Case 1
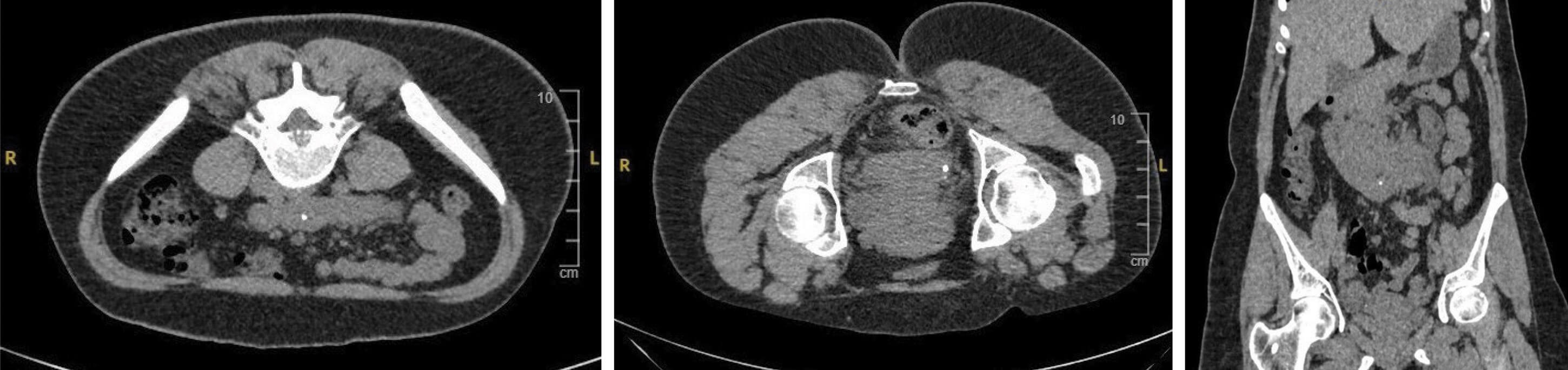
Figure 1.
- A 26-year-old female presents to A&E with loin pain. What do the CT images in Figures 1 (left, centre and right) show?
- What is the prevalence of the congenital anomaly in the general population, and is either sex more prone to it?
- What other similar anomalies are described?
- Are there any risk factors for this anomaly?
- What are the most common complications from this anomaly?
- The patient has persistent pain and is unable to return to work. How should this be managed?
- Could such a kidney be used for transplant?
Case 2
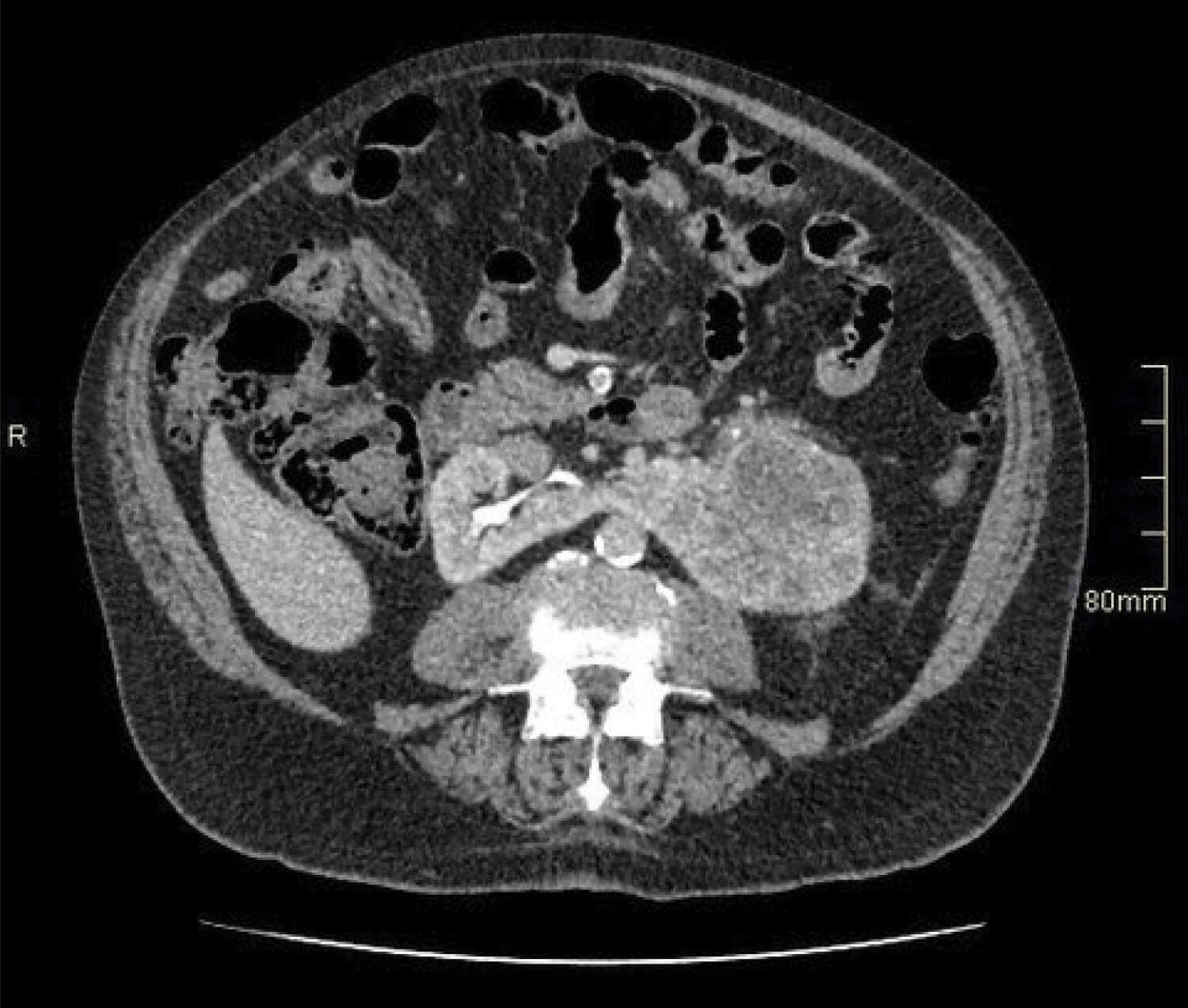
Figure 2.
- An 82-year-old man presents with visible haematuria. Flexible cystoscopy is normal, but what does the contrast CT image in Figure 2 show?
- What stage could the lesion be?
- How does the congenital anomaly influence risk of malignancy?
- What other types of imaging may be useful prior to multidisciplinary team (MDT) discussion?
- What is the likely surgical management of this lesion?
- Final histology shows a 10cm clear cell renal cell carcinoma (RCC) with invasion of renal sinus fat, nodal status undetermined, no necrosis but rhabdoid change therefore graded International Society of Urological Pathology (ISUP) G4. What tumour, node and metastasis (TNM) stage and 2003 Leibovich risk score would this be?
