Case 1
A fit and well 50-year-old gentleman presents to the emergency department with pain and swelling of his penis that started a few hours after he had a shower earlier in the day. On examination, the appearance is as below (Figure 1).
- Identify the pathology in Figure 1.
- Describe this pathology.
- What is the mechanism of injury?
- Describe the structure of the penile shaft.
Case 2
An uncircumcised 65-year-old was catheterised 12 hours previously on the orthopaedic ward for urinary retention after a hemiarthroplasty. The urology team have been asked to see him as his foreskin was not returned to normal position after catheterisation and he has a swollen and very painful glans surrounded by a tight oedematous foreskin at the base.
- What are complications of this pathology?
- What are treatment options?
- What is the prognosis?
Answers: Nuptial night tragedy
Case 1
1. Paraphimosis. Other differentials include:
- Acute angioedema
- Balanitis
- Penile fracture / haematoma
- Foreign body tourniquet
- Penile carcinoma
2. Paraphimosis is the inability to return a retracted foreskin. Colloquially referred to as the nuptial night tragedy, it describes entrapment of a tight foreskin proximal to the corona of the glans penis.
3. This condition only occurs in partially or uncircumcised individuals wherein the foreskin is retracted for several reasons (e.g. cleaning, during intercourse, or iatrogenic processes like catheterisation or cystoscopy) and is not replaced. The glans engorges and the foreskin becomes oedematous due to venous and lymphatic congestion. Subsequently, the foreskin forms a tighter ring causing severe pain and eventual ischaemia.
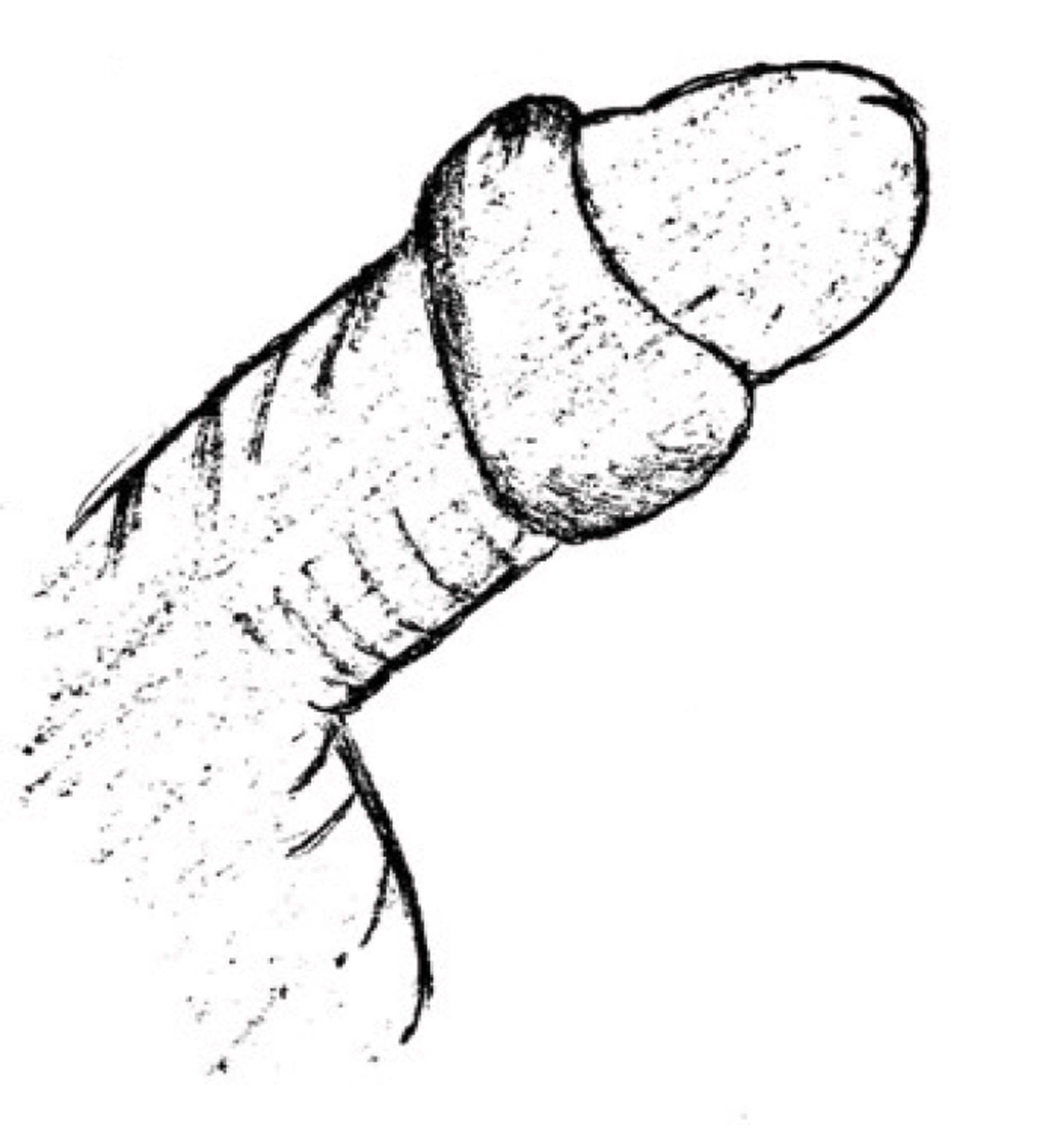
4. The penile shaft is divided into three parts:
- Root: this part lies under the pubic bone and provides stability when the penis is erect (Figure 2a).
