There has been so much recent discussion and so much emphasis placed on the fundamental right that we all have to determine what is or is not done to us, the right to self-determination, that it would be either a very brave or a very foolish surgeon who nowadays approached consent in a perfunctory fashion.
For a surgeon to be reprimanded by a judge for failing to respect that fundamental right of self determination would, I think, represent a special kind of negligence because it would be an indication that the surgeon was swimming against the tide of public opinion, regulatory opinion (the General Medical Council) and judicial opinion. To fall below the standard of care in a standard negligence case is one thing (which we will probably all do once in a career), but to infringe the expectations of the public or the obligations laid down by the GMC and judiciary would indicate that a surgeon was seriously out of touch. Questions relating to fitness to practice might then follow.
With that in mind, surgeons must have a clear understanding of their obligations under the law of consent as it currently stands. The history of the law of consent places this obligation in context so allowing the surgeon to understand how and why he or she should approach consent in the modern, post-Montgomery era.
The recent Supreme Court judgment in Montgomery v Lanarkshire [1] is seen by some as representing a fundamental shift in the law of consent, but it should be regarded more as the end of a process of evolution, which began in 1985 with the Sidaway case [2].
The judgment in Montgomery v Lanarkshire endorsed GMC guidance on consent, which has for years advised an approach tailored to the individual patient’s circumstances, as indeed has the case law upon which our obligations are founded.
As far back as 2008, the GMC document Consent: patients and doctors making decisions together emphasised the right to self-determination – “The doctor explains the options to the patient…The patient weighs up the potential benefits, risks and burdens of the various options…The patient decides [my emphasis] whether to accept any of the options and, if so, which one.”
The approach to consent that Montgomery now obliges, and indeed which we have been obliged for some considerable time by the GMC to undertake, is one with which urologists are not unfamiliar. As a profession we have accepted for many years that we have a duty to inform men undergoing a vasectomy that there is a 1 in 2000-3000 risk of pregnancy. We have been cognisant that pregnancy is a material risk for a man requesting a vasectomy. The consequences of a failed vasectomy are obvious to most couples and so it is not difficult for the consenting surgeon to talk in terms not only of the frequency of the event (the percentage risk), but also in terms of the implications of such an eventuality for the individual man or couple. What Montgomery does is to emphasise the importance of discussing the implications of a certain risk materialising and to focus the process of consent on the individual patient’s concerns.
The move away from the Bolam test, the so-called professional standard of consent (doctors deciding what patients should be told) towards the approach enshrined in Montgomery (patients deciding what patients should be told) really started with Sidaway v Board of Governors of the Bethlem Royal and the Maudsley Hospital. Mrs Sidaway became permanently paralysed following a laminectomy for nerve root compression. She alleged that, had she been warned of the <1% risk of spinal cord damage, she would not have undergone the procedure. The majority of the Law Lords endorsed the Bolam test, that while some neurosurgeons warned of the risk of spinal cord damage, many did not, the many representing a responsible body of opinion. Mrs Sidaway lost her case.
At appeal in the House of Lords, in a famous dissenting judgment that was ahead of its time, Lord Scarman rejected current medical practice in favour of the patient’s right to know. In so doing he laid the foundations for the rejection of the Bolam test. In Lord Scarman’s view, a doctor would be liable “where the risk is such that in the court’s view a prudent person in the patient’s situation would have regarded it as significant”. Sidaway was really the first time that the courts considered the concept of the opinion of the ‘reasonable patient’ holding sway over the ‘reasonable doctor’. Sidaway explicitly stated that it was open to the courts to decide that information about a particular risk was so obviously necessary that it would be negligent not to provide it, even if a ‘responsible body’ of medical opinion would not have done so.
The requirement for advice and warnings based on the individual patient’s unique circumstances developed further in an Australian case Rogers v Whittaker [3], which followed seven years after Sidaway. Mrs Rogers was blind in one eye. She underwent a non-essential procedure to this blind eye. An ophthalmic surgeon failed to disclose a 1 in 14,000 chance of blindness in the contralateral eye (through sympathetic othalmoplegia, an auto-immune reaction), although Mrs Rogers had expressed specific concerns about losing her residual sight. The expert medical evidence was that the risk was so small that most surgeons would not warn of it. The High Court of Australia disagreed and judged the surgeon negligent for failing to warn.