Case 3
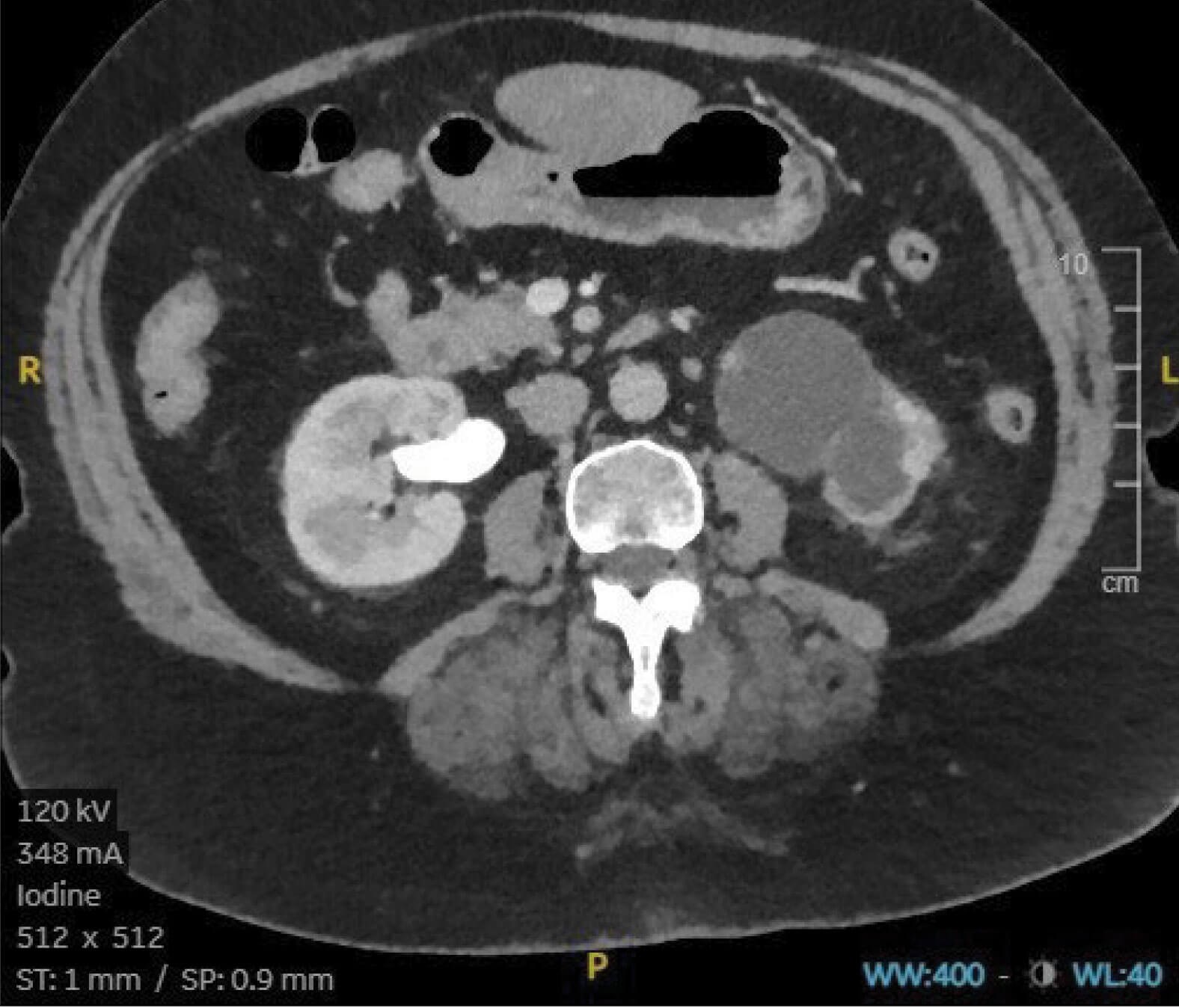
Figure 3.
- A 74-year-old female is noted on annual review to have a deterioration in her renal function. Following an ultrasound scan, a CT intravenous urogram (IVU) is performed, showing no hydroureter on either side, but what does Figure 3 show?
- A subsequent MAG-3 renogram confirms obstruction with 10% split function on the affected side. What are the congenital causes of this abnormality?
- At what age is this usually diagnosed, and is one side more commonly affected by this abnormality?