- Body: this is composed of two cavernosal bodies (i.e. corpora cavernosa) and a corpus spongiosum (i.e. head of the penis). The male urethra traverses the corpus spongiosum and exits from the meatus (Figures 2a and 2b).
- Glans: this is the distal expansion of the corpus spongiosum usually covered by the loose skin of the foreskin in uncircumcised individuals (Figure 2a).

Figure 2a: Penile anatomy.
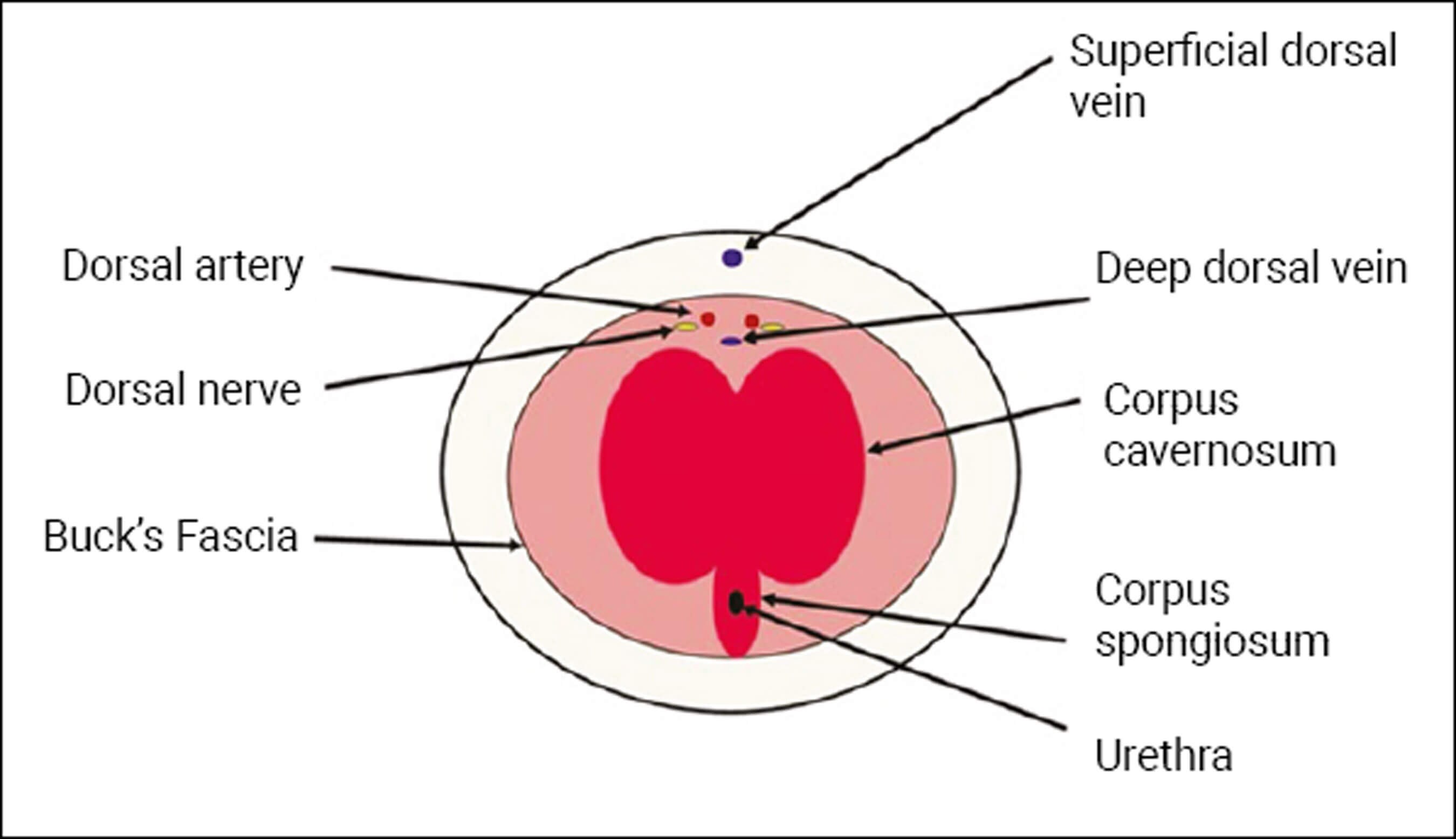
Figure 2b: Cross section of penile shaft.
Case 2
1. Complications include:
- Pain
- Posthitis
- Recurrence
- Necrosis and gangrene
- Autoamputation
2. Pain management is important in the treatment of paraphimosis. Adequate analgesia