Rogers v Whittaker and Sidaway demonstrated that it is not just the percentage chance that the risk will occur that matters, but rather the nature of the risk and, more specifically, the impact that it will have on the individual. Rogers v Whittaker also clearly showed that the rarity of an event does not absolve a doctor from an obligation to inform (urologists have accepted that for a long time; post-vasectomy pregnancy being the obvious example, as noted above).
For us Rogers v Whittaker raises an interesting question. Fournier’s gangrene after elective circumcision can only be described as extremely rare. We have had one case in Oxford in something like 30 years. Galukande and colleagues from Uganda estimate the risk to be 1 in 50,000 circumcisions [4]. Should we now warn of the possibility, albeit very rare, of such a risk? BAUS, the professional standard, advises not. But who would argue that the consequences are not life changing for the individual concerned assuming he survives? Would a judge be more sympathetic to the claimant, post-Montgomery, than to a defendant urologist? I don’t know the answer. I am simply posing the question as food for thought.
For my own part I do now warn of this risk telling patients something like “once in 30 years, amongst many thousands of circumcisions, we have encountered just one case of a severe infection of the skin of the penis, scrotum and lower abdomen. The risk is estimated to be 1 in 50,000 so it is very rare. Such infection would necessitate removal of a substantial quantity of skin, over several operations, probably with an ITU admission of a week or longer, and then subsequent plastic surgery to reconstruct the genitals. Fournier’s gangrene is life-threatening with a death rate of 30%. Let me re-emphasise that the chances of this occurring are very rare at just 1 in 50,000 men.” Is this overkill or consistent with a Montgomery-style consent? I’ll leave you to think about it.
By the end of the 1990s, judges were by now fast approaching the reasonable patient test as the dominant force in consent. In Pearce v United Bristol Healthcare NHS Trust [5] Mrs Pearce was not warned of a small risk of still-birth if she went over term. Lord Woolf, Master of the Rolls (the most senior civil judge in England) concluded:
“In a case where it is being alleged that a plaintiff (claimant) has been deprived of the opportunity to make a proper decision as to what course he or she should take in relation to treatment, it seems to me to be the law…..that if there is a significant risk which would affect the judgment of a reasonable patient, then…..it is the responsibility of a doctor to inform the patient of that significant risk.”
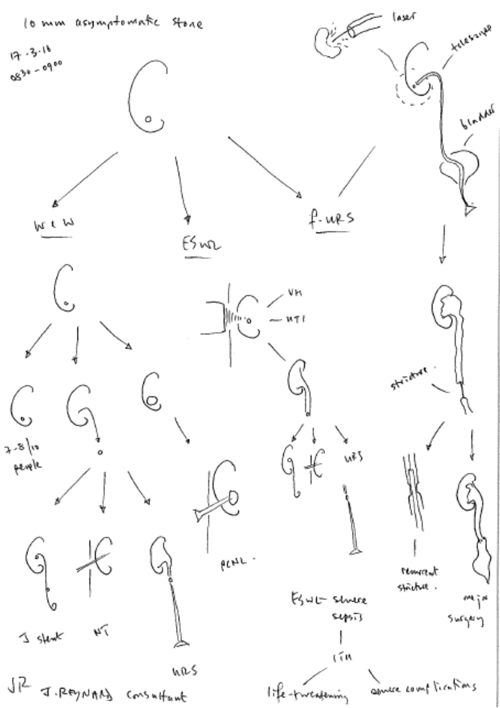
Figure 1: A Reynard-o-gram for discussions of management options
for a small asymptomatic renal stone (Copyright John Reynard).
