advantages to having a suprapubic catheter, such as avoidance of urethral pain, urethral erosion (traumatic hypospadias), urethral trauma on insertion and removal, reduction of risk of faecal contamination and thereby reduced risk of catheter-associated urinary tract infections (CAUTIs), and easier access to the catheter site for cleansing and replacement in patients with decreased mobility or who are wheelchair bound. Absence of a catheter from the proximity of the genitals may enable resumption of sexual activity. Clamping the SPC allows a trial of void if required.
Indications for the consideration of a suprapubic catheter include [1]:
- Acute urinary retention – SPC insertion as an emergency when it is not possible to safely perform urethral catheterisation.
- Chronic urinary retention – elective if it is deemed to significantly aid catheter care or improve the patient’s quality of life.
- Underlying neurological disease, such as in spinal cord injuries, cerebrovascular accidents, and multiple sclerosis where self-catheterisation is not an option.
- Urinary incontinence – SPC insertion can be considered when urethral catheterisation cannot provide safe and sanitary drainage of the bladder, or is more comfortable.
- Postoperative – short-term suprapubic catheterisation may sometimes be indicated in the postoperative setting, either to enable continuous irrigation without influencing bladder pressure, or after urogenital surgery where this approach facilitates urethral or bladder healing.
- Urethral trauma or after extensive genitourinary surgery where urethral access is unavailable or not preferable, an example being previous surgery for vulval carcinoma.
- Urodynamic studies – an SPC can be used as an alternative when urethral catheterisation is not possible.
The patient should also be fully assessed for the presence of contraindications to suprapubic catheterisation such as bladder malignancy, infection of the skin overlying the proposed site of insertion, previous extensive abdominal surgery and the presence of vascular grafts in the lower abdomen. While not a contra-indication, pregnancy would necessitate special precautions and due care is required in obese individuals.
Equipment
SPCs most commonly employ the Foley balloon catheters which are available in a range of sizes from 10F to 18F. Various SPC kits are available, such as the Add-a-Cath®, the Bonanno™ System and the S-Cath™ System which is currently most commonly available and employs a Seldinger approach (Figure 1).
