In the fifth article in this series the authors describe some of the most complex cases they have encountered.
Case 1
A 45-year-old woman was admitted under the care of the medical team with shortness of breath, renal failure and abdominal distension six weeks post laparoscopic hysterectomy. A small right-sided pleural effusion was present on chest x-ray and large-volume ascites was identified on ultrasound. Drainage of both the chest and the abdomen confirmed the fluid to be urine.

Figure 1.
Bilateral retrograde studies revealed extravasation of contrast from the distal left ureter with the contrast seen travelling in a peritoneal pleural fistula on the right retrograde (Figure1.). After a failed attempt at inserting a left ureteric stent due to complete transection and retraction of the ureter a nephrostomy successfully diverted the urine leak. A Boari flap ureteroneocystostomy was performed via a lower midline incision with a covering ureteric stent six weeks later. A MAG3 scan was performed six weeks after the ureteric stent had been removed which showed equal split function with good drainage bilaterally.
Learning points
- Ureteric injuries can present with non-specific symptoms.
- A pleural peritoneal fistula is rare.
- Delayed ureteric reconstruction is the preferred surgical option when patients present late.
Case 2
A systemically well 50-year-old male who had a cystoprostatectomy and ileal conduit formation for severe urethral 17 years prior presented with recurrent E coli urinary tract infections and acute kidney injury. A CT revealed severe bilateral hydronephrosis and hydroureter with two large distal right ureteric stones (total length 2.5cm, HU 1000 units) and multiple stones (largest 12mm with combined length of 4.5cm, HU 600) in his conduit which were obstructing his left ureter (Figure 2.). A recent MAG 3 scan revealed equal split function with sluggish drainage but no obstruction.
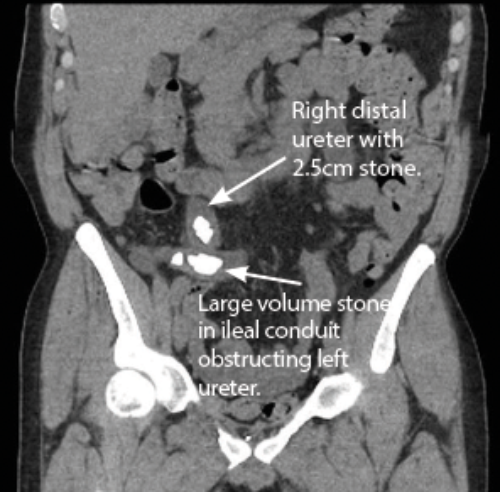
Figure 2.
Bilateral nephrostomy tubes were placed and the renal function improved. Antegrade stents were placed but the right stent dislodged into the conduit requiring removal under fluoroscopy and the left stent failed to drain.
Management options
An enormous prolapsing conduit with approximately 15cm of conduit outside the abdomen represents one of the most complex cases the author has encountered.
- Good governance requires a second opinion from an equally experienced surgeon, which has been sought.
- The length of both ureter and conduit will adversely affect access to the uretero-ileal junction. A staged approach to the conduit stone followed by a rendezvous procedure for the ureteric stones is the proposed treatment modality.
- Informed consent stressing the risk of failures, is key to such ‘once in a lifetime’ cases.