Montgomery represents the final word in the evolution of the reasonable patient test, summarising as it does current judicial thinking on disclosure and I would strongly advise that urologists take heed of the following paragraphs in that judgment:
- Para 89 – “the assessment of whether a risk is material cannot be reduced to percentages [my emphasis]. The significance of a given risk is likely to reflect a variety of factors besides its magnitude: for example, the nature of the risk, the effect which its occurrence would have upon the life of the patient, the importance to the patient of the benefits sought to be achieved by the treatment, the alternatives available, and the risks involved in those alternatives. The assessment is therefore fact-sensitive, and sensitive also to the characteristics of the patient.” This paragraph has led me to conclude that the BAUS consent forms, good though they are (and I applaud BAUS for introducing them before other surgical specialties), are nothing more than a starting point in the process of consent. In my opinion they do not provide adequate evidence in themselves that consent has been obtained, principally because while they discuss percentage risks they do not provide adequate detail of what those risks really mean. A more sophisticated approach is needed.
- Para 90 – “Secondly, the doctor’s advisory role involves dialogue, the aim of which is to ensure that the patient understands the seriousness of her condition, and the anticipated benefits and risks of the proposed treatment and any reasonable alternatives, so that she is then in a position to make an informed decision. This role will only be performed effectively if the information provided is comprehensible [my emphasis]. The doctor’s duty is not therefore fulfilled by bombarding the patient with technical information which she cannot reasonably be expected to grasp, let alone by routinely demanding her signature on a consent form.” I don’t have all the answers, but I would advance the principle of the Reynard-o-gram (Figure 1) to assist the doctor in providing comprehensible information. I would also caution against simply handing patients a BAUS consent form, to read in their own time, especially when this is used as a time-saving substitute to a verbal explanation (again see below for why I think this).
- Para 93 – “even those doctors who have less skill or inclination for communication, or who are more hurried, are obliged to pause and engage in the discussion which the law requires”. Their Lordships are telling us what they think. We should listen.
After 12 years of experience as a medical expert witness, acting both for claimants and defendants, in thousands of cases, I have concluded that it is in the explanation of the significance of a particular complication where so many defendants let themselves down. Most of us (though amazingly not all of us) are pretty good about using the BAUS consent information forms, but as noted above these go only so far. Where many defendants fall down is in explaining what, for example, that 1 in 100 risk (or thereabouts) of a ureteric stricture post-ureteroscopy might really mean. BAUS’s description of “Very rarely, scarring or stricture of the ureter requiring further procedures” may occur, does little to give a patient a genuine understanding of what “further procedures” really means.
We all know that “further procedures” involves something like the following (I have seen several such cases and the claimants were definitely sure that they had not been properly informed of what “further procedures” really meant) – weeks or indeed months of stent symptoms, the admission to hospital with urinary infections, the requirement for several stent changes and for nephrostomy insertion culminating in some cases in the need for ureteric re-implantation or in loss of function in the affected kidney, and then a further admission for a nephrectomy. Not one bit of this will be comfortable; all of it will be painful and distressing. “Further procedures” in no way does justice to the pain and suffering that some patients go through and this seemingly throwaway term only serves to fuel the resentment and add to the grievance that a claimant may feel towards their urologist. And all for the want, many barristers will argue, and many judges will accept, for a genuinely adequate explanation of risks.
Another example is that of TURP (I am not talking about TURBT) and bladder perforation. Consider this – do you warn of the risk of a bladder perforation after a TURP? BAUS say you should be describing: “Very rarely, perforation of the bladder (can occur) requiring a temporary urinary catheter or open surgical repair”. Just an “open surgical repair”. How little those words really mean. They give no sense of the requirement for ITU admission that may follow (common in my medicolegal experience), or indeed the possibility of death (not infrequent in my medicolegal experience of bladder perforation). There cannot be a single patient who would not regard a warning of a possible ITU admission or death as anything but absolutely necessary. There can be few judges, if any, who would not be sympathetic to the claimant’s view (and I know for a fact that the GMC takes a dim view of the failure to warn of the risk of a bladder perforation after a TURP). This then is the essence of Montgomery – giving patients the information they need to decide what will be done to them.
I cannot cover everything there is to consider about consent – books are written on the subject. But I have a few final words of practical advice. The GMC advises that doctors “could consider using a pre-printed checklist and recording that you have discussed everything on it, therefore removing the need to write everything repeatedly. However, if you do this it is important that you consider any other information that may be relevant to that individual patient and show that you have tailored the information based on their needs. It should not be a tick box exercise.”