- How do patients commonly present and how is this different in adult vs. paediatric populations
Upper tract abnormalities - Answers
Case 1
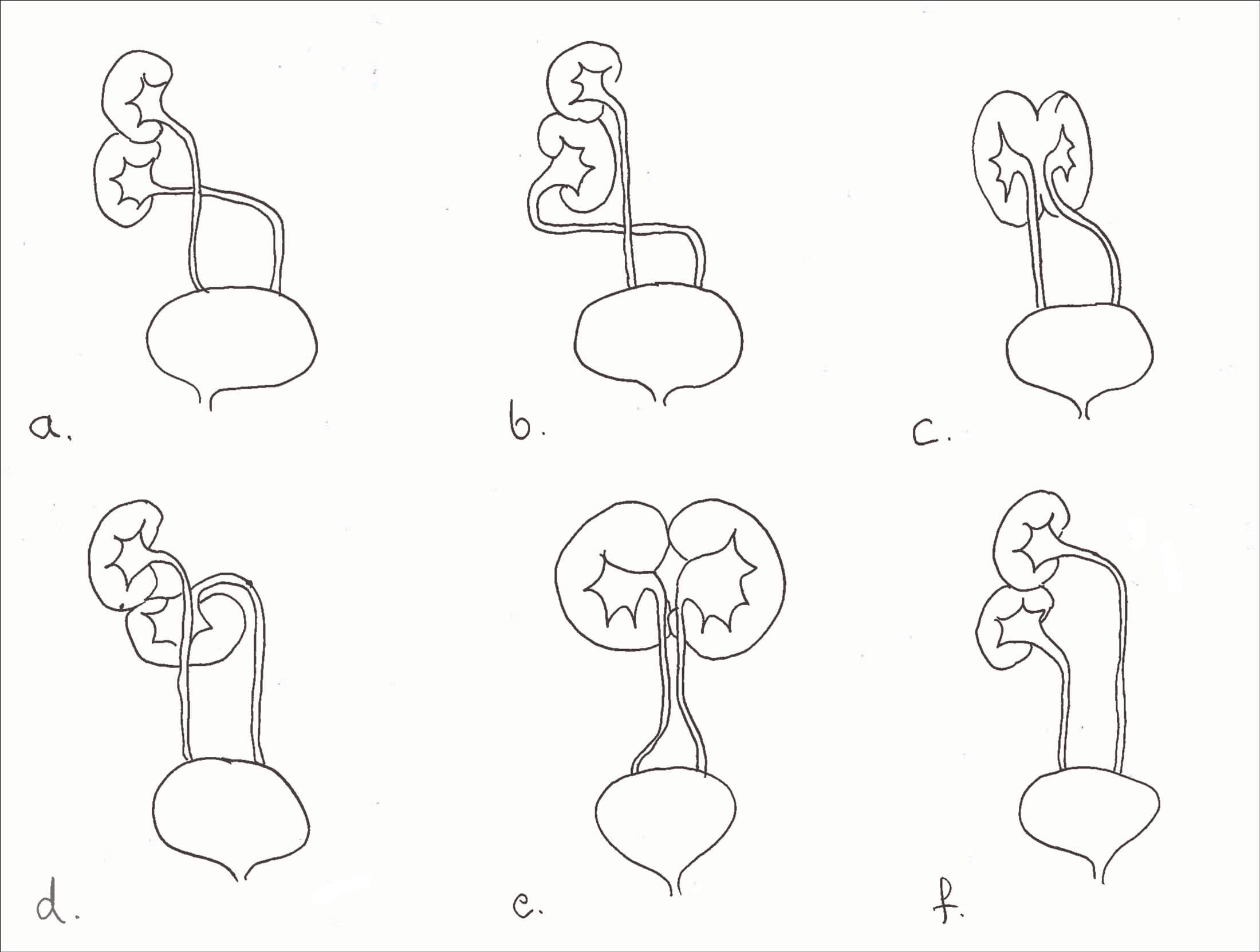
Figure 4.
- Horseshoe kidney with a small stone in the renal pelvis and a ureteric stone.
- Horseshoe kidney has a population prevalence of 0.25%, being twice as common in men [1].
- Other fusion defects include a) unilateral fused kidney with inferior ectopia, b) S-shaped kidney, c) lump kidney, d) L-shaped kidney, e) disc kidney, and f) unilateral fused kidney with superior ectopia (Figure 4) [2].
- Teratogens such as thalidomide, alcohol and poor glycaemic control increase the risk, incidence is higher in chromosomal anomalies such as Edwards syndrome, Turner’s syndrome and Down’s syndrome and cases are described in identical twins as well as several siblings within a family [3].
- The three most common pathologies are pelviureteric junction (PUJ) obstruction, stones and infection, while an increased incidence of injury in trauma is noted, as well as an increased risk of malignancies. Note that 30% remain asymptomatic and uncomplicated [3].