and / or local anaesthesia can be achieved by a dorsal penile nerve block, penile ring block, or a combination. Local anaesthetic agents with adrenaline should not be used as this could lead to penile necrosis.
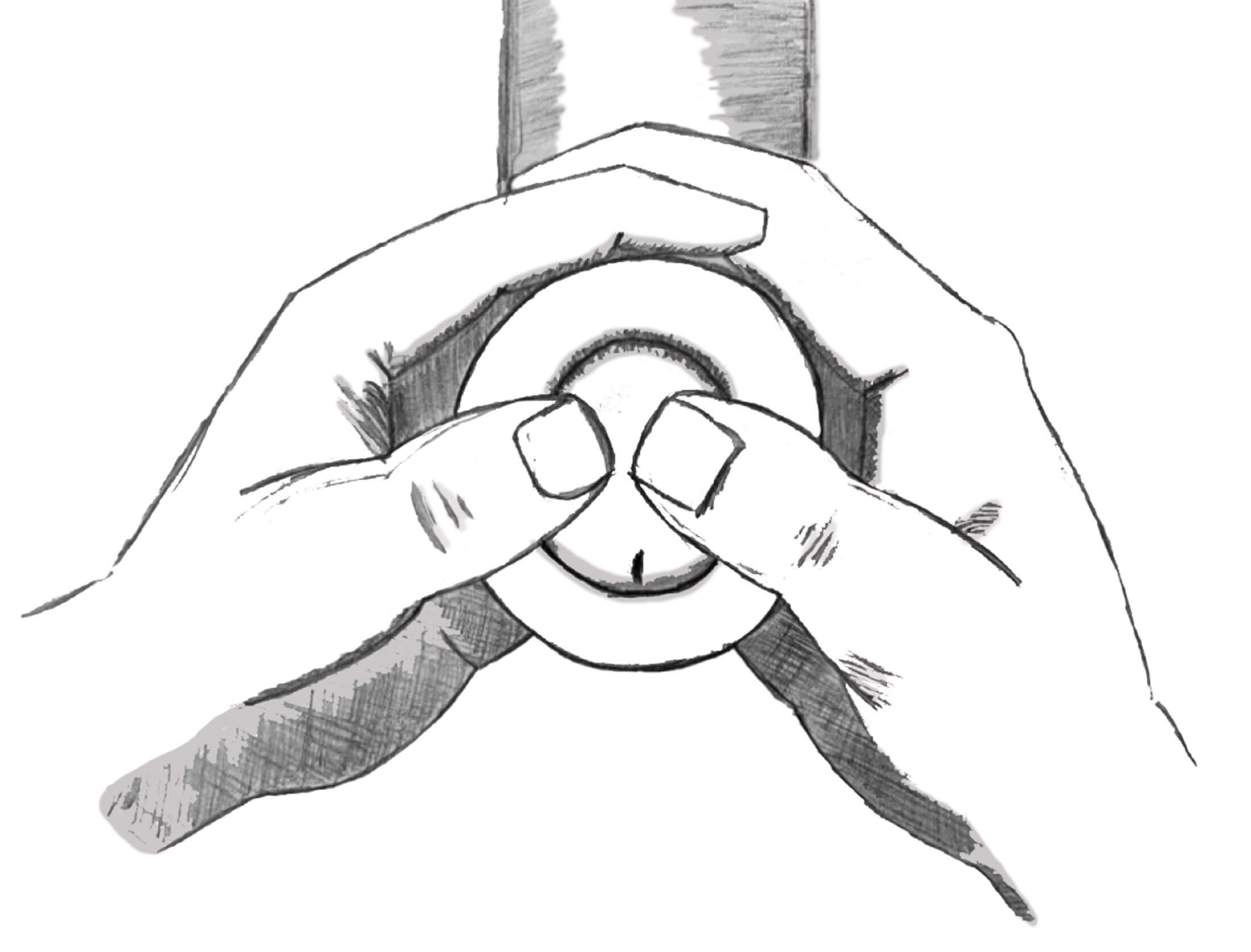
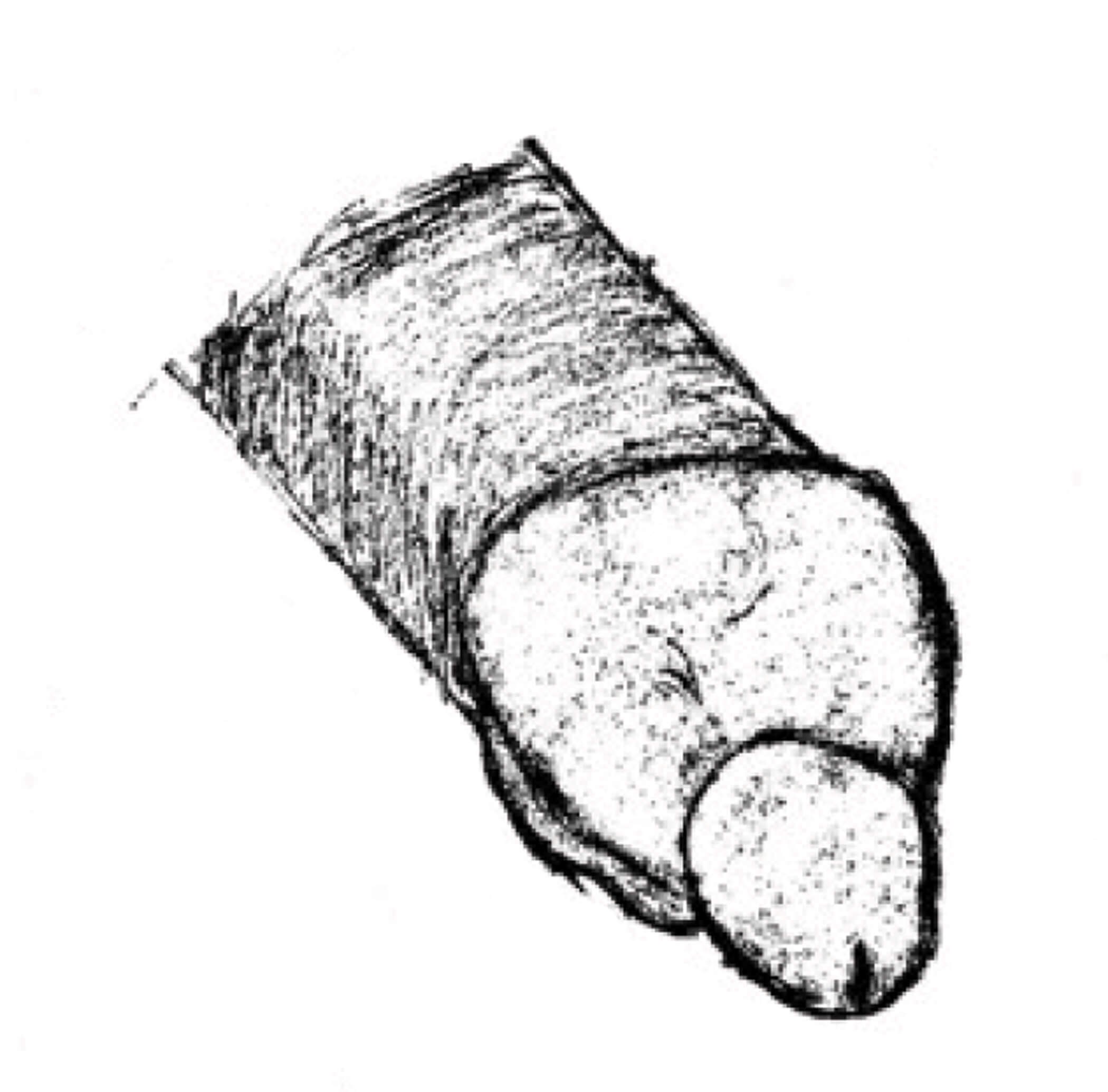
Figure 3: Manual reduction of paraphimosis.
