Case 1
A 64-year-old man presents to the haematuria clinic with visible haematuria, on a background of a 40 pack-year smoking history and family history of bowel cancer in his sister at the age of 48. A CT was performed as part of his investigations (Figure 1).

Figure 1.
- What kind of CT is shown here? Describe the different phases and their timing of acquisition.
- Describe the abnormality demonstrated on the CT, and possible differential diagnosis.
- What percentage of urothelial cancers do upper urinary tract urothelial cell carcinomas (UTUC) account for?
- Which non-urological hereditary conditions are associated with UTUC?
- Which other investigations might you undertake for this patient?
Case 2
The same patient underwent a diagnostic ureteroscopy, with the following image seen during the procedure.
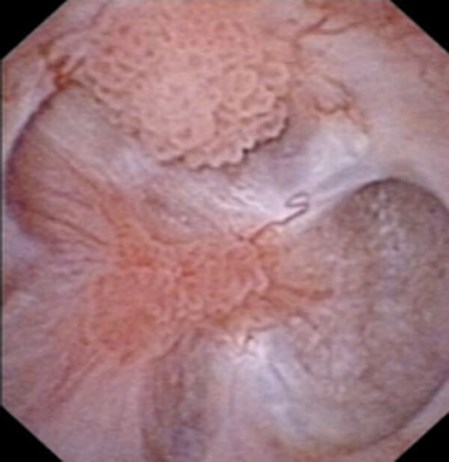
Figure 2.
- What does this image show?
- What proportion of UTUC are invasive at diagnosis?
- What factors are considered in risk-stratification of non-metastatic UTUC in order to guide management?
- Outline the treatment options for non-metastatic UTUC for low-risk and high-risk tumours respectively.
- What is the risk of urothelial cancer recurrence in the bladder and contralateral upper tract following radical nephroureterectomy for UTUC?
Acknowledgements:
Figure 1: Case courtesy of Dr Michael P Hartung, Radiopaedia.org, rID: 78377.
Figure 2: Reprinted from: Matin SF, Palou J. Chapter 4. Management of Low-Risk Disease: Endoscopy, Topical Therapy, Kidney-Preserving Surgery, and Surveillance. In: Upper Tract Urothelial Carcinoma. A Joint SIU-ICUD International Consultation. Shariat SF, Matin S, Stenzl A [eds.]. Vancouver, Canada. 8-12 September 2013: page 148. Available at:
https://www.siu-urology.org/themes/web/assets/
files/ICUD/pdf/utuc.pdf
Reproduced with permission from the Société Internationale d’Urologie (SIU) and the International Consultation on Urological Diseases (ICUD).
Upper urinary tract urothelial cell carcinoma: answers
Case 1
- This is a CT urography (CTU), or CT intravenous urogram (CT-IVU). Most CTU protocols consists of three phases; non-contrast, enhanced / nephrographic, and a delayed / excretory phase. The non-contrast phase is performed prior to contrast administration, the enhanced phase is taken 90-100 seconds after contrast administration and the delayed phase is taken 5-15 minutes after contrast has been given.
- The delayed phase of this CT has demonstrated a filling defect in the left renal pelvis, raising suspicions of UTUC. Other common differential diagnosis includes centrally located renal cancer, benign tumours (e.g. fibroepithelial polyps, nephrogenic adenomas), papillary necrosis, and blood clot.
- 5-10% of all urothelial cancers are in the upper tract.
- Patients with Lynch syndrome, also known as hereditary nonpolyposis colorectal carcinomas (HNPCC), are at risk of developing UTUC.
- Cystoscopy to ensure there is no concurrent bladder cancer. Urinary cytology may be helpful in diagnosing high-grade tumours. Where imaging and cytology alone are not certain, diagnostic ureteroscopy should be performed to allow direct visualisation of the upper tract and tumour, with subsequent biopsy.
Case 2
- There are multifocal papillary lesions, suggestive of UTUC.
- Approximately two-thirds of patients with UTUC have invasive disease at diagnosis.
- The European Association of Urology (EAU) guidelines recommend that the following factors should be considered when risk stratifying patients into low or high-risk tumours groups; low-risk: unifocal disease, tumour size <2cm, low grade cytology / ureteroscopic biopsy, and no evidence of tumour invasion on CTU; high-risk: multifocal disease, tumour size >2cm, high-grade cytology/ureteroscopic biopsy, presence of hydronephrosis, previous radical cystectomy for high-grade bladder cancer, and variant histology.
- Low-risk disease: kidney-sparing surgery should be considered in all low-risk diseases. These include ureteroscopic ablation of tumours (using laser), segmental ureteral resection, and instillation of topical agents (such as BCG and mitomycin C) into the upper tract. High-risk disease: radical nephroureterectomy is the standard treatment within this group of patients. However, in patients with solitary kidney or impaired renal function, kidney-sparing options should be considered. Recent evidence (the POUT trial) suggests that gemcitabine-platinum combination adjuvant chemotherapy following nephroureterectomy for locally advanced disease (pT2-4 pN0-3 M0) improves disease-free survival.
- 22-47% in bladder, and 2-6% in the contralateral upper tract.