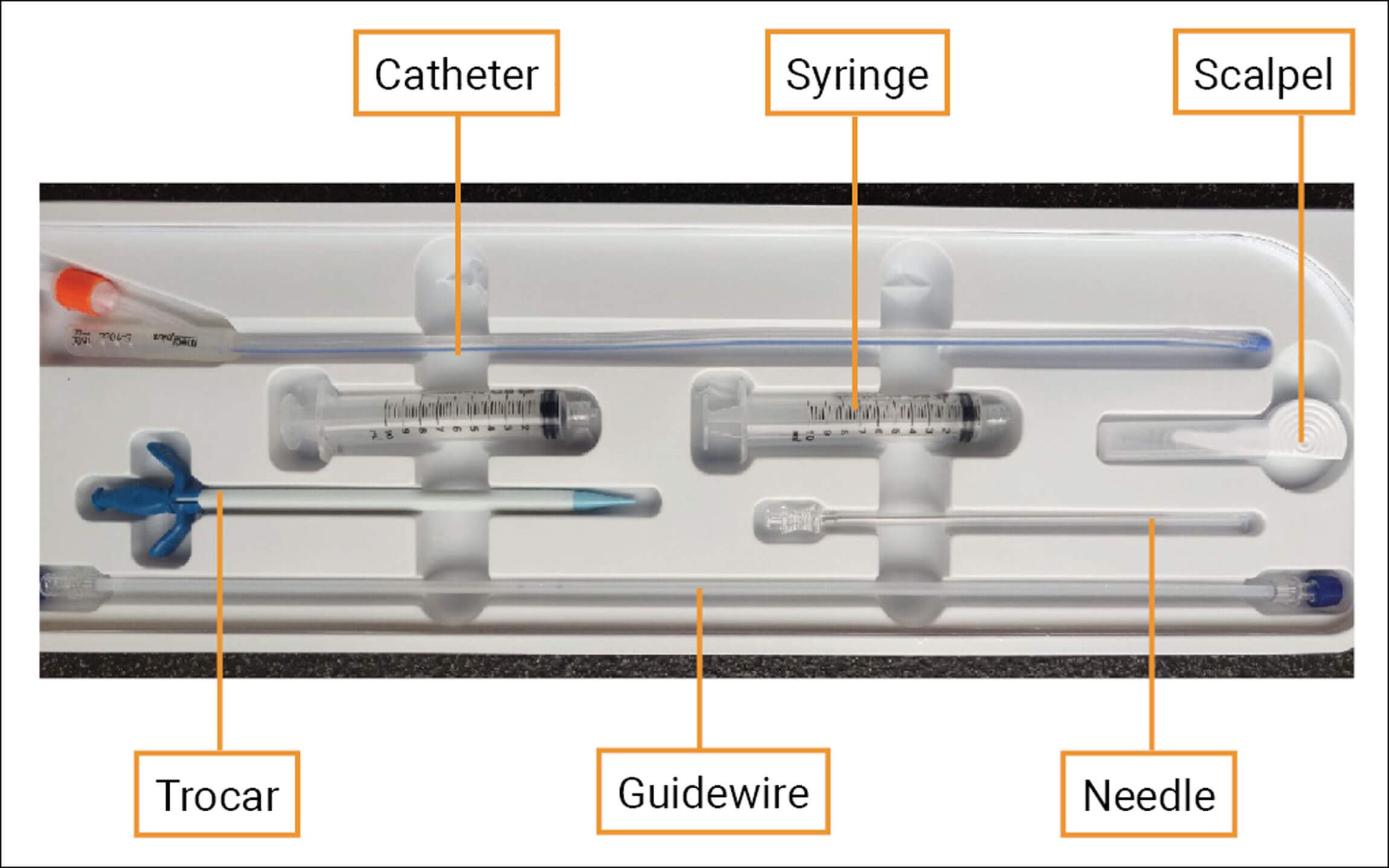
Figure 1: Kit for Seldinger approach to suprapubic catheterisation.
Technique of suprapubic catheterisation
There are various approaches to suprapubic catheterisation. The easiest option is to have access to a cystoscope – which may be a flexible scope under local anaesthetic (LA). This will enable adequate bladder distention and direct visualisation of the needle from inside the bladder. This may however not be immediately available in an emergency setting.
An alternative is an ultrasound guided approach where ultrasound is used to reliably ascertain if the bladder is distended. This may help identify interposing bowel along the route of the planned suprapubic track. This option should be considered when encountering an obese abdomen, a non-distended bladder that cannot be reliably confirmed to be full on palpation, or when there is a history of previous pelvic and lower abdominal surgery or radiotherapy. The needle is visualised as a hyperechoic structure on the ultrasound image. A radiographer should provide the images to enable the clinician placing the SPC to have both hands free.
Open insertion of SPC in operating theatres, when indicated, allows direct visualisation of the bladder.
Although trocar systems have been in widespread use for many years, SPC kits based on the Seldinger principle have become popular as they are considered safer. Both the Add-a-Cath and S-Cath Systems employ a peel-away trocar sheath, the principal difference being that the Seldinger system uses a floppy-tip guidewire that is advanced over an access needle. We describe the standard technique of SPC insertion using the Seldinger technique:
- Obtain informed consent and provide written information – including patient details and allergies, details of the procedure, alternative options, and potential complications (see below).
- Clean the site with an appropriate agent (e.g., Betadine®).
- Palpate 2cm above the pubic symphysis in the midline and confirm that the bladder is unequivocally distended. Avoid an obvious skin fold.
- Use an appropriate local anaesthetic (e.g. 20ml 0.5% bupivacaine) to create a subcutaneous bleb and then advance the needle whilst infiltrating along the track).
- Cap the spinal needle onto the syringe. Advance slowly in the vertical plane while aspirating until the bladder is reached.