Manual reduction: This can be achieved by traction on the foreskin and countertraction on the glans. Reduction is achieved by circumferentially compressing the foreskin and holding for two to ten minutes to push the oedematous fluid along the penile shaft proximally. After this, the foreskin is reduced by placing both thumbs on the glans and using the remaining fingers to pull the foreskin back over the glans (Figure 3). Instruments like forceps and clamps can be used in the reduction of paraphimosis, however, these must be used cautiously as they can crush the skin leading to necrosis.
Dorsal slit: This surgical technique for reducing paraphimosis is described below. A haemostat is applied at 11 and 1 o’clock positions on the dorsal foreskin up to the coronal sulcus. An incision is made at the 12 o’clock position (Figure 4a) whilst avoiding the penile skin.
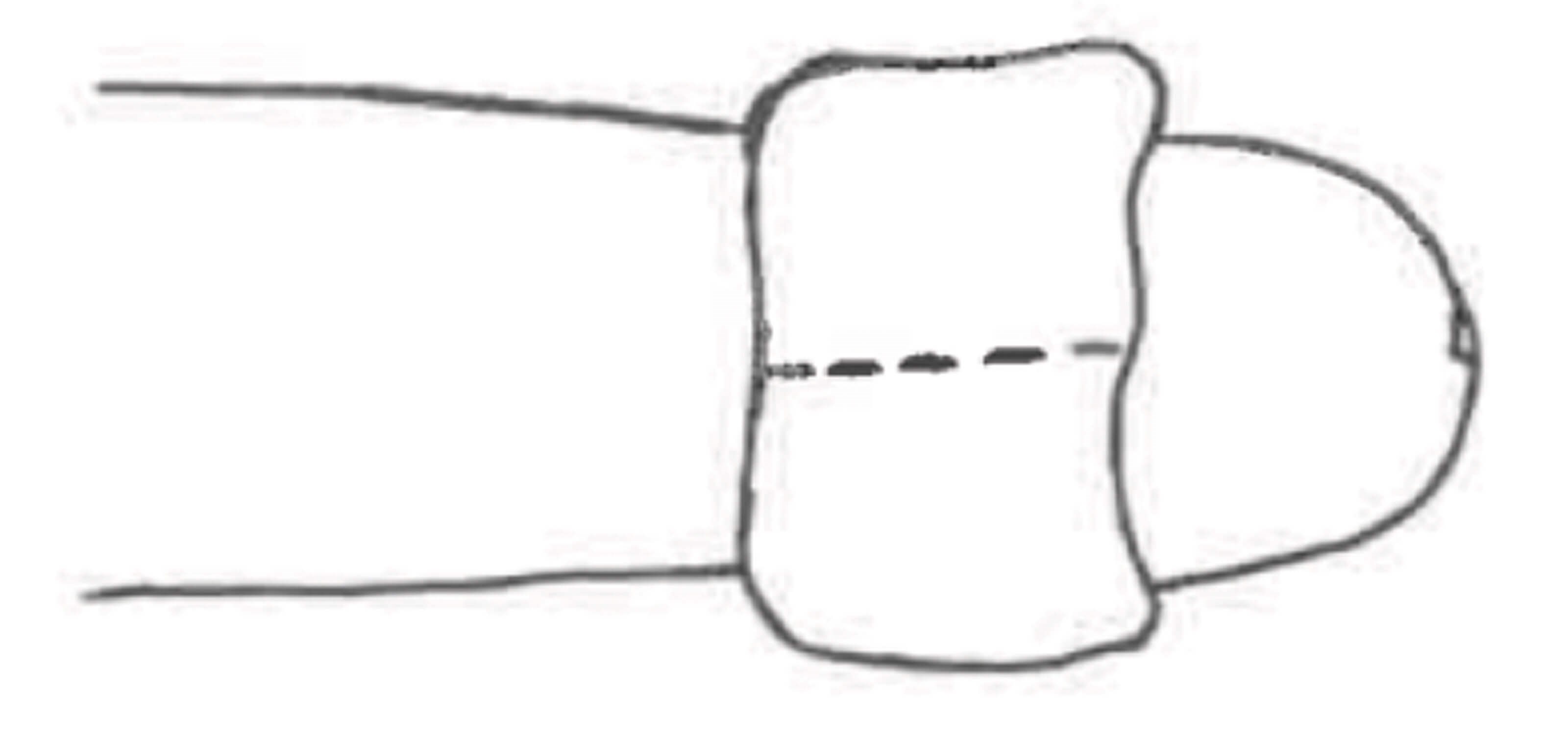
Figure 4a: Incision at 12 o’clock position.
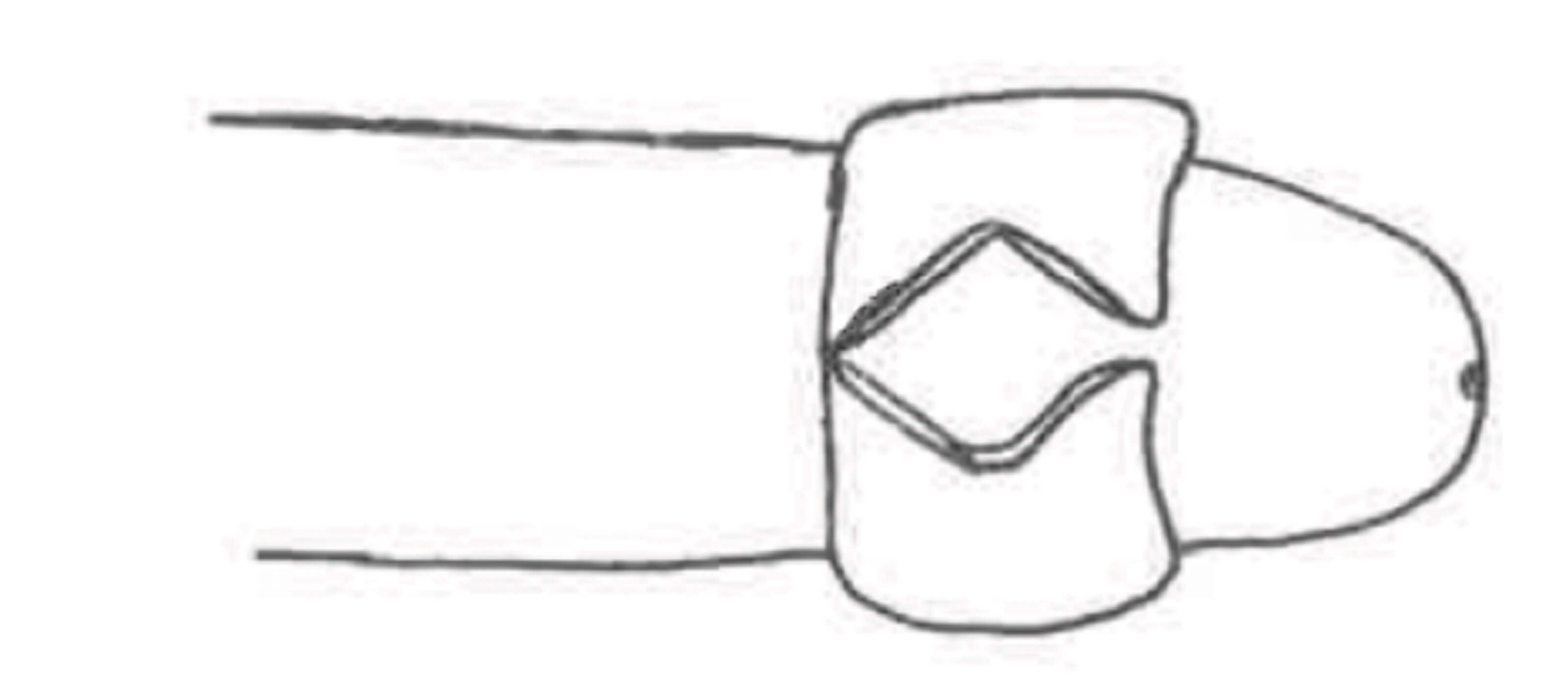
Figure 4b: Diamond shaped opening of incision.
