See Part 2 on this topic here
Case 1
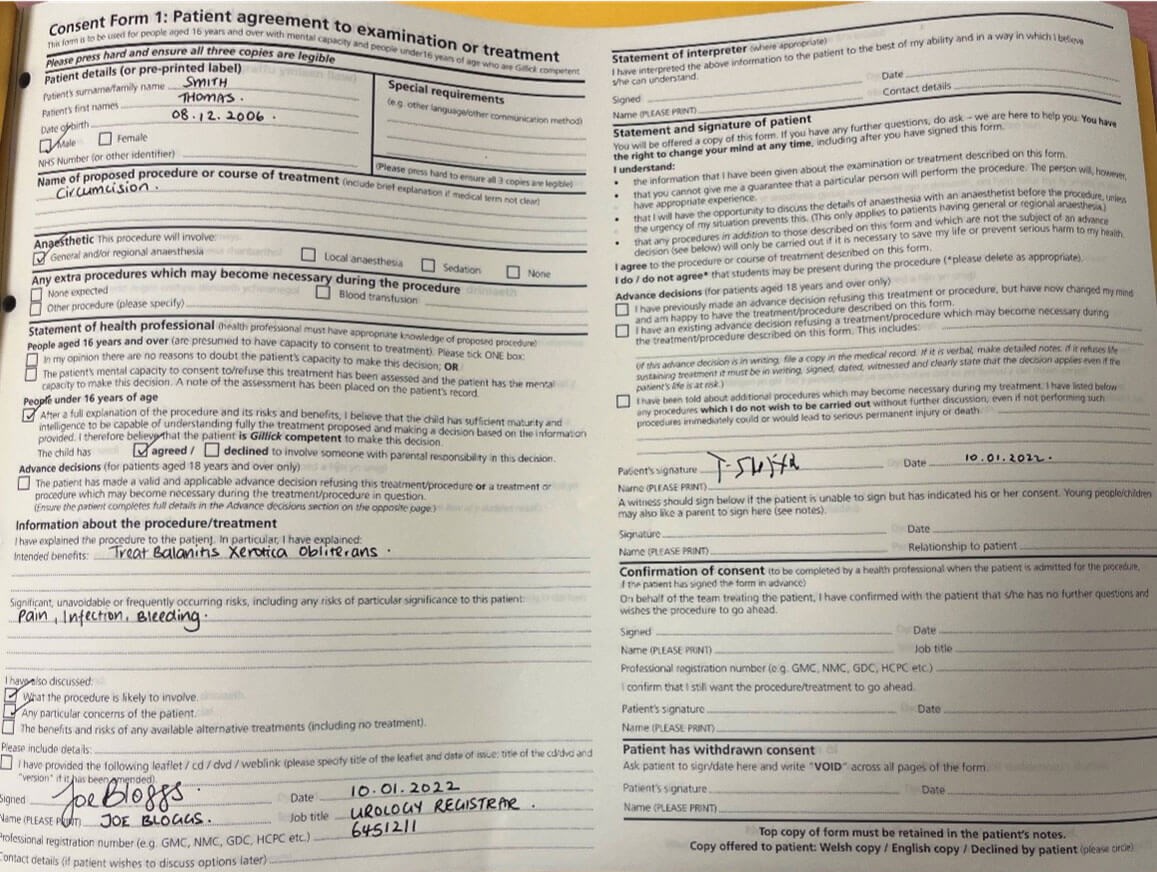
A 15-year-old boy attends with his father to have a circumcision on a day case list. He had been seen previously by a colleague and noted to have a tight phimosis with signs suggestive of balanitis xerotica obliterans (BXO). You have been asked to check the consent form with the patient, which was previously completed with your colleague in clinic.
- What information is missing from the consent form for this procedure?
- Which risks for this procedure are listed on the British Association of Urological Surgeons (BAUS) patient information leaflet?
- In addition to the consent form, what other information is recommended as part of the consent process?
Case 2
The child’s father then says that he is not happy for his son to have the surgery as he recalls having a circumcision for religious reasons as a child which was very traumatic with complications which he would not want his son to have.

Device A.

Device B.
- Can you identify device A and B used in circumcision?
- How do these techniques differ from standard circumcision?
- Can you proceed with the circumcision if the 15-year-old boy consents for the procedure but his father does not?
Consent: answers
Case 1
1. There are a number of missing items from the consent form:
a. Frequently occurring risks are not all mentioned on the consent form.
b. Guidelines for consent also advise that a procedural information leaflet be provided to the patient and allow them time to consider their decision.
c. In this case, as the boy is 15 years old and has agreed for their parents to consent, they can also sign as a witness beneath the patient’s signature.
2. Risks associated with circumcision (as per BAUS):
- Swelling of penis lasting a few days (100%).
- Increased sensitivity to the head of penis lasting up to two weeks (>75%, almost all patients).
- Altered sensation to glans (>75%, almost all patients).
- Infection (1-2%).
- Bleeding (1-2%).
- Dissatisfaction with cosmetic result (1‑2%).
- Oedema of excess skin requiring further surgery and skin removal (1-2%).
- Anaesthetic risk (1-2%).
- May also be beneficial to discuss association with meatal stenosis in BXO.
3. Consent guidelines recommend clear documentation of the consent discussion with the patient and their parent in addition to the consent form being signed.
Case 2
1. Device A: Plastibell; Device B: Gomco clamp.
2a. Plastibell: a single-use disposable plastic device, mainly used to circumcise infants. The plastic ring placed under the foreskin is secured with a ligature around the circumference for haemostasis, the distal foreskin is then excised around the ring which protects the glans, leaving the ring to fall off after four to seven days. The wound heals by secondary intention in one to two weeks.
2b. Gomco clamp: Most utilised instrument in the USA, Gomco bell is placed over glans at level of corona and foreskin replaced in anatomic position. The ‘crush’ technique is used to crush the foreskin between the bell and base plate. Leaving this in place for five minutes allows for haemostasis to be achieved. The foreskin is then cut away at the base plate, to prevent injury to the glans.
3. Yes, the boy can consent for the procedure without parental consent if he is deemed to be Gillick competent although the legal age for consent is 16 years of age (Section 8, Family Law Reform Act 1965).
Gillick competence was initially established in the Gillick v West Norfolk and Wisbech AHA [1986] case relevant to whether under 16-year-olds should be given contraceptive advice and treatment without parental consent. It allows for children under 16 years of age to be deemed competent to make informed and independent decisions about their health and treatment if they have sufficient maturity and intelligence to understand the nature and implications of that treatment.
However, it is important to ensure clear documentation of the discussion throughout. It may be beneficial to give the patient and their parents more time to discuss. It may be beneficial to see both parents (if possible). If they are still unsure, they may want to seek a second opinion. The ICE acronym (Ideas, Concerns, Expectations) for patient-centred communication is useful to remember: Identify the concerns of the parent, it is likely that with clear communication he will come to an agreement if he understands the risks of not performing the procedure.