- Once urine is aspirated, stop advancing the needle and detach the syringe from the needle.
- Pass the guidewire (floppy tip first) provided in the pack through the needle and remove the needle.
- Railroad the trocar over the guidewire using firm pressure guided by the index finger. You will need to make a small skin incision with a scalpel to enable introduction of the trocar.
- Remove the guidewire.
- Remove the trocar and place thumb on opening of sheath.
- Insert the Foley catheter and inject 10ml sterile water into the catheter balloon.
- Remove the outer sheath and the catheter should remain in position. Free movement within the bladder and unrestricted flow of urine confirms satisfactory positioning.
Complications
Clinicians and patients should be aware of potential complications of suprapubic catheterisation. These should be discussed with the patient prior to the procedure, both in acute and elective situations. Insertion of an SPC is an invasive procedure and the specific indications that justify it should be explained and documented. The British Association of Urological Surgeons (BAUS) patient information leaflet is quite comprehensive for this purpose (https://www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/Suprapubic.pdf).
Infection from the procedure should be recognised as a possible complication and be prepared for. A meta-analysis concluded that if the duration of catheterisation was more than five days, the risk of infection associated with suprapubic or intermittent catheters was lesser compared to that associated with use of an indwelling catheter (OR 0.142, 95% CI 0.073-0.276) [2].
Damage to the bowel is a serious and potentially fatal complication if unrecognised. Studies vary in their analysis of the rates of bowel injury following SPC insertion and range from 0.2-2.4% [3,4]. Septicaemia secondary to UTI occurs in 5-6% and catheter site bleeding occurs in another 2-3% of patients [3]. The risk of bowel injury is higher in cases when a suprapubic catheter is inserted into a bladder that is not fully distended [5].
The patient should be monitored for features of peritonitis and sepsis [6]. If the patient is septic post SPC insertion, the sepsis protocol should be commenced. If there is suspicion of bowel injury, initial management should prompt imaging using a contrast CT scan to delineate the injury along with escalation for further surgical management if indicated. The type of surgical management would depend on the extent of bowel injury and is beyond the scope of this article.
Replacement of a suprapubic catheter
As with any long-term urethral catheter, regular changes are required, usually every four to six weeks to three months unless otherwise indicated. However, a faulty or occluded catheter that is not unblocked by flushing would require an urgent change. The replacement catheter must be inserted immediately as the suprapubic channel can begin to close within a few minutes and access may be lost if re-insertion is delayed. This is more of a concern if the initial insertion has been recent.
Conclusion
Suprapubic catheters offer a viable alternative to the urethral option in specific circumstances, but require awareness of specific precautions and risks. Suprapubic catheterisation is a skill well worth learning for any surgical trainee who is part of an acute service, especially one with a special interest in urology. As with any other technique, practice with the help of a training model and a full understanding is important before the procedure can be undertaken judiciously and safely.
References
1. Harrison SC, Lawrence WT, Morley R, et al. British Association of Urological Surgeons’ suprapubic catheter practice guidelines. BJU Int 2011;107:77‑85.
2. Han CS, Kim S. Comparison of urinary tract infection rates associated with transurethral catheterization, suprapubic tube and clean intermittent catheterization in the postoperative setting: a network meta-analysis. J Urol 2017;198(6):1353-8.
3. Ahluwalia RS, Johal N, Kouriefs C, et al. The surgical risk of suprapubic catheter insertion and long-term sequelae. Ann R Coll Surg Engl 2006;88(2):210-13.
4. Hall SJ, Harrison S, Harding C, et al. British Association of Urological Surgeons suprapubic catheter practice guidelines – revised. BJU Int 2020;126:416-22.
5. Farina LA, Palou J. Re: Suprapubic catheterisation and bowel injury. Br J Urol 1993;72(3):394.
6. Hooton TM , Bradley SF. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 2010;50(5):625‑63.
Declaration of competing interests: None declared.