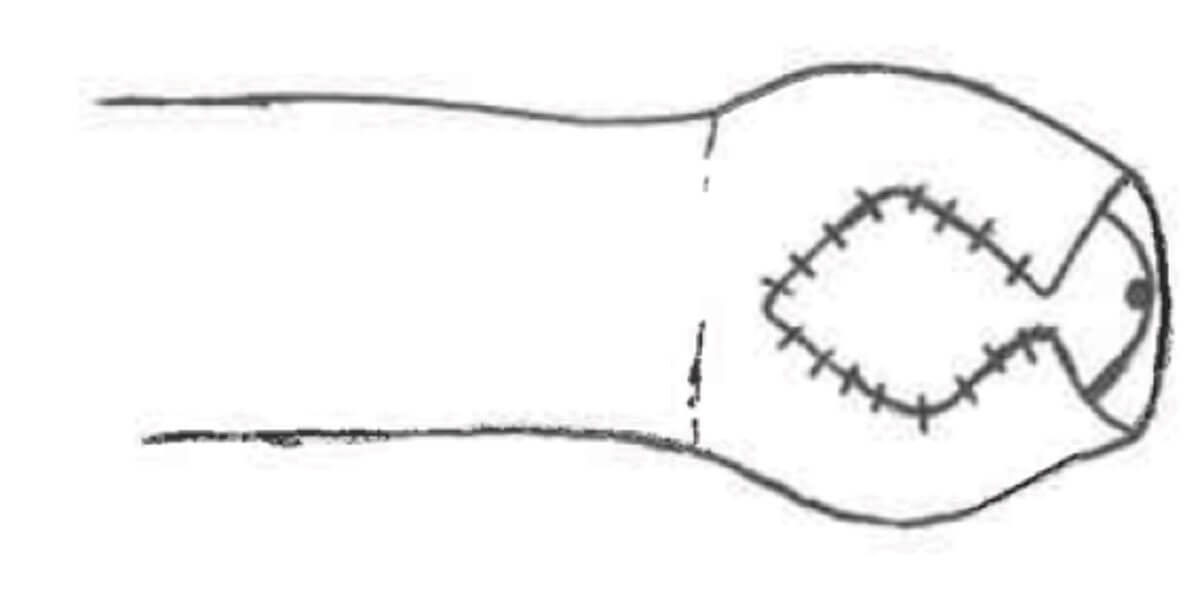
Figure 4c: Apposing ipsilateral edges of incision.