- Extracorporeal shockwave lithotripsy (ESWL) is known to be less effective in horseshoe kidneys due to problems localising the energy and poor drainage for fragment clearance [4]. Ureteroscopy and laser lithotripsy would be justifiable first-line treatment.
- There are two ways to transplant a horseshoe-shaped kidney – divide and transplant separately or transplant en bloc [5].
Case 2
- The image shows an 8cm tumour in the left moiety of a horseshoe kidney.
- This tumour is T2a at least given the size visible here: further images would reveal invasion of the renal vein, T3a.
- Horseshoe kidney is associated with an increased risk of renal malignancies including renal cell carcinoma, transitional cell carcinoma (three times), Wilm’s tumour (twice as likely) and an extremely large increase in very rare tumours such as Carcinoid (62 to 82 times) [3]. Horseshoe kidneys are rarely associated with PKD, with fewer than 20 cases reported: the risk of having both is estimated to be 1:8,000,000 [6].
- Imaging with arterial phase contrast is useful prior to surgery for renal tumours, to detect relevant vascular anomalies – which are more common in horseshoe kidney. It is also useful to assess renal function in the unaffected moiety, for which a DMSA scan would be ideal [1,2].
- A heminephrectomy is the definitive surgical management for a tumour of this size in a horseshoe kidney.6. T3a, Nx, Mx, and Leibovich score 8 (high risk) [7].
Case 3
- A hydronephrotic left kidney with minimal renal cortex and no excretion of contrast into the collection system. Right kidney appears normal.
- Fifty percent of cases of congenital PUJ obstruction are the result of a crossing accessory renal vessel causing extrinsic obstruction of the proximal ureter. Other causes include ureteral hypoplasia with abnormal peristalsis preventing adequate drainage and high insertion of the ureter into the renal pelvis [8].
- PUJ obstruction is most commonly seen in the paediatric population, the left side being more commonly affected than the right [8].
- Hydronephrosis is commonly detected antenatally and up to 80% of these cases are as a result of PUJ obstruction. In paediatric patients it may also be found during investigation for other congenital abnormalities. Older children may present with loin pain associated with increased fluid intake, recurrent infection or pyelonephritis. In adults, chronic loin pain may also be associated with haematuria. Symptoms are often exacerbated by diuretics and high fluid intake [8].
References
1. Schiappacasse G, Aguirre J, Soffia P, et al. CT findings of the main pathological conditions associated with horseshoe kidneys. The British Journal of Radiology 2015;88(1045):20140456.
2. Kubihal V, Razik A, Sharma S, Das CJ. Unveiling the confusion in renal fusion anomalies: role of imaging. Abdominal Radiology 2021;46:4254-65.
3. Kirkpatrick J, Leslie S. Horseshoe kidney. StatPearls [Internet] 2022.
https://www.ncbi.nlm.nih.
gov/books/NBK431105/
4. Stein RJ, Desai MM. Management of urolithiasis in the congenitally abnormal kidney (horseshoe and ectopic). Current Opinion in Urology 2007;17(2):125-31.
5. Nemes B, Kanyári Z, Zádori G, et al. Horseshoe kidney transplantation. Interv Med Appl Sci 2015;7(2):85-9.
6. Philo D. Horseshoe kidney in conjunction with autosomal dominant polycystic kidney disease: a case report. Journal of Diagnostic Medical Sonography 2021;37(3):298-303.
7. Leibovich BC, Blute ML, Cheville JC, et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer: Interdisciplinary International Journal of the American Cancer Society 2003;97(7):1663‑71.
8. Al Aaraj MS, Badreldin AM. Ureteropelvic junction obstruction. StatPearls [Internet] 2022.
https://www.ncbi.nlm.nih.gov/books/
NBK560740/#:~:text=Ureteropelvic%
20junction%20obstruction%20(UPJO)
%20is,loss%20of%20the%20affected%20kidney.
All links last accessed June 2023.