My approach to consent has evolved over the last 20 years or so. My current approach to documentation of the consent process for ureteroscopic stone removal for example, is to state in a letter addressed directly to the patient (the GP being copied in), something along the lines of: “We went through the BAUS consent information form, line by line and I used language that I think helped you understand the medical jargon. I also supplemented this using a series of diagrams to explain the nature of ureteroscopic stone removal and potential risks of failed access requiring stent insertion and redo-ureteroscopy, ureteric stricture formation and injury and major surgery in the form of ureteric reimplantation. Given the nature of your job I explained that stent symptoms, should they occur, are described by some patients as being so severe that it can be very difficult to work during the period of stent insertion. This would have obvious financial implications for you, as you are self-employed. Hopefully such severe symptoms will not occur, but you should be aware that they can occur. Similarly, if you were to experience a ureteric stricture or injury, that and the major surgery required to correct it could lead to many months off of work. Such complications are fortunately uncommon, but certainly not unheard of.” I am not saying that I have got it right, but it an approach with which I feel comfortable.
The diagrams I use are known affectionately by Oxford urological trainees as ‘Reynard-o-grams’ (I think it is affection, but maybe it’s ridicule). Their main function is to impart genuine understanding on the part of the patient and their relatives, but they serve another important function, that of providing evidence that an effort was made to impart genuine understanding.
I would further advise every surgeon to consider the questions I am now not infrequently posed by claimant solicitors:
- Has the clinician taken full notes documenting the consent process?
- From the notes, does it appear that adequate time has been set aside for a meaningful consent process?
- Is there evidence of a genuine dialogue between the doctor and patient around consent?
- Has the clinician done any more than simply express magnitude of risk by reference to percentages?
- Have the risks of possible distressing, painful or dangerous intervening events been explained to the patient, in addition to the risks of adverse final outcomes?
- Is there any impression of lip service having been paid to the consent process? For example, does it appear that it consisted of the provision of a leaflet and not much more?
For those who think handing the patient the BAUS consent information form is enough, consider this latter point carefully. The readability of NHS information leaflets, websites and the BAUS consent information forms is poor (and this emphasises the beauty of the Reynard-o-gram). Our simple conclusion [6] is that many people do not have the reading skills to understand them, because they are written in ‘Gobbledygook’. We have proven that in our study where we applied the Simple Measure of Gobbledygook (SMOG) to the BAUS forms. Gobbledygook is language that is meaningless or is made unintelligible by excessive use of abstruse technical terms.
We concluded:
- The majority of the leaflets are written above the reading level of an 18-year-old.
- Using national literacy statistics, at least 43% of the population will have significant difficulty understanding the majority of these leaflets.
- Comprehension of the leaflets provided by BAUS is likely to be poor. These leaflets may be used as an adjunct to discussion but it is essential to ensure that all the information necessary to make an informed decision has been conveyed in a way that can be understood by the patient.
Summary
In summary, a patient has a fundamental right to decide whether to undergo a recommended treatment. A doctor has a fundamental obligation (a fundamental duty of care) to make available to the patient sufficient information to enable the patient to reach a balanced judgment. The professional standard of consent (the so-called Bolam test) is dead. Motgomery rules. You have worked hard to become a surgeon. Don’t expose yourself to the threat of litigation or censure by the GMC by failing in that obligation.
References
1. Montgomery (Appellant) v Lanarkshire Health Board (Respondent) 2015 UKSC 11 On appeal from 2013 CSIH 3; [2010] CSIH 104.
2. Sidaway v Board of Governors of the Bethlem Royal and the Maudsley Hospital 1985 1 All ER 643.
3. Rogers v Whittaker 1992 67 ALJR 47.
4. Galukande M, Sekavuga DB, Muganzi A, Coutinho A. Fournier’s gangrene after adult male circumcision. Int J Emerg Medicine 2014;7:37-40.
5. Pearce v United Bristol Healthcare NHS Trust 1999 PIQR P 53.
6. Graham C, Reynard JM, Turney BW. Consent information leaflets – readable or unreadable? J Clin Urol 2015;8:177-82.