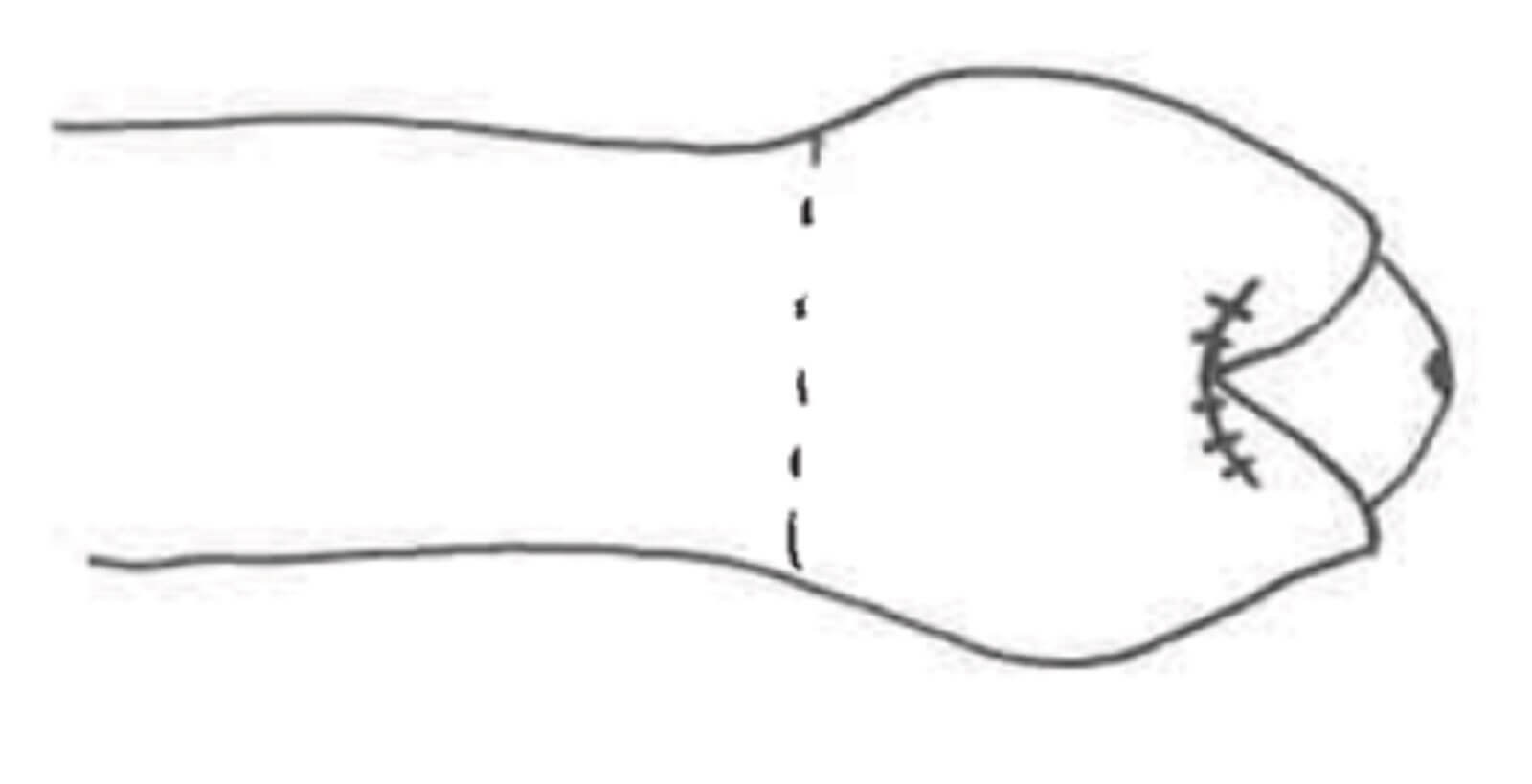
Figure 4d: Apposed edges of foreskin.
Following the vertical incision, the edges of the foreskin open like a diamond shape (Figure 4b). Remove the haemostat to allow drainage of oedema for a few minutes then approximate the edges of the diamond on ipsilateral sides with absorbable suture (Figure 4c). Successful apposition of the slit will leave a gap at 12 o’clock position (Figure 4d), then attempt manual reduction as described above.
3. The prognosis with paraphimosis is excellent if diagnosed and treated promptly. There may be some bleeding during skin retraction, but long-term negative outcomes are rare. Paraphimosis can commonly recur however, circumcision can preclude recurrence. An alternative to a circumcision, especially in older or sicker patients, would be a dorsal slit. Either is satisfactory in preventing a recurrence.
Further reading
1. Bragg BN, Kong EL, Leslie SW. Paraphimosis. StatPearls [Internet] 2022
https://www.ncbi.nlm.nih.gov/
books/NBK459233/
2. Choe JM. Paraphimosis: Current Treatment Options. American Family Physician 2000;62(12):2623-6.
3. Shlamovitz GZ, Snyder EW. Dorsal Slit of the Foreskin: Overview, Indications, Contraindications. MedScape 2018
https://emedicine.medscape.com/
article/80697-overview#a3
4. Brooks NA, Brown JA. Paraphimosis: Practice Essentials, Relevant Anatomy, Pathophysiology. MedScape 2021
https://emedicine.medscape.com/
article/442883-overview
5. Raveenthiran V. ‘Paraphimosis’ In: Baky Fahmy MA. Normal and Abnormal Prepuce. Springer Nature; Switzerland; 2020.
[All links last accessed June 2022].