See Part 1 on this topic here
Case 1
A 77 year old lady presents to the Emergency Department confused and generally unwell. She is septic and, on imaging, is found to have a 9mm obstructing right sided proximal ureteric calculi with subsequent right sided hydronephrosis and surrounding fat stranding. The patient does not have capacity. Your consultant decides it is in the patient’s best interests to undergo an emergency insertion of a ureteric stent. They ask you to complete the consent form.
- List the consent forms that we use. Which one is appropriate in this situation and why?
- What is included in a consent form 4?3. How do you assess a patient’s capacity?
Case 2
A 55-year-old male attends the Day Surgical Unit (DSU) to undergo repair of a left sided hydrocoele under a general anaesthetic. You have been asked to go through the consent process with the patient. However, the patient states that he does not want to know anything about what the procedure involves or the potential risks, and would just like to sign the consent form and proceed.
- Define informed consent.
- What should you do in the above situation? Can the patient sign the consent form and undergo the hydrocoele repair?
- What is the Montgomery ruling?
- What is the Bolam test and how is it related to Montgomery?
Consent part 2: answers
Case 1
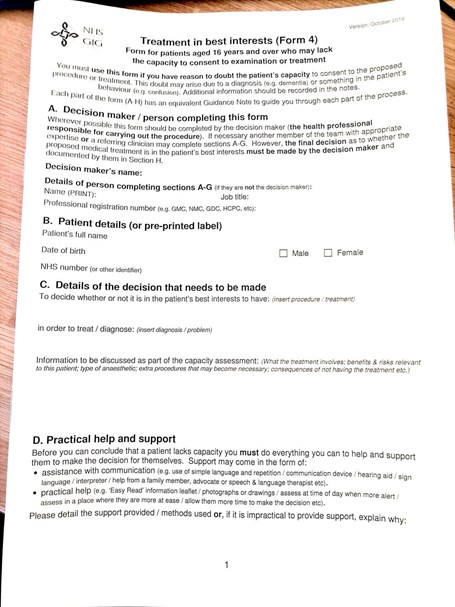
Figure 1.
- Consent form 1 is for patients who are able to consent for themselves. Consent form 2 is for those with parental responsibility consenting on behalf of a child / young person. Consent form 3 is an optional form that is both for patients able to consent for themselves, and for those with parental responsibility consenting for a child / young person where the procedure does not involve any impairment of consciousness. Consent form 4 is for adults who lack capacity to make a decision for treatment.
- In this case, a consent form 4 (Figure 1) is required as the patient does not have capacity for this decision.
- Patient details, name of proposed procedure, assessment of patient’s best interests, assessment of patient’s capacity, information regarding any lasting power of attorney / advance decision regarding treatment, involvement of family / other close people to the patient, if an independent mental capacity advocate is needed, signature of health professional proposing treatment.
- A patient must be able to: understand information relevant to the decision, retain that information, use or weigh up the information as part of a decision, and communicate their decision effectively by any means. Patients should be presumed to have capacity unless it can be established otherwise. Capacity is both time and decision specific. The capacity assessment must be clearly documented in the patient’s notes.
The Mental Capacity Act (2005) is used in England and Wales to assess capacity. The Adults with Incapacity Act (2000) governs assessing capacity in Scottish law. Common law applies with respect to capacity in Northern Ireland.
Case 2
- Informed consent is a process in which patients are provided with important information regarding a treatment / procedure to aid their decision making.
- In this circumstance, you should explain to the patient that they will need to have some information about the procedure before you can proceed, including what the procedure entails, alternative options, and potential risks. If the patient still does not want to hear the information, then the consent may be invalid as the patient has not provided informed consent. You should raise this to the patient’s consultant and clearly document everything in the patient’s notes. You should also consider seeking help from your medical defence body or professional association.
- The Montgomery ruling established that, to consent patients, doctors must ensure patients are aware of any material risks involved in a proposed treatment, and of reasonable alternatives. Material risks are those in which a reasonable person in the patient’s position would attach significance, given their individual circumstances. Background: The case of Montgomery vs. Lanarkshire Health Board. Nadine Montgomery’s son was born with cerebral palsy as a result of shoulder dystocia during birth. Mrs Montgomery had not been warned of the risk of shoulder dystocia, or offered a caesarean section as an alternative, despite being deemed a high-risk pregnancy. Mrs Montgomery claimed for negligence, arguing that she should have been told all the risks. The appeal went to the Supreme Court and the law was passed in 2015.
- The Bolam test is a means of assessing clinical negligence in court; if a doctor acts in accordance with a responsible body of medical opinion, he or she will not be negligent. It was re-examined and reviewed in the 2015 Supreme Court decision of Montgomery vs. Lanarkshire Health Board where it was deemed not to apply in consent cases.










