Case 1
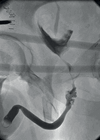
A four-year-old boy presents to clinic following GP referral unable to retract the foreskin (Figure 1).

Figure 1.
- What is the diagnosis?
- The above condition may be pathological or physiological; clinically how can you differentiate this?
- Explain the process of why the foreskin cannot be retracted and how the condition usually self resolves in the physiological variant of the condition.
- What is the cause of the pathological variant?
- How should the pathological variant of the condition be managed compared to the physiological variant?
- If the decision is made to offer a circumcision, what are the risks parents should be informed of ?
Case 2
You are called to the emergency department to assess an 11-year-old boy with a 24-hour history of right sided scrotal pain and swelling. On examination you note a blue tender lump at the upper pole of the testes (in the region shown on Figure 2).

Figure 2.
- Given the history, what are the differential diagnoses?
- The description above would classically represent what?
- What is the hydatid of Morgagni?
- How would you manage this case?
- As you are in the department a colleague asks you to review a six-month-old boy whose mother is very concerned about a diffuse, non-tender, fluctuant and transilluminating swelling in a hemiscrotum. Given the brief history you have what is the most likely diagnosis and what would be your management plan?
Acknowledgements
Figure 1: Reprinted from Hayashi Y, Kojima Y, Mizuno K, Kohri K. Prepuce: phimosis, paraphimosis, and circumcision. Scientific World Journal 2011;11:289‐301.
Figure 2: Reprinted from Pomajzl AJ, Leslie SW. Appendix Testes Torsion (Updated 6 Nov 2019). In: StatPearls [Internet]. Treasure Island (FL), USA; StatPearls Publishing; 2020.
Both figures have been used under the terms of the Creative Commons Attribution 4.0 International Licence allowing free use and reproduction as long as sources are correctly cited from original content
(http://creativecommons.org/licenses/by/4.0/).
Spot Test: answers
Case 1
- Balanitis xerotica obliterans (BXO).
- In a physiological phimosis, when you attempt to retract the foreskin the inner mucosa of the foreskin pouts through the preputial opening, looking a little like a flower. When a similar attempt is made in BXO, the pouting does not occur and a characteristic thickened, scarred white ring can be seen at the preputial opening as shown in Figure 1. In physiological phimosis, the foreskin is mobile around the glans meatus, whereas in severe BXO, it may be adherent.
- The preputial opening is very narrow and there are adhesions between the glans and the inner prepuce. With time, the adhesions separate and the foreskin meatus loosens, to allow it to glide over the glans. The foreskin must never be forcibly retracted as this may tear the foreskin and glans.
- BXO is a chronic skin condition akin to lichen sclerosis, with evidence suggestive of an autoimmune pathology.
- BXO requires circumcision whereas physiological phimosis can safely be managed conservatively with parental advice on bathing and proper foreskin hygiene, steroid creams can be used for physiological phimosis which is slow to release.
- The overall risk is relatively low but parents should be made aware of the following: infection, bleeding (which in rare cases may require a further procedure), meatal stenosis, cosmetic dissatisfaction, altered sensation to the glans of the penis and anaesthetic risks. BXO can affect the glans (pale appearance) and less commonly, the urethra, which causes urethral stricture; this is of course an outcome of the underlying condition, rather than the circumcision procedure.
Case 2
- Differential diagnosis: testicular torsion, torsion of the hydatid of Morgagni.
- The blue spot is a classical sign of torsion of the hydatid of Morgagni, representing the ischaemic / necrotic appendix testis.
- The hydatid Morgagni is one of the regressed Mullerian (female) embryological remnants found on the upper pole of the testes and epididymis.
- If there is any concern that a diagnosis of testicular torsion cannot be excluded, the child should undergo a surgical exploration. If there are no concerns, the child can be conservatively managed with anti-inflammatory medication. Rarely, pain persists beyond seven days, at which point surgery to remove the hydatid can be offered. Be aware of the medico-legal implications of this and ensure that the parents are counselled well and this is documented.
- This case is a textbook history of an infantile hydrocoele which should spontaneously resolve within 18 months as the patent processus vaginalis closes. Observation of the child for the first year of life would be appropriate, however surgical repair may be required if it does not self-resolve. Be aware of a hernia - in young children, a herniated loop of bowel can transilluminate